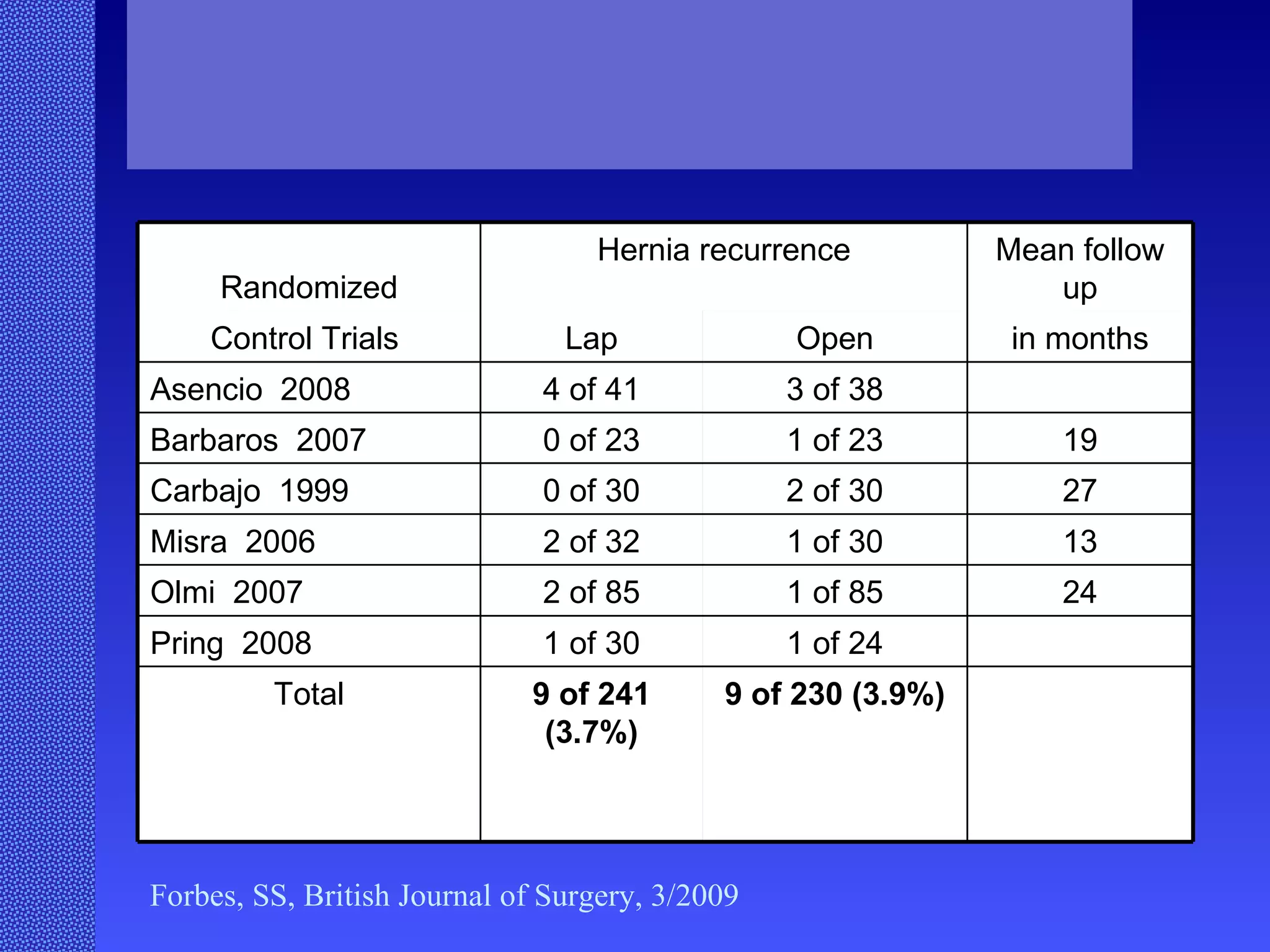
