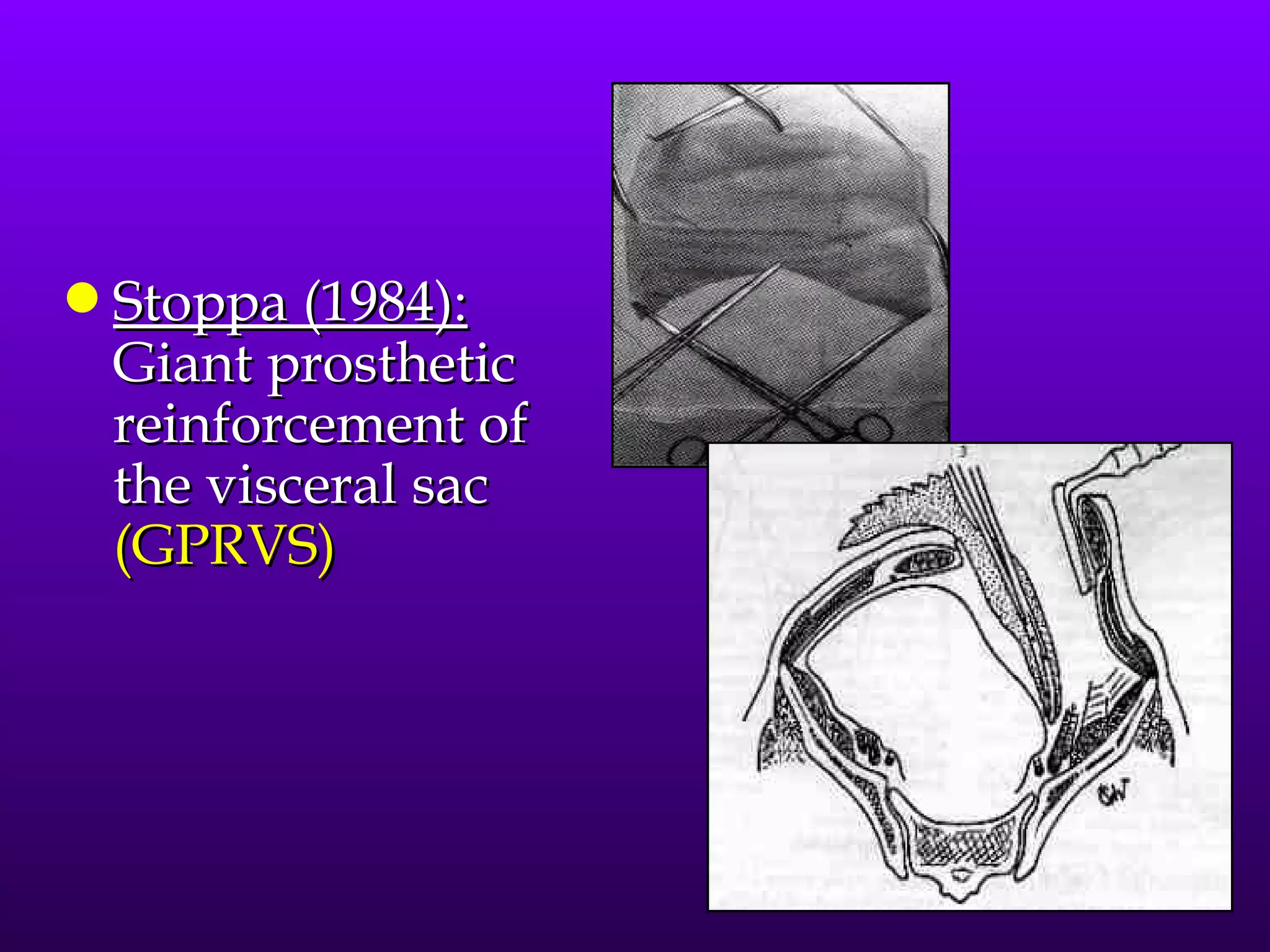
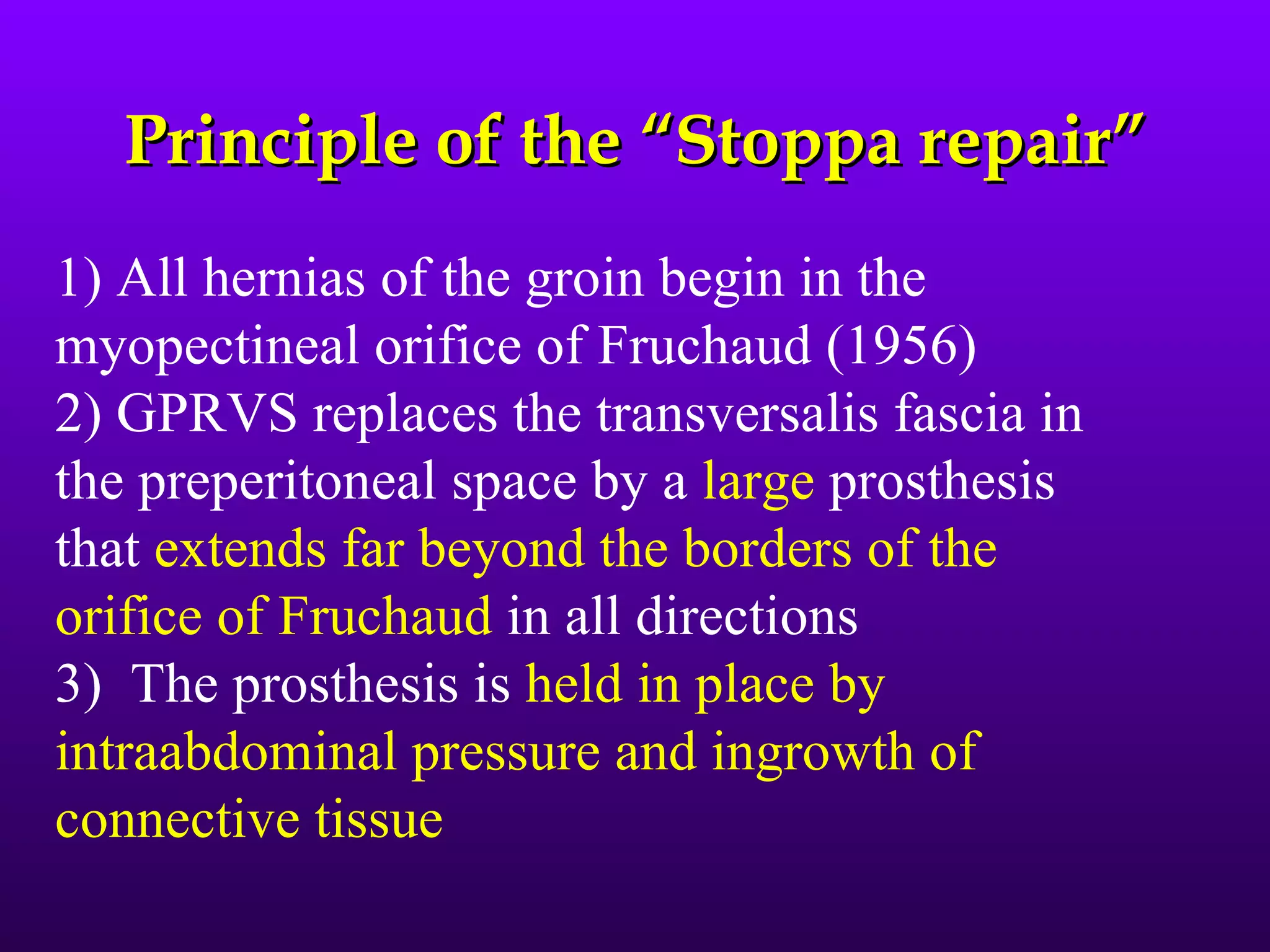
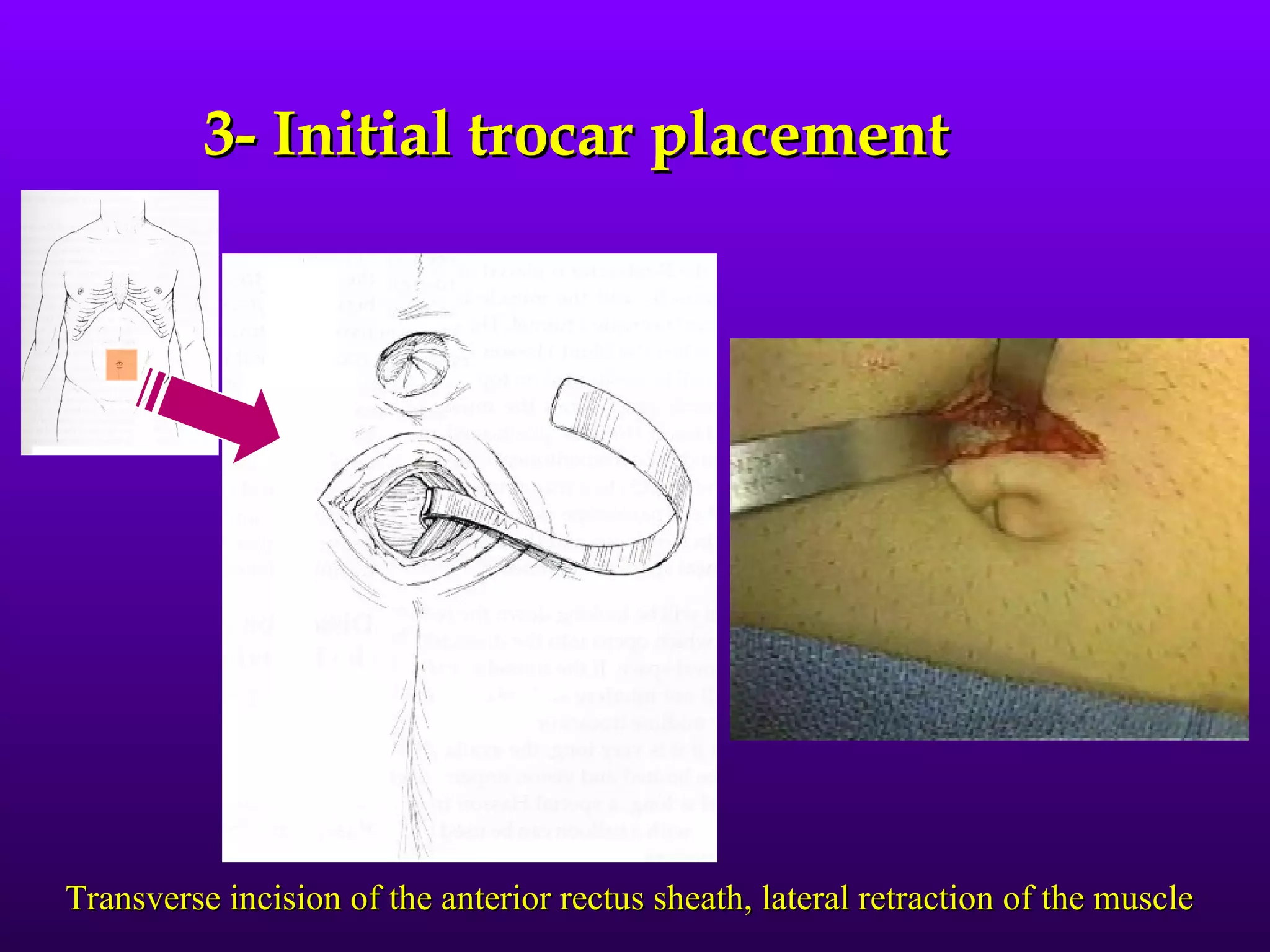
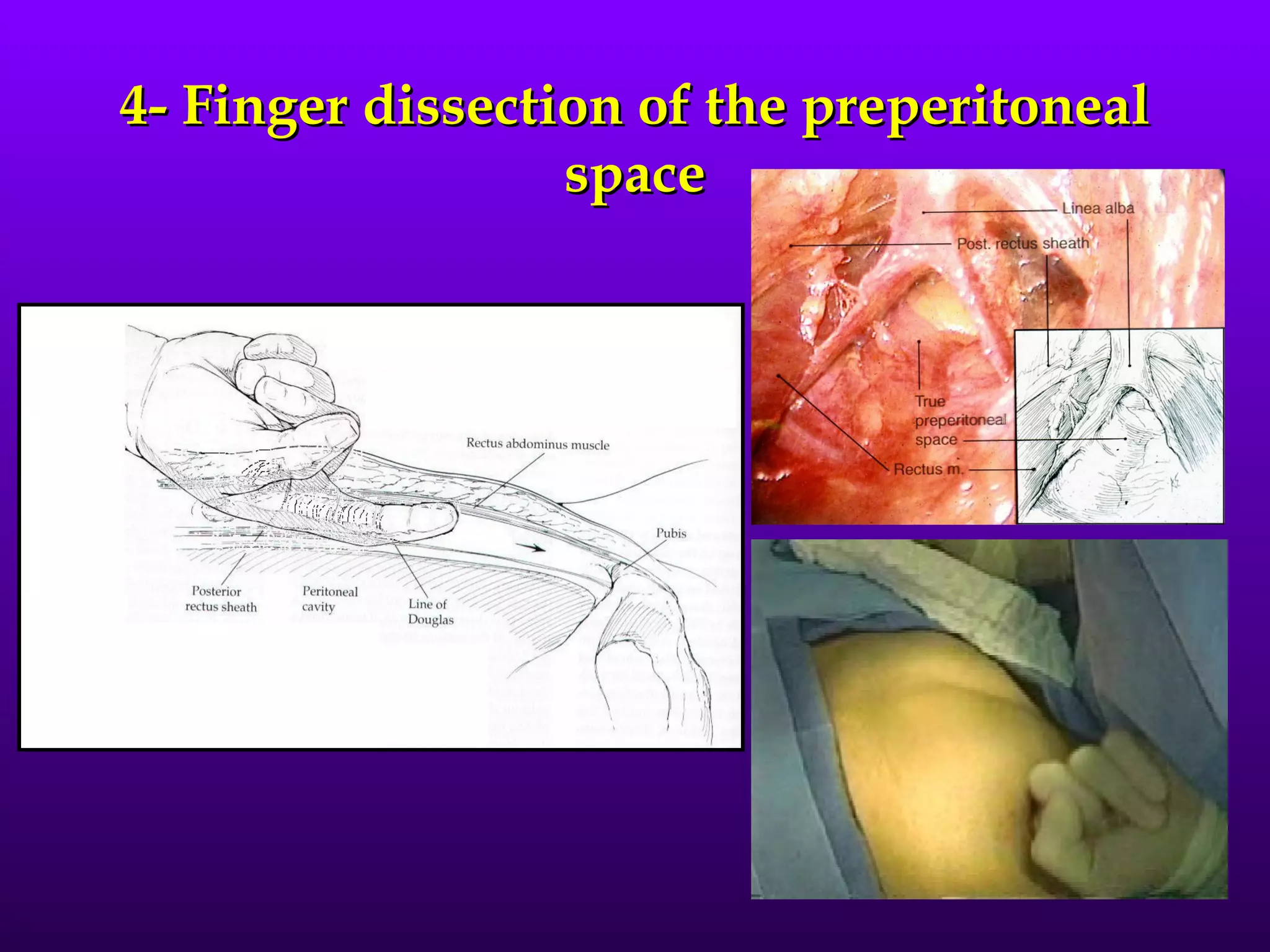
