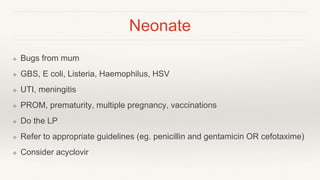
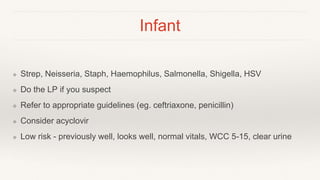
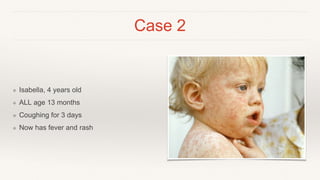
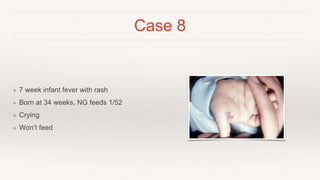
This document discusses the evaluation and management of fever in pediatric patients. It provides guidance on identifying potential infectious and non-infectious causes of fever based on age, considering factors like common bacterial and viral illnesses as well as environmental exposures. It also presents 8 case examples of pediatric patients presenting with fever and discusses appropriate diagnostic and treatment approaches based on each patient's age, symptoms, vital signs and risk factors.