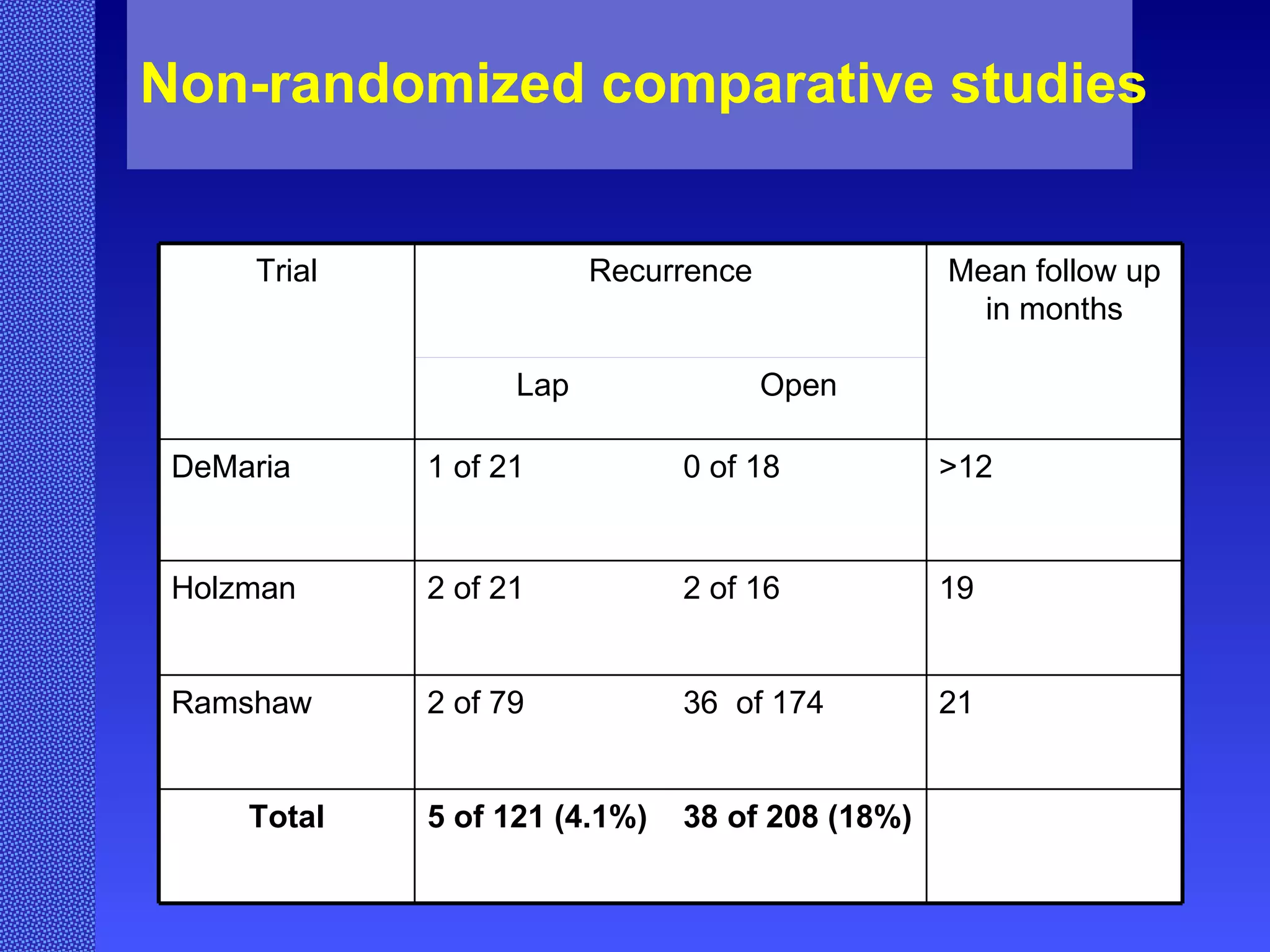