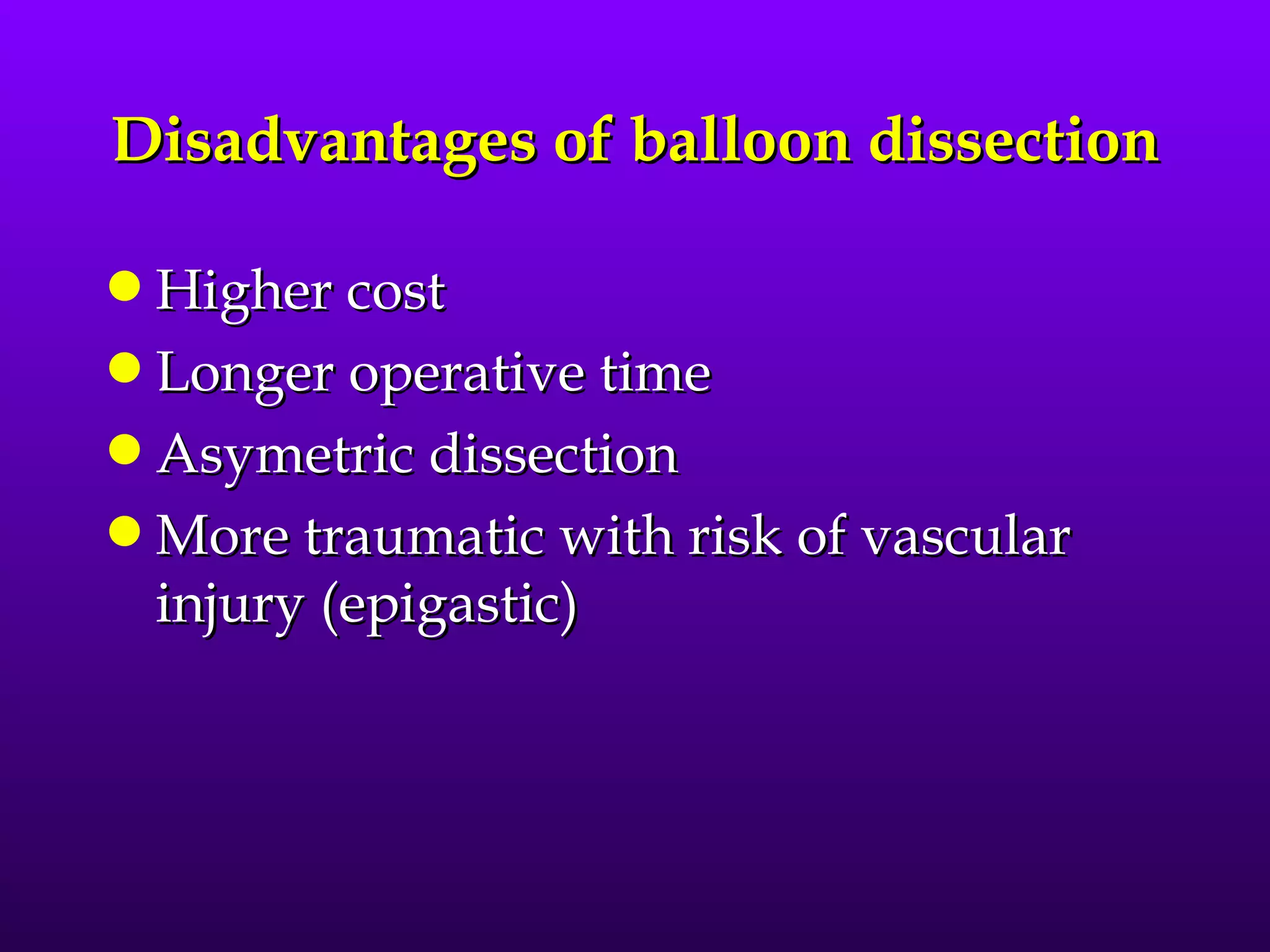
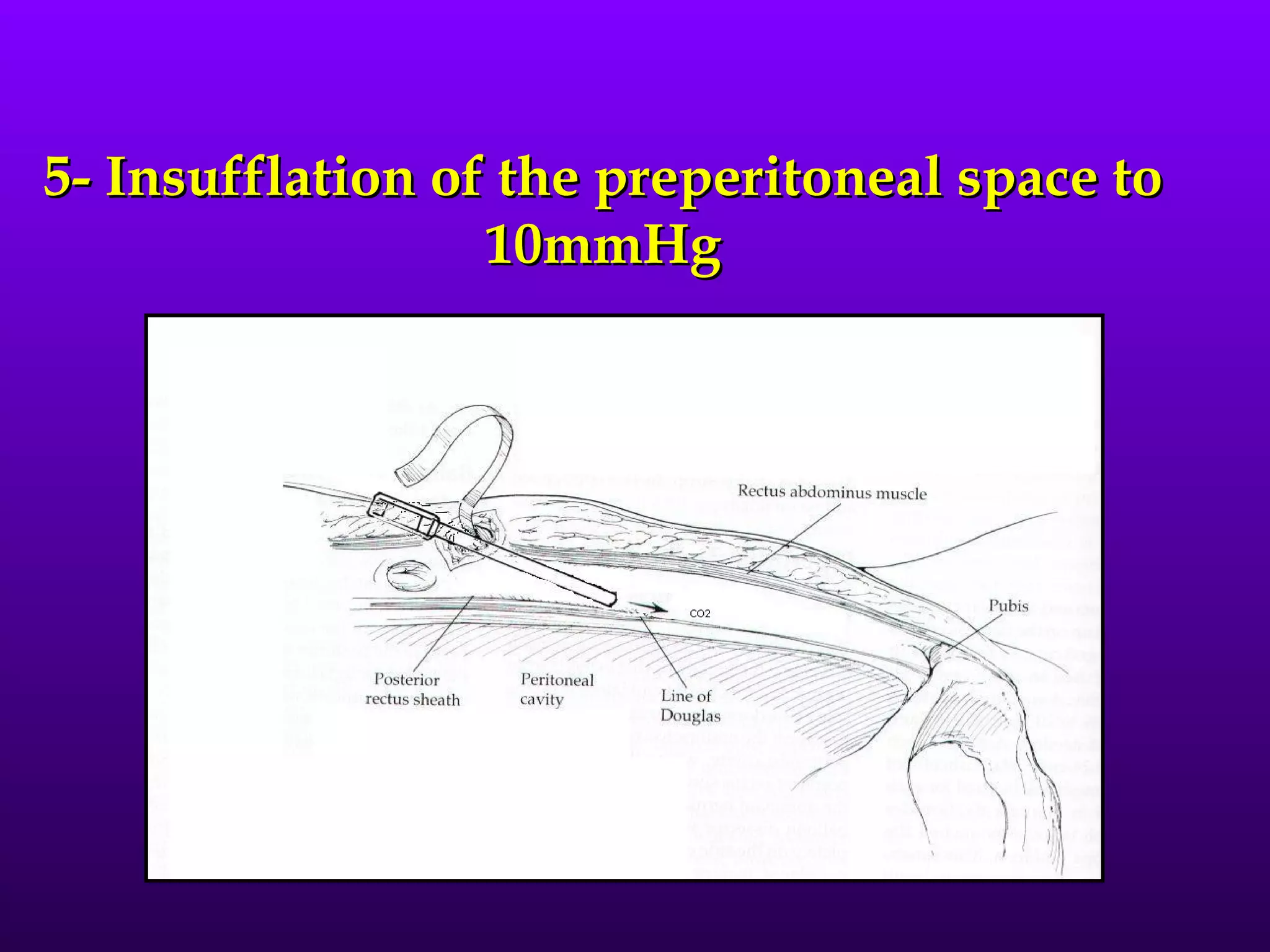
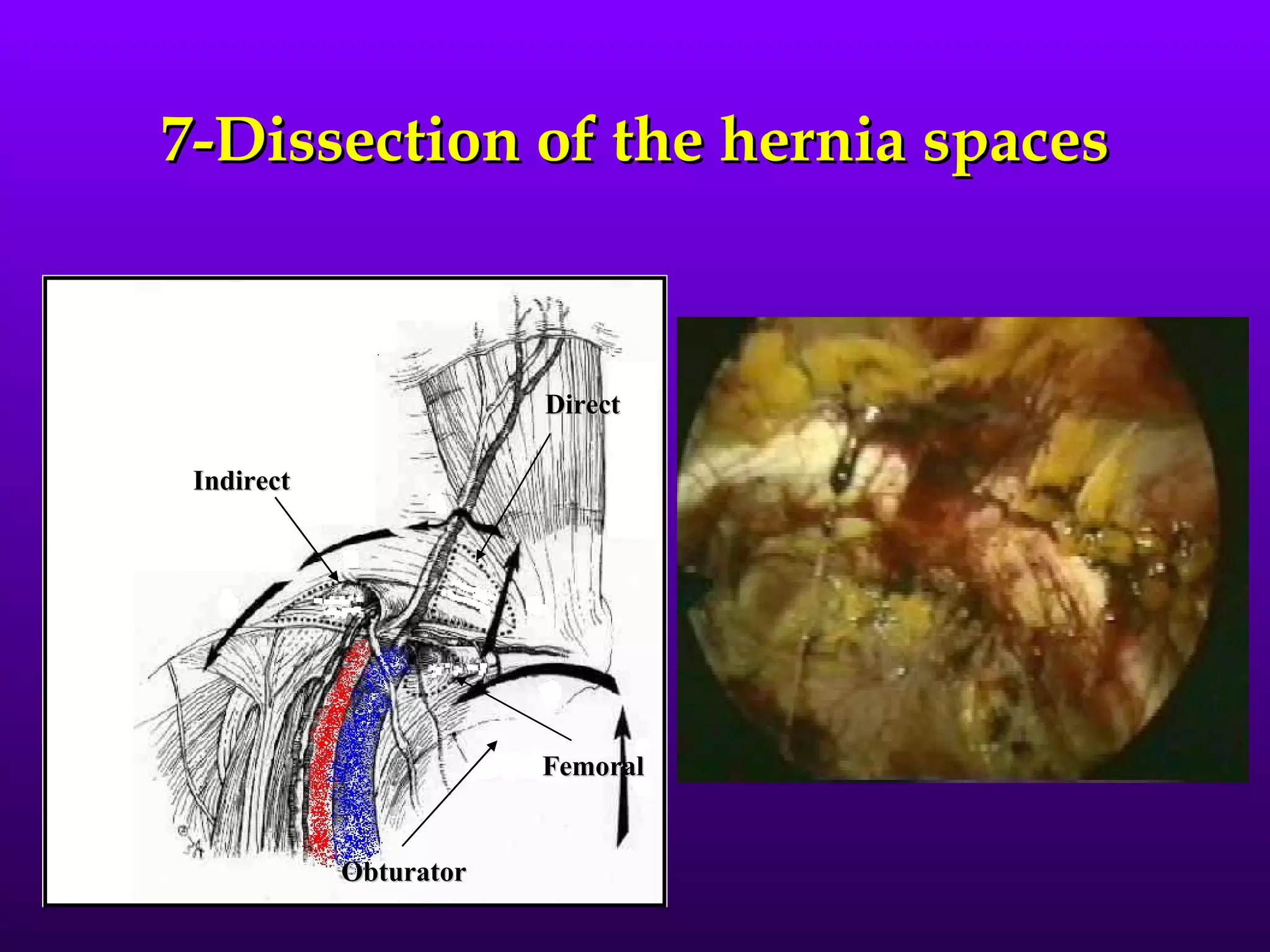
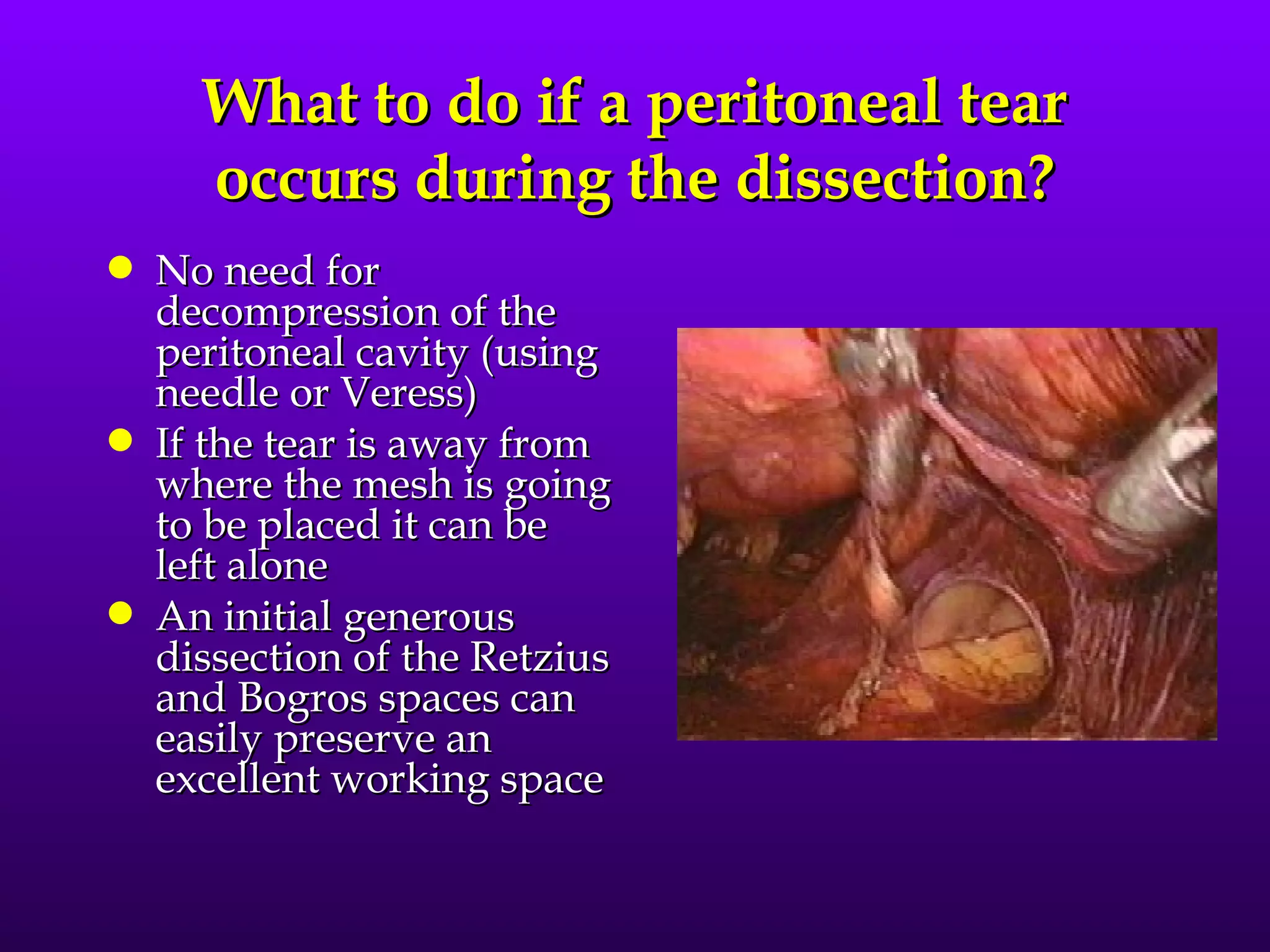