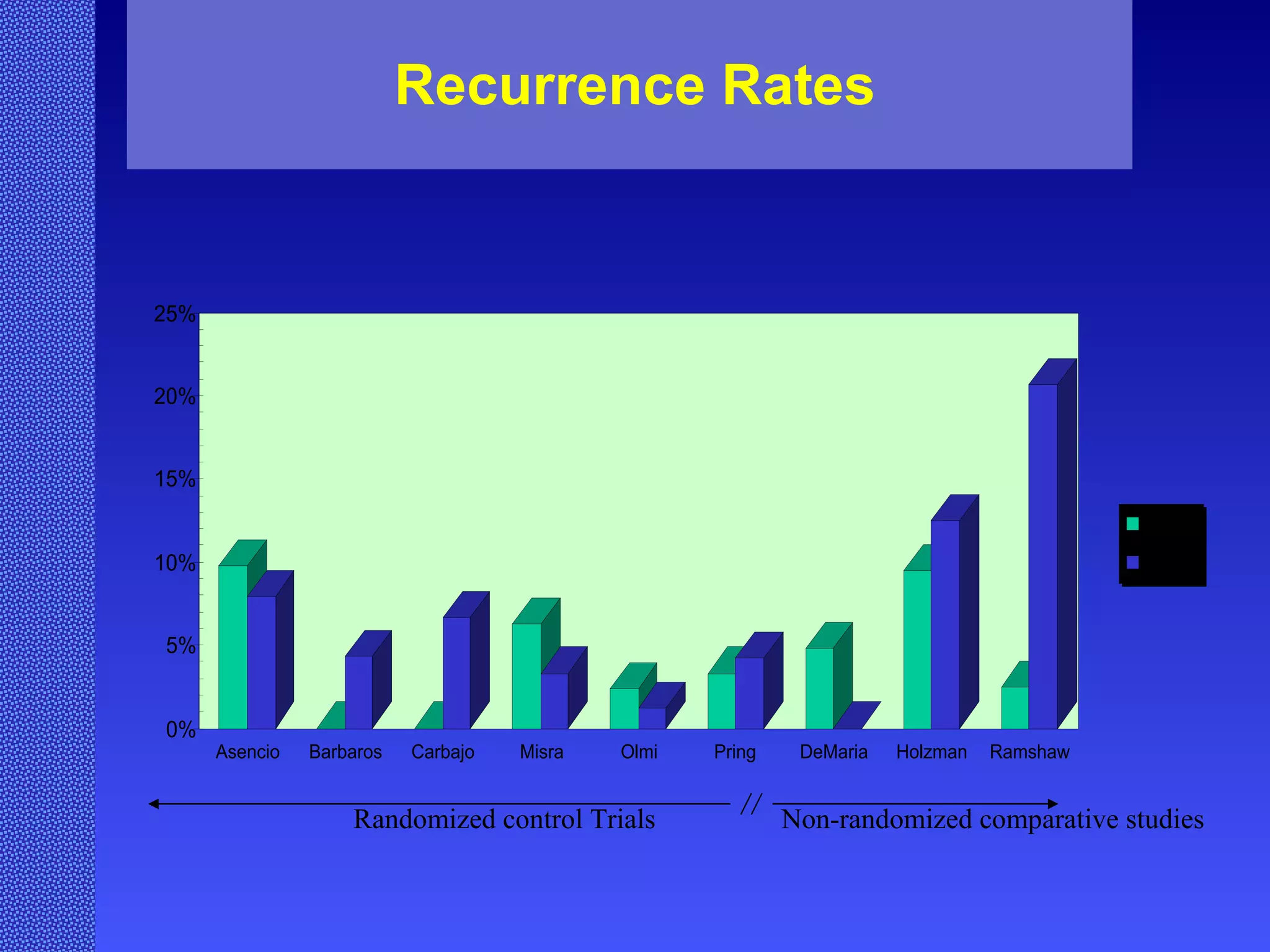
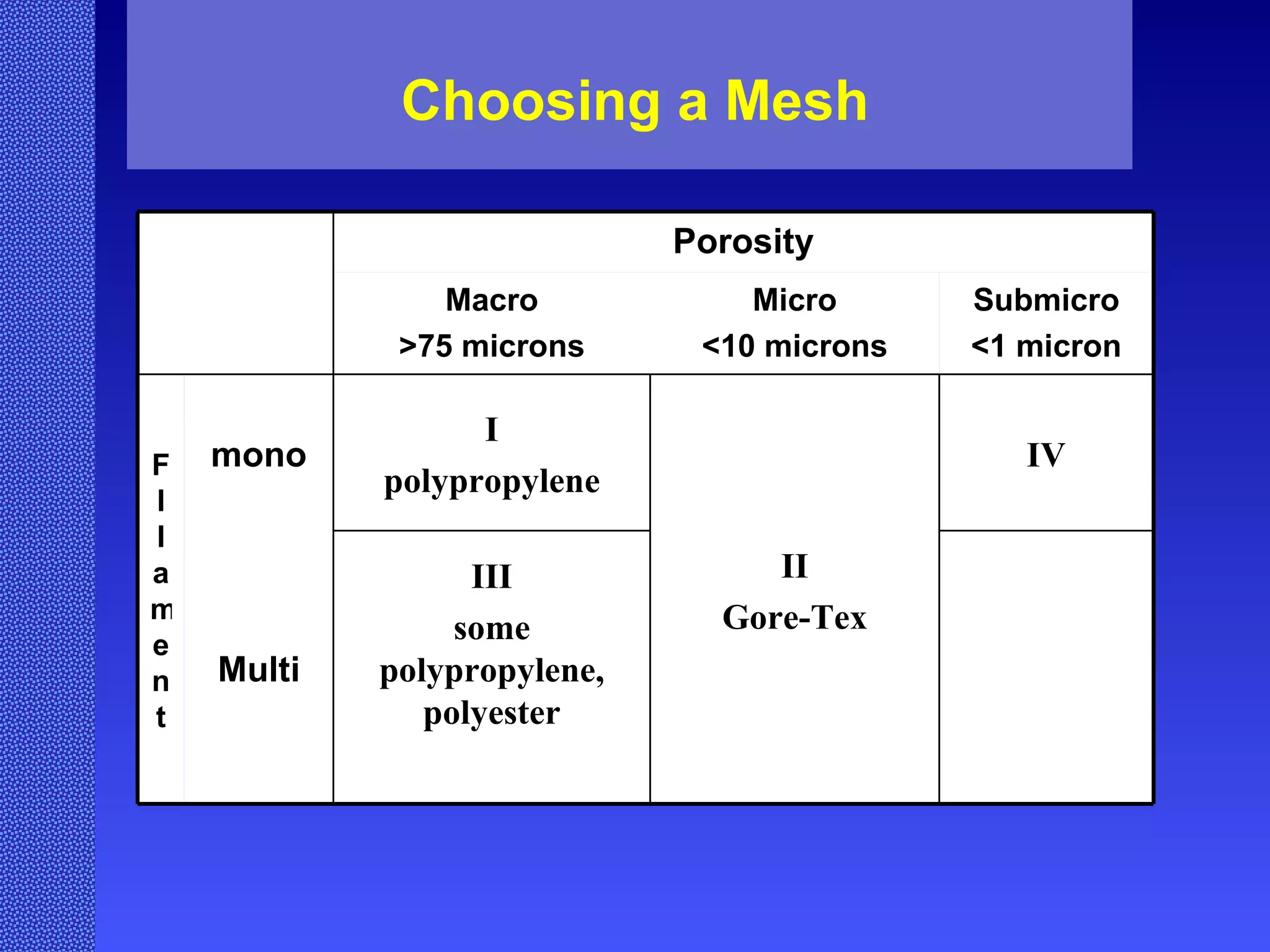