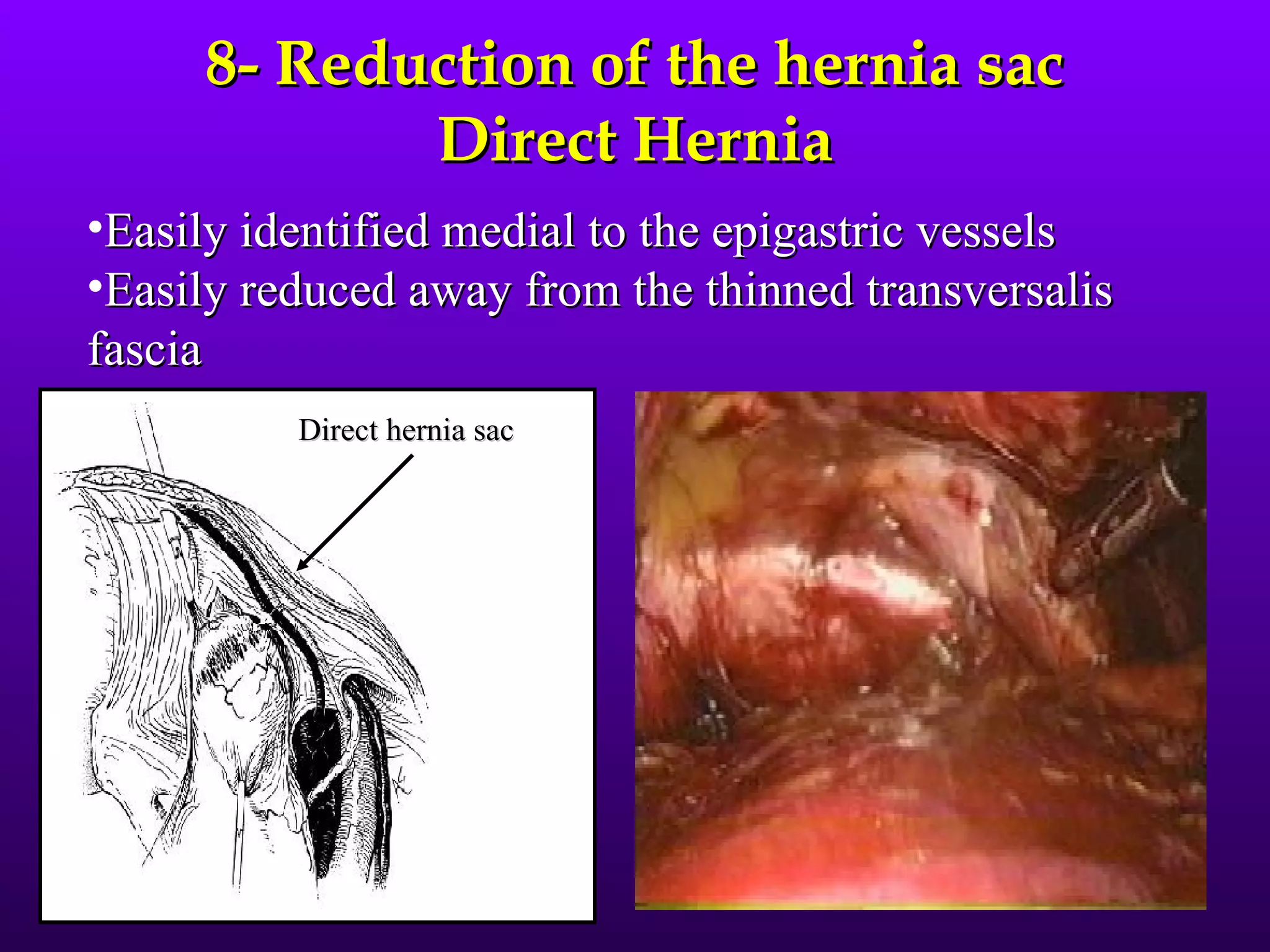
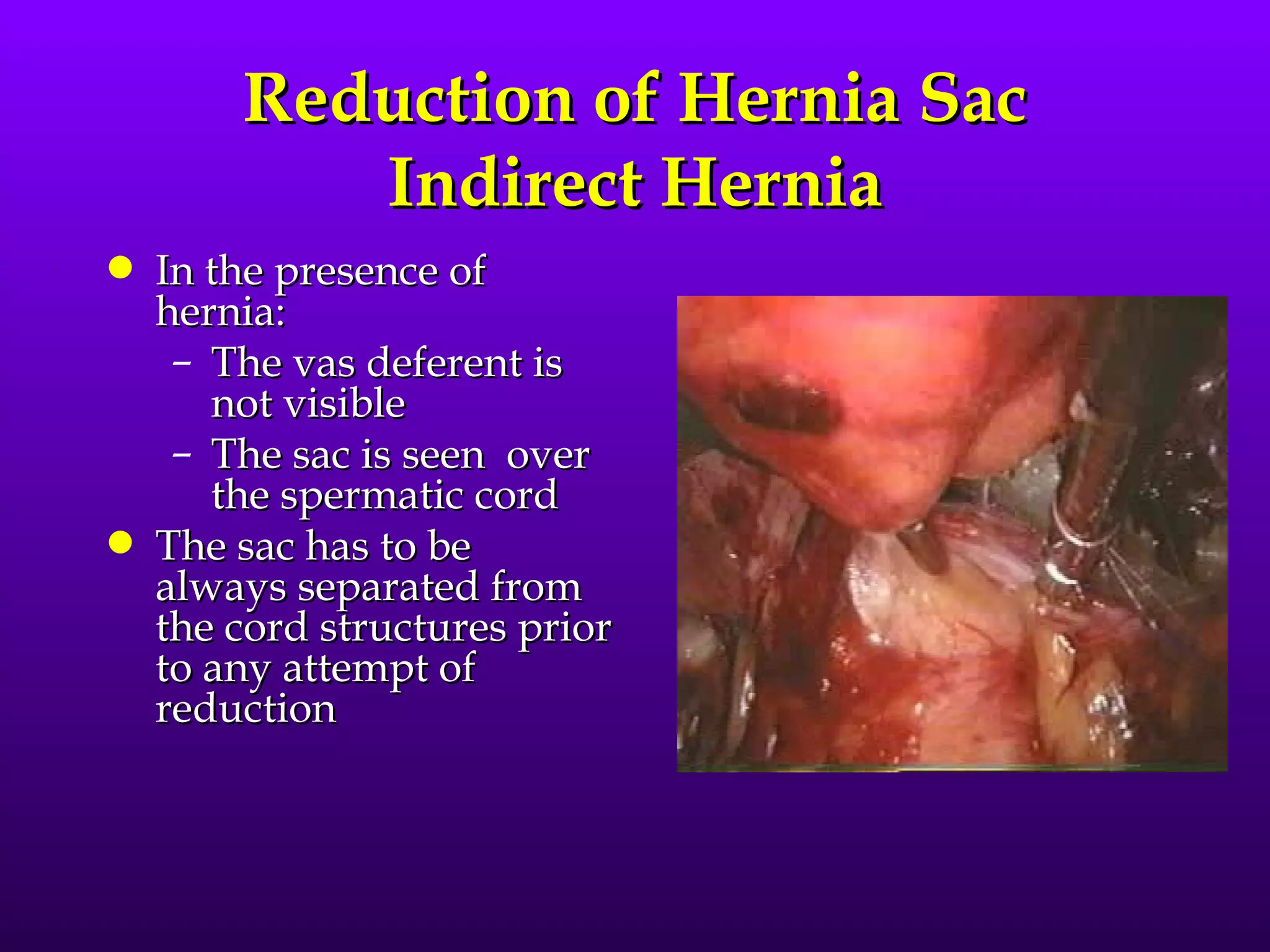
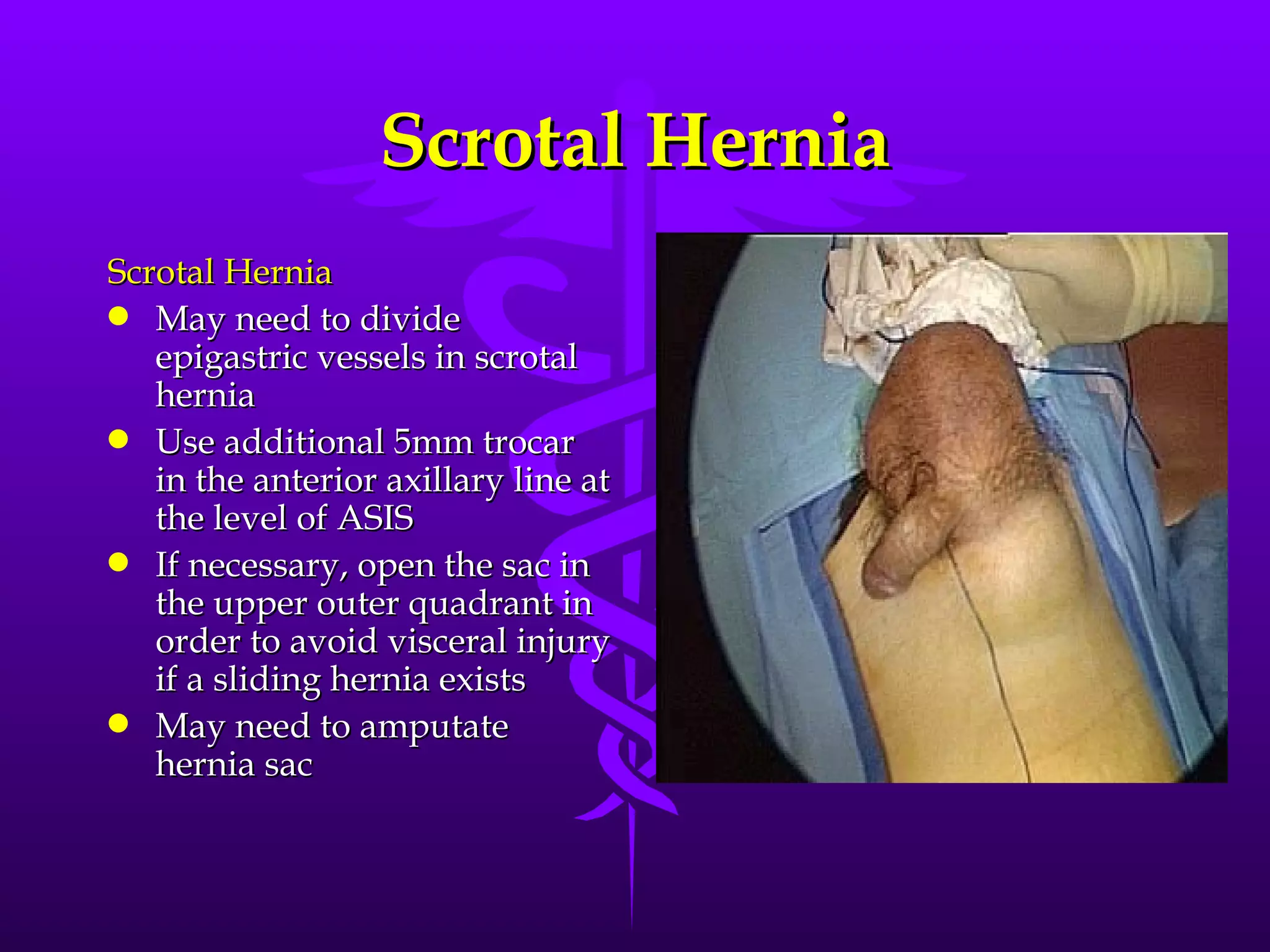
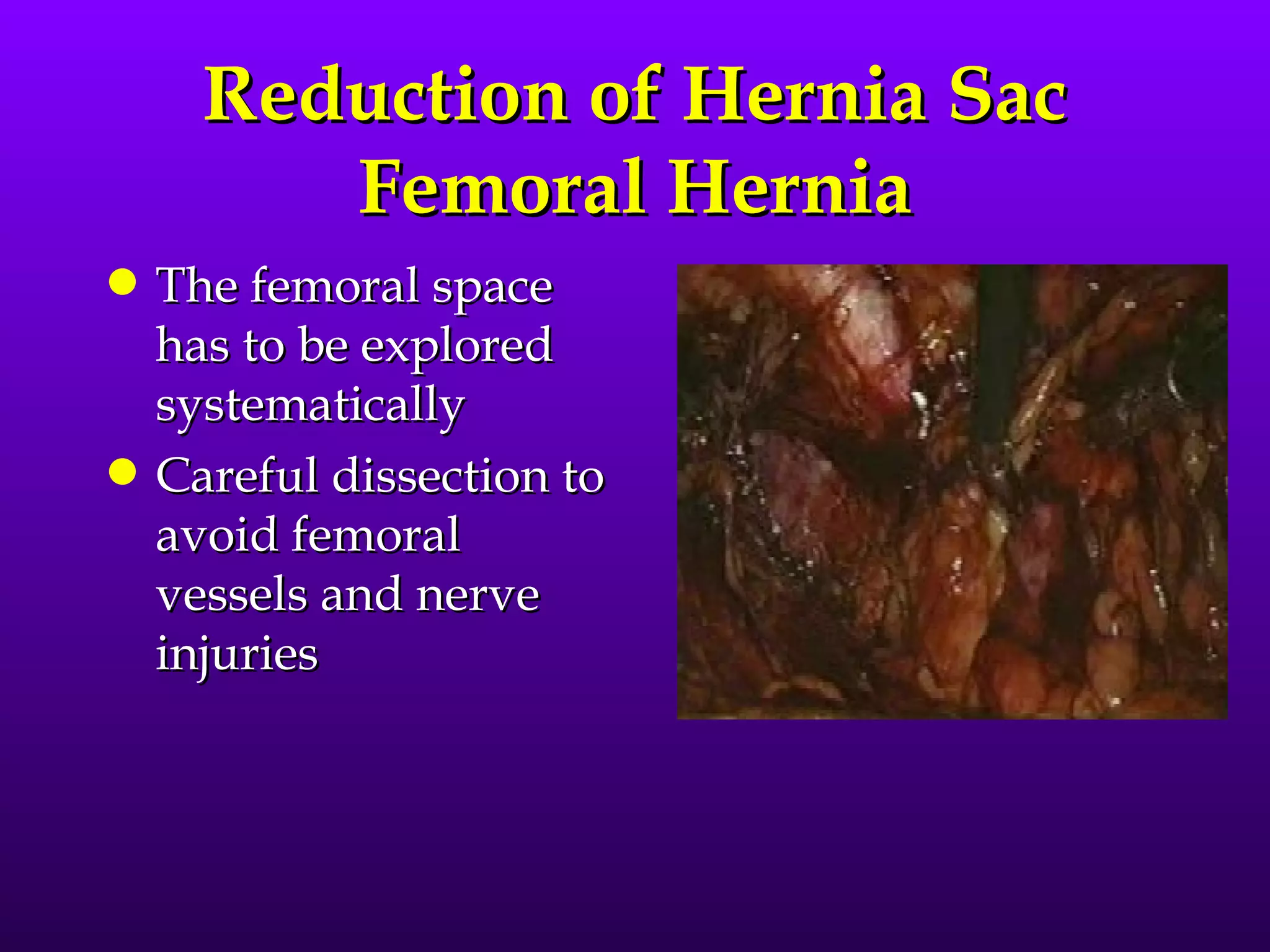