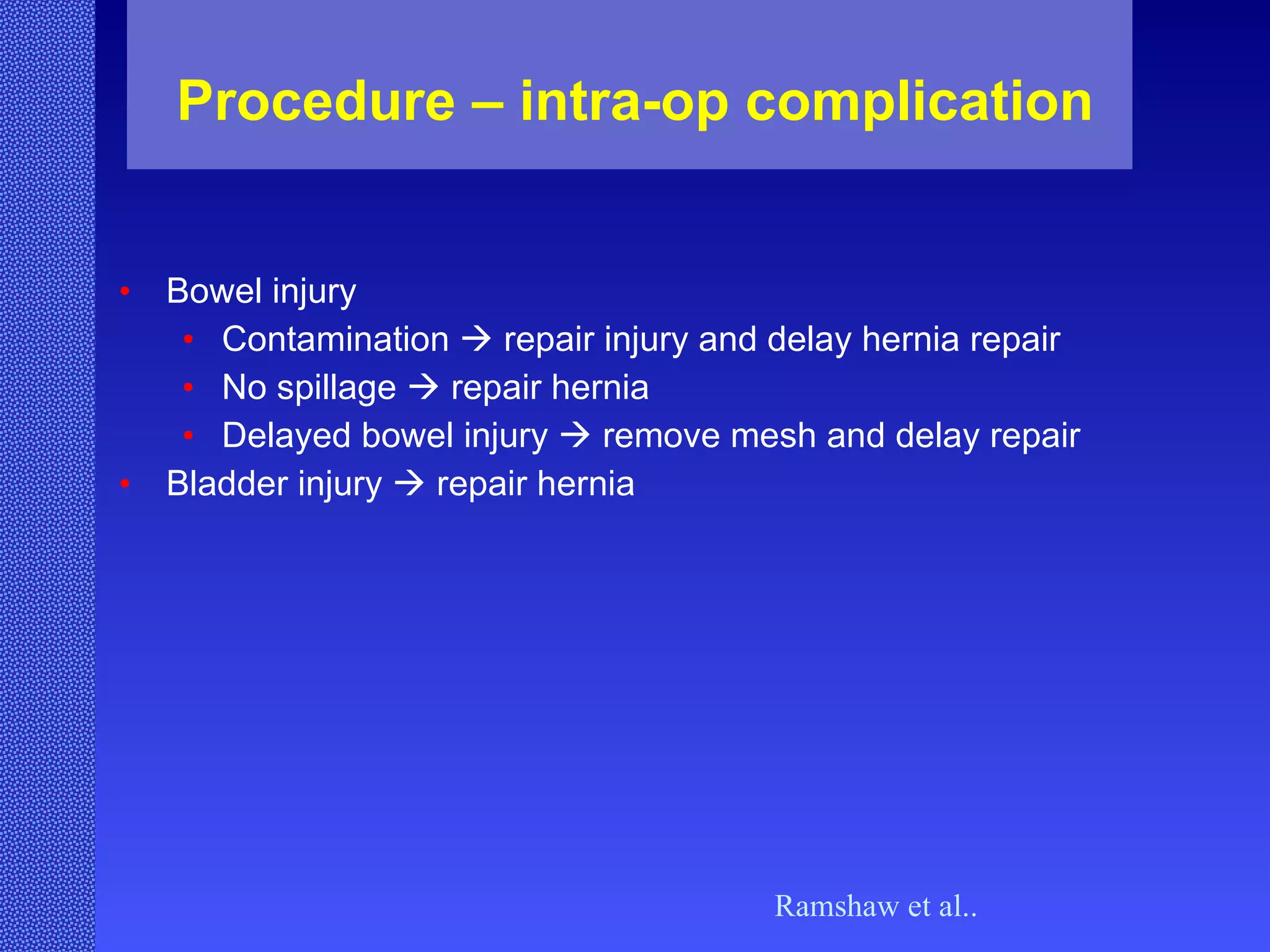