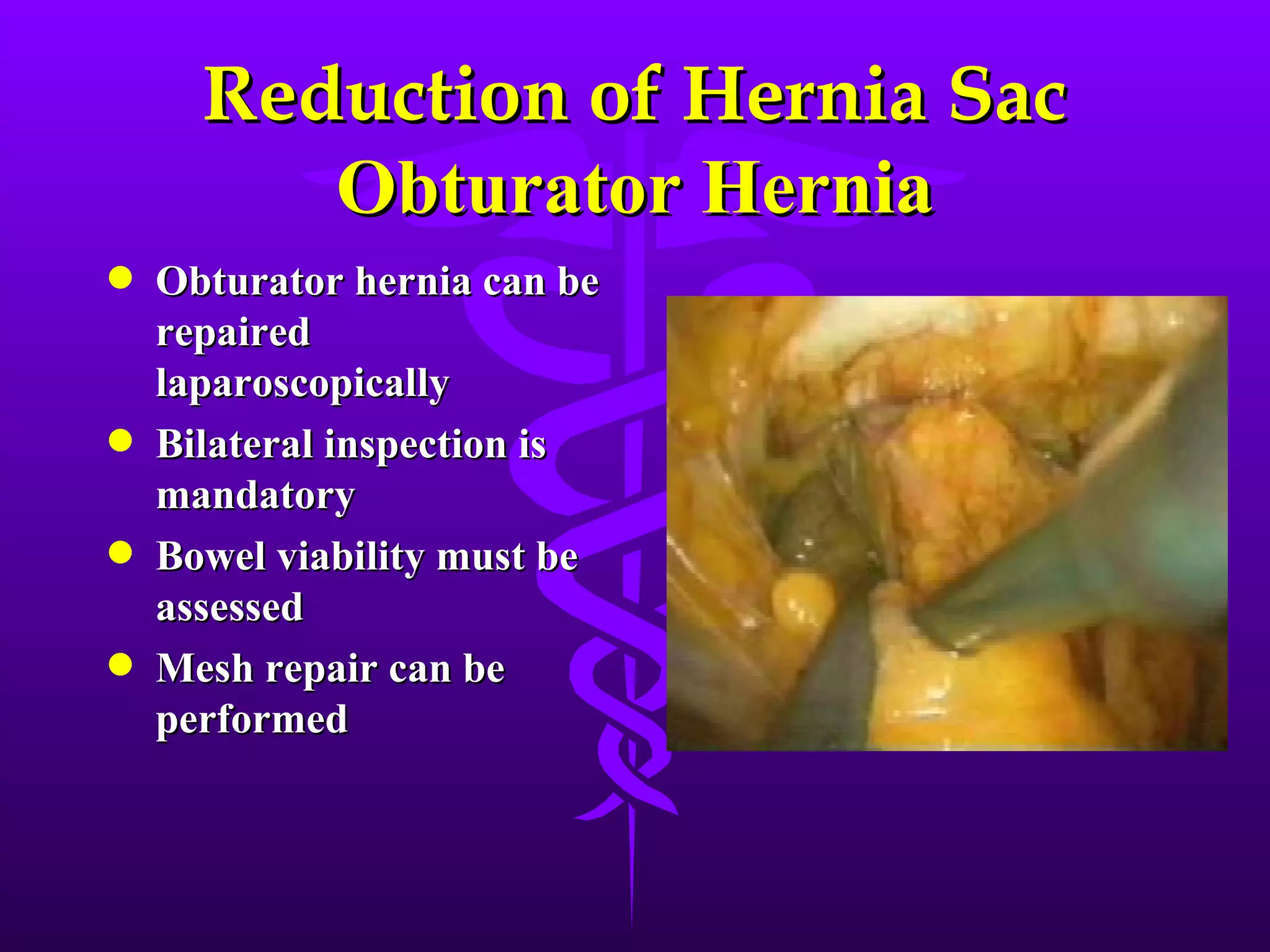
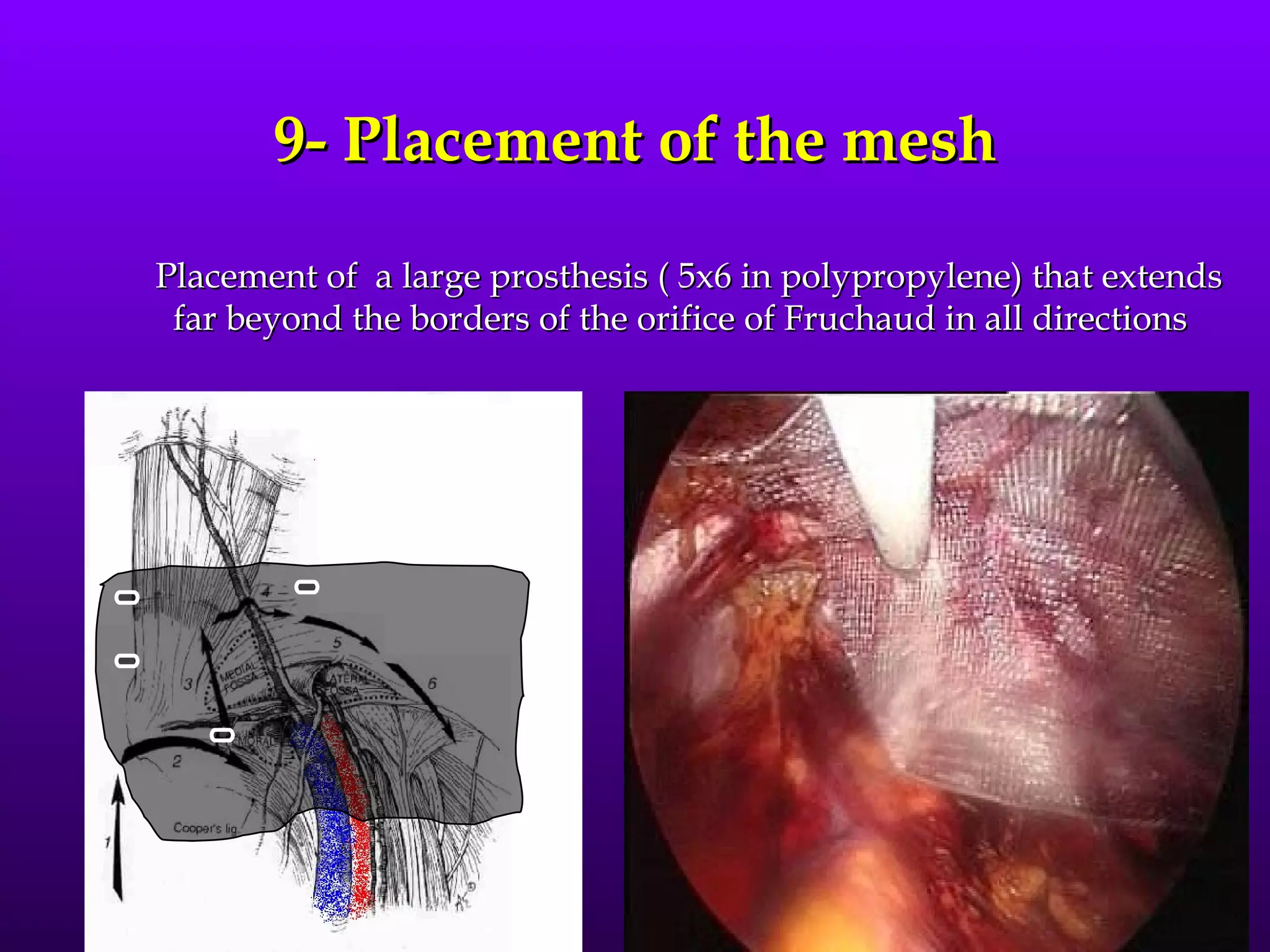
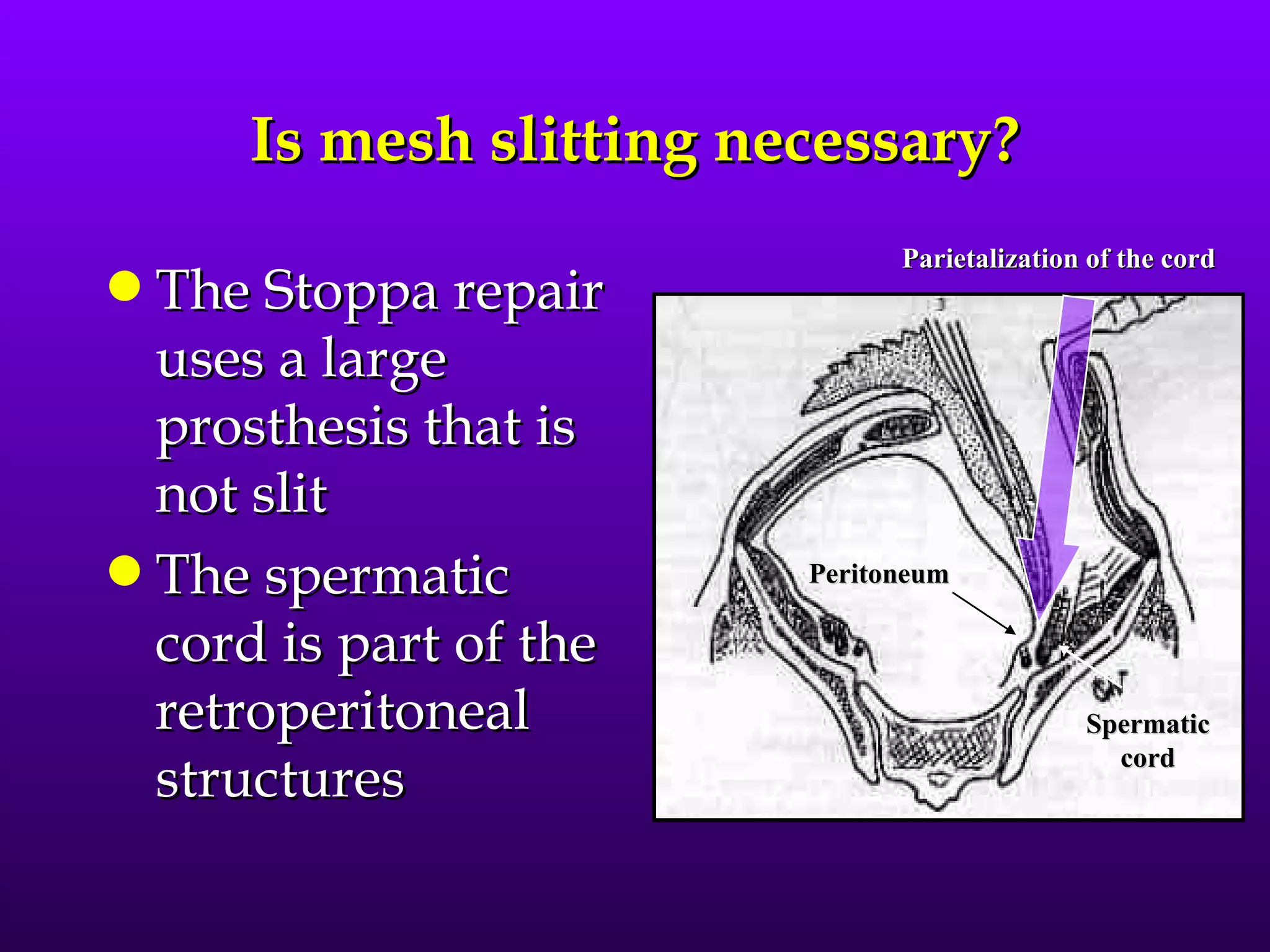