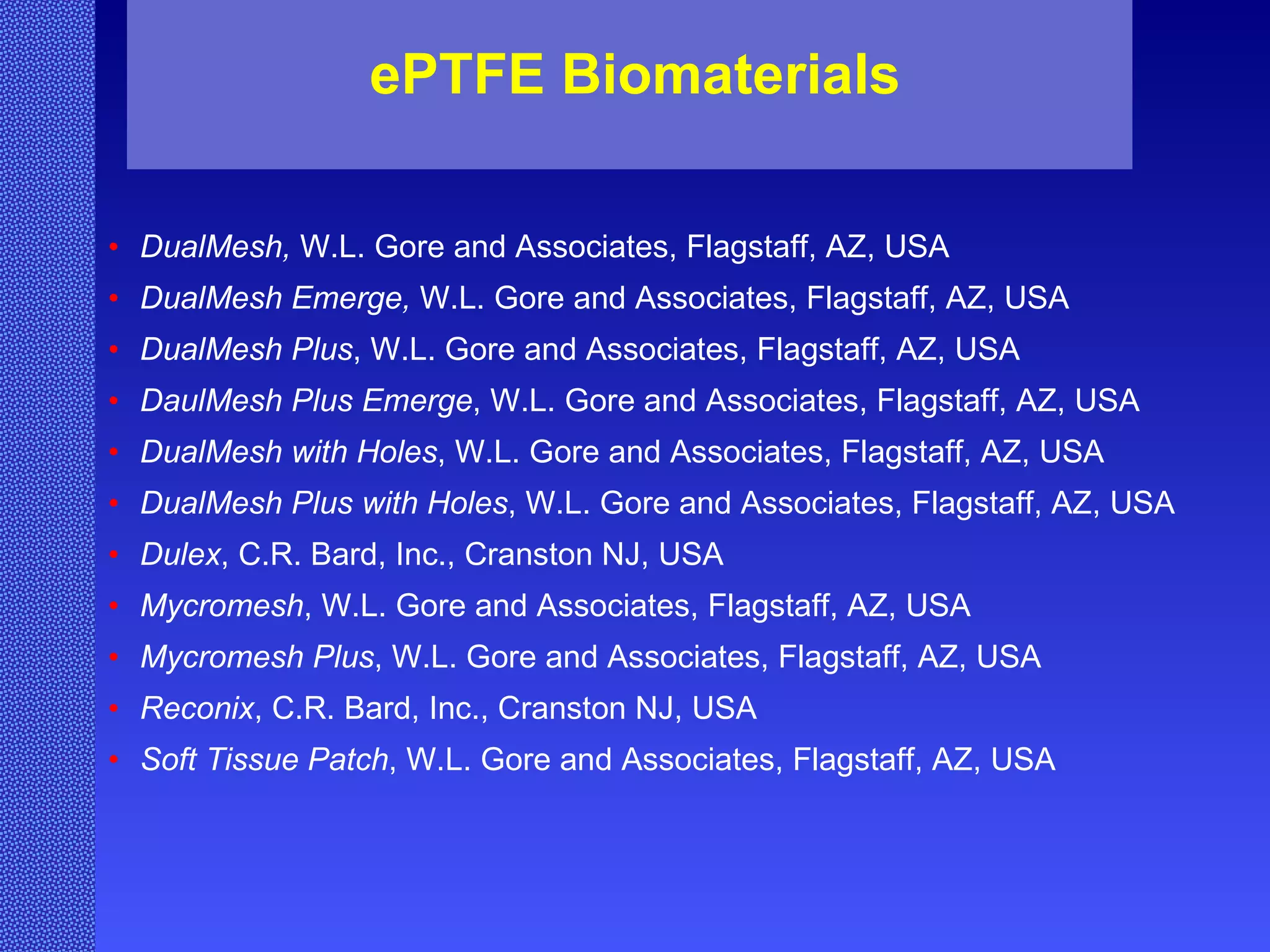
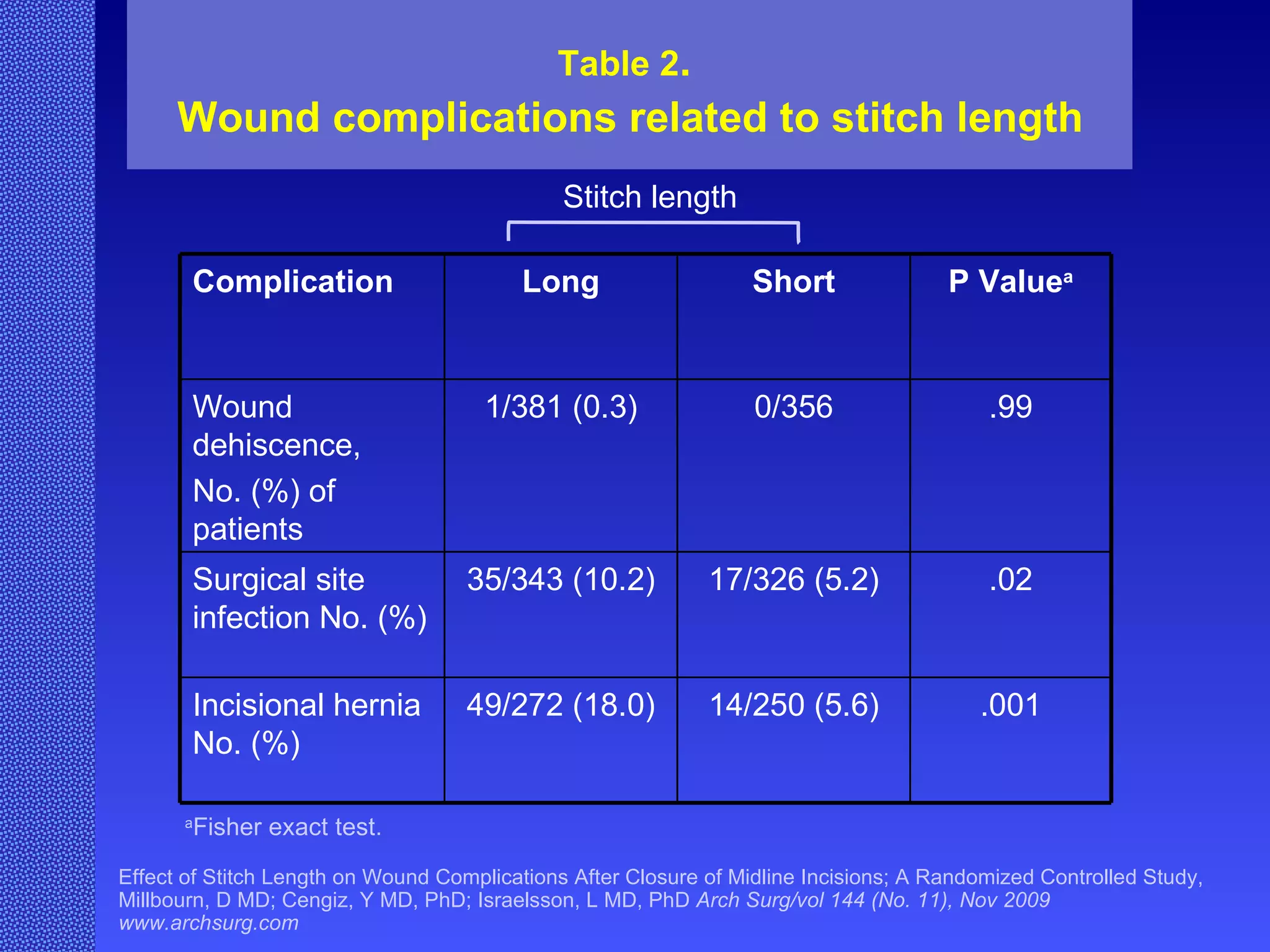
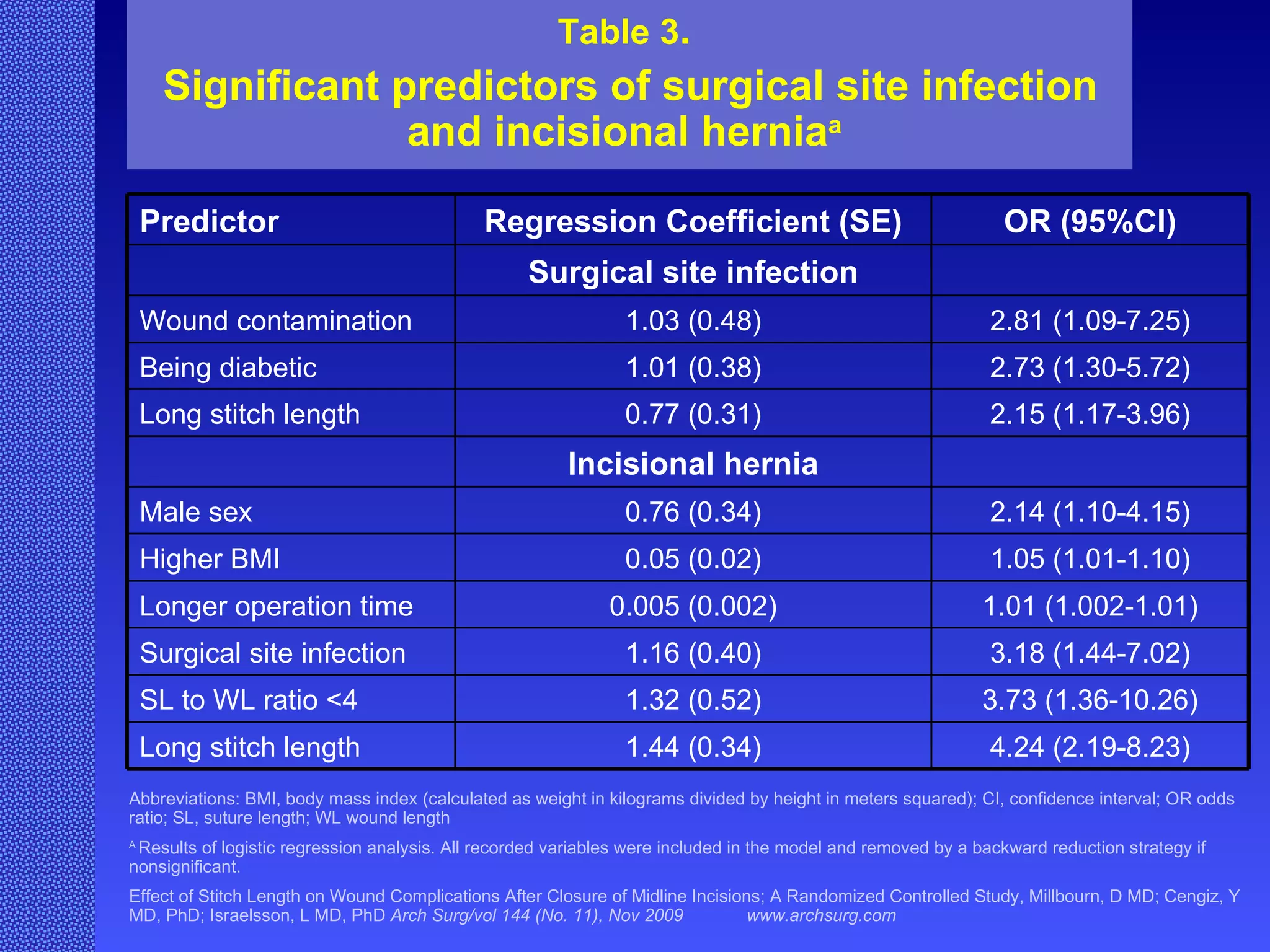