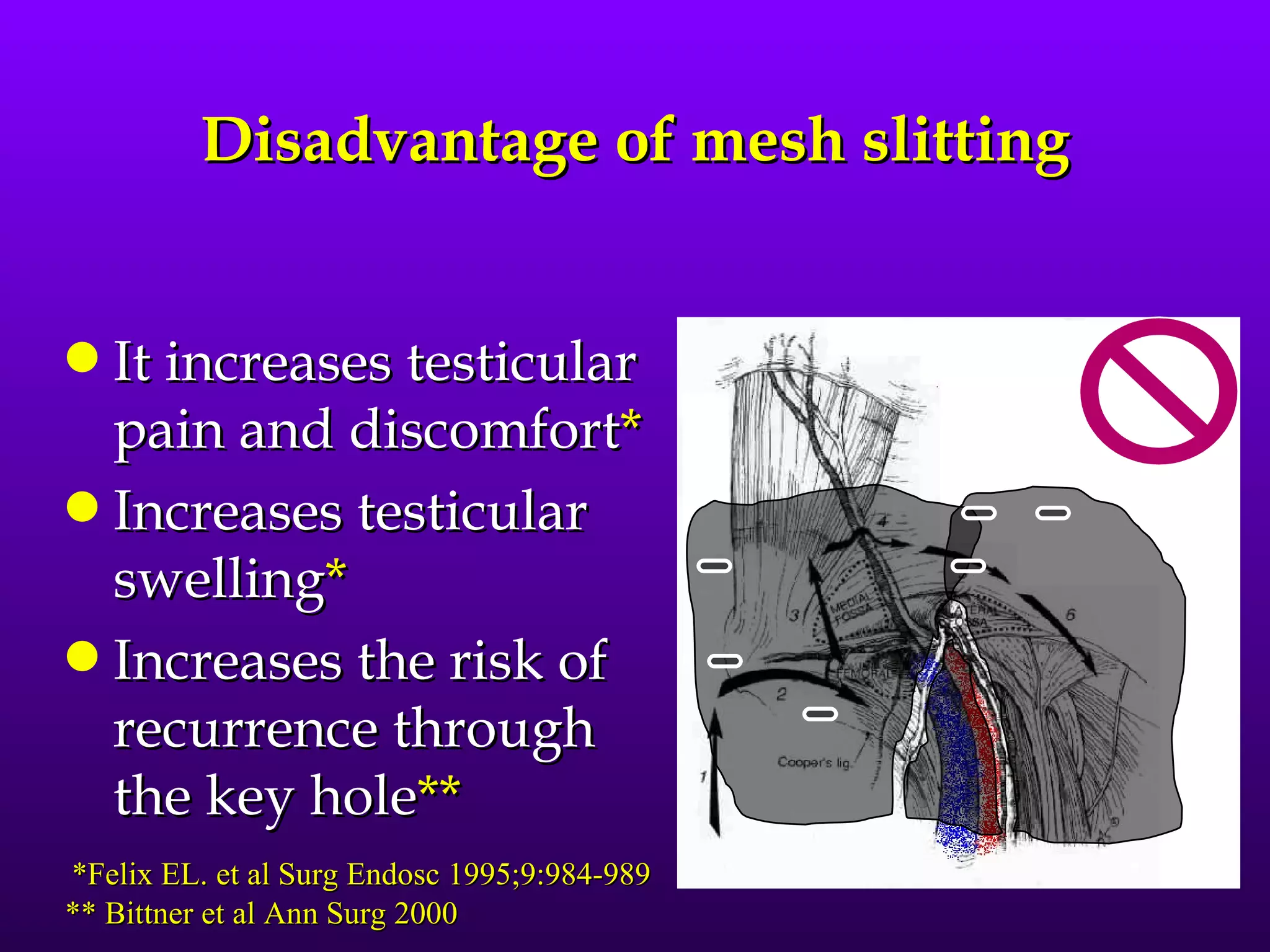
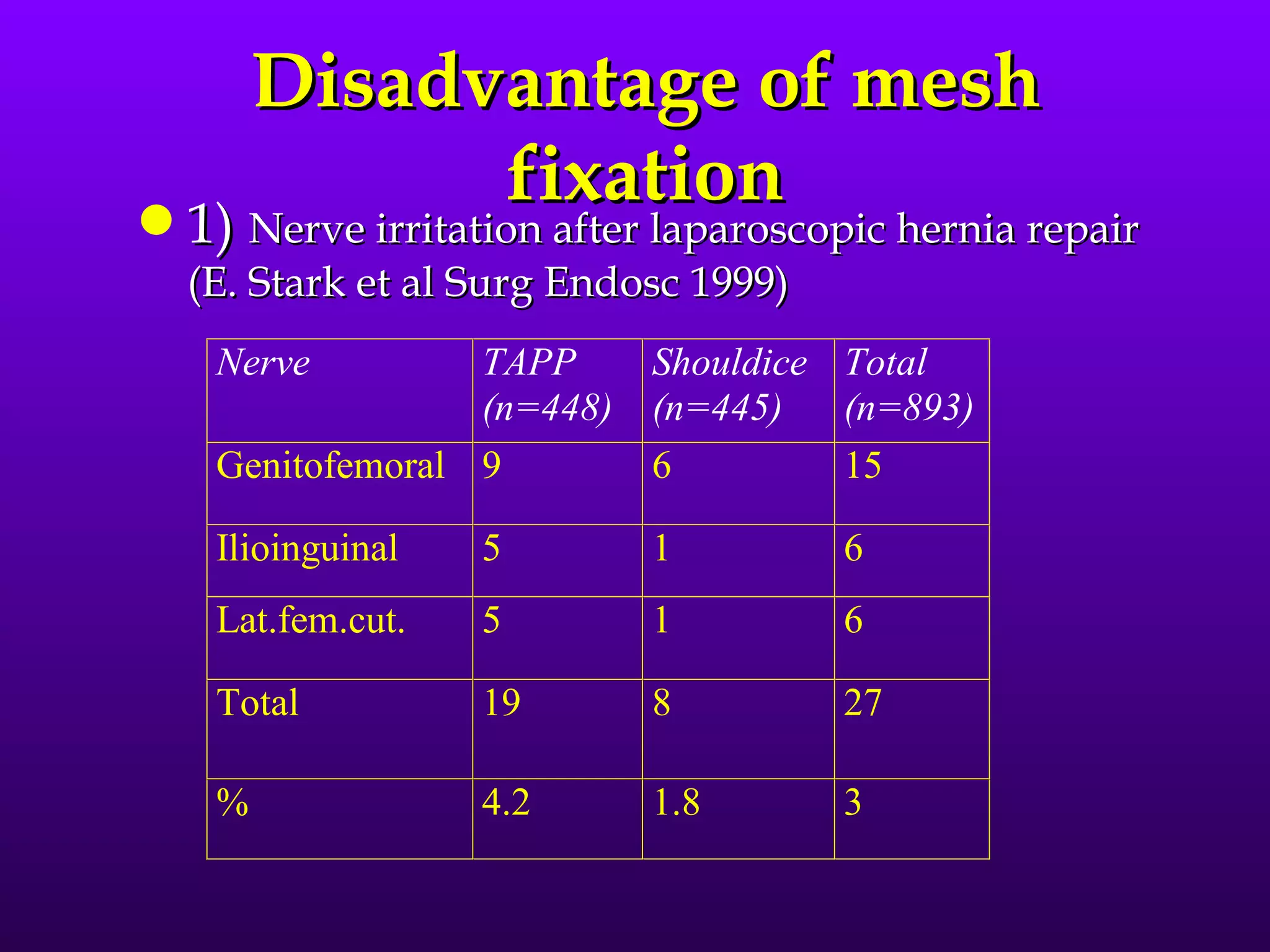
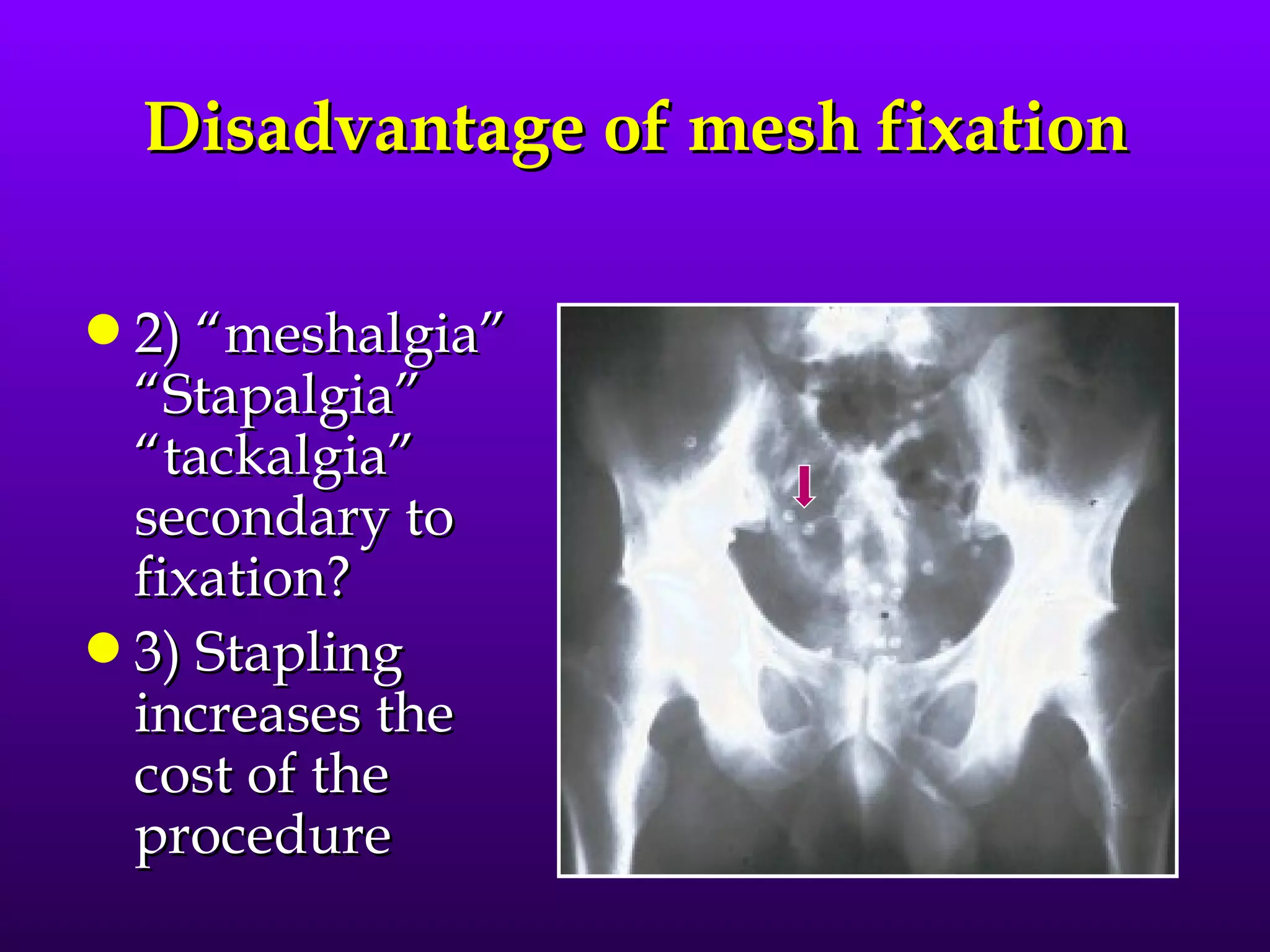
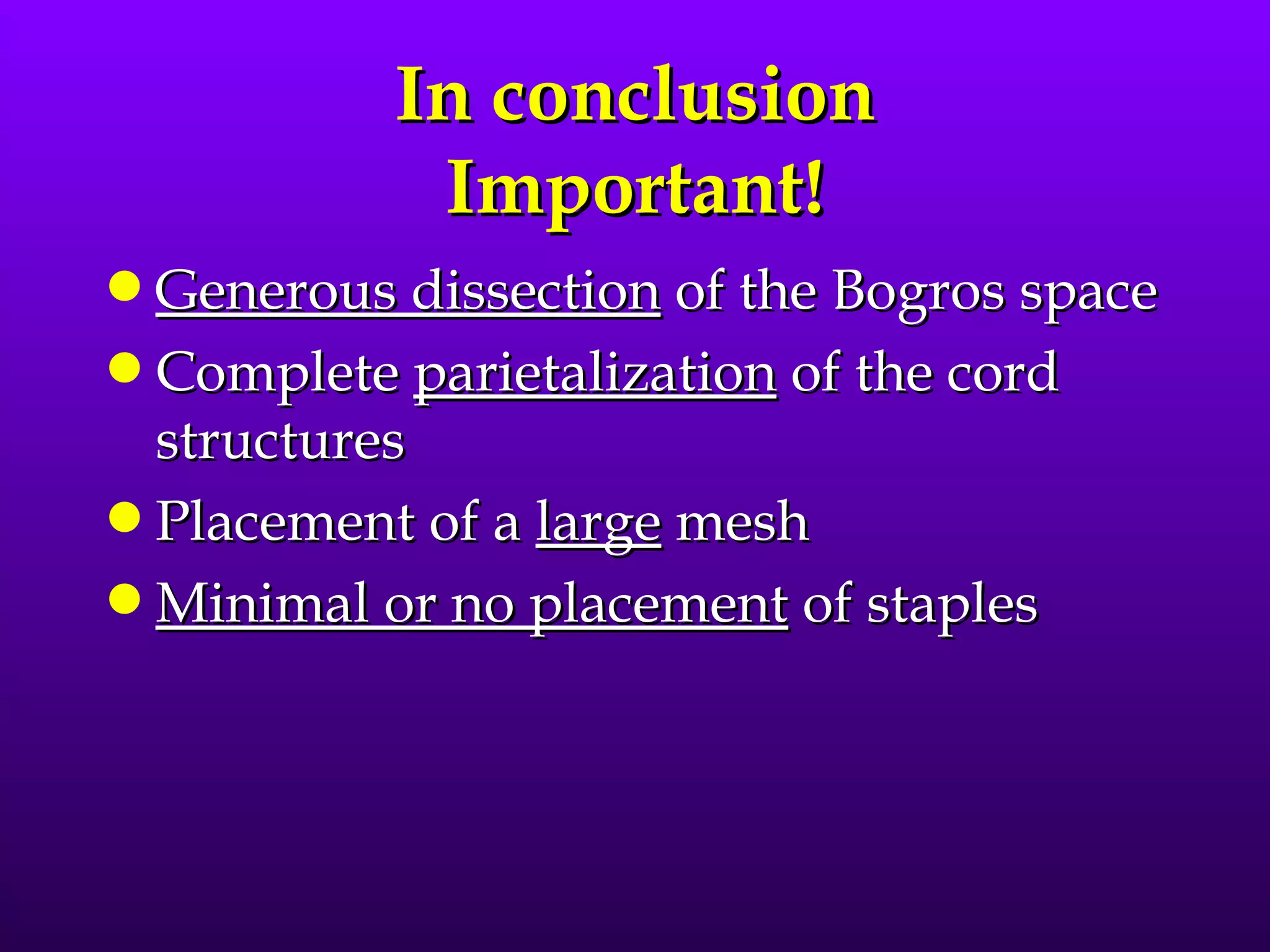
This document describes the technique of laparoscopic herniorrhaphy (TEP). It involves: 1) Dissecting the preperitoneal space to create working space; 2) Reducing any hernia sacs; 3) Placing a large mesh that extends beyond the hernia borders; 4) Optionally fixing the mesh with minimal staples. The goal is to reproduce the open 'Stoppa repair' technique laparoscopically using a large mesh with wide coverage and minimal fixation to reduce risks of nerve injury, pain, and recurrence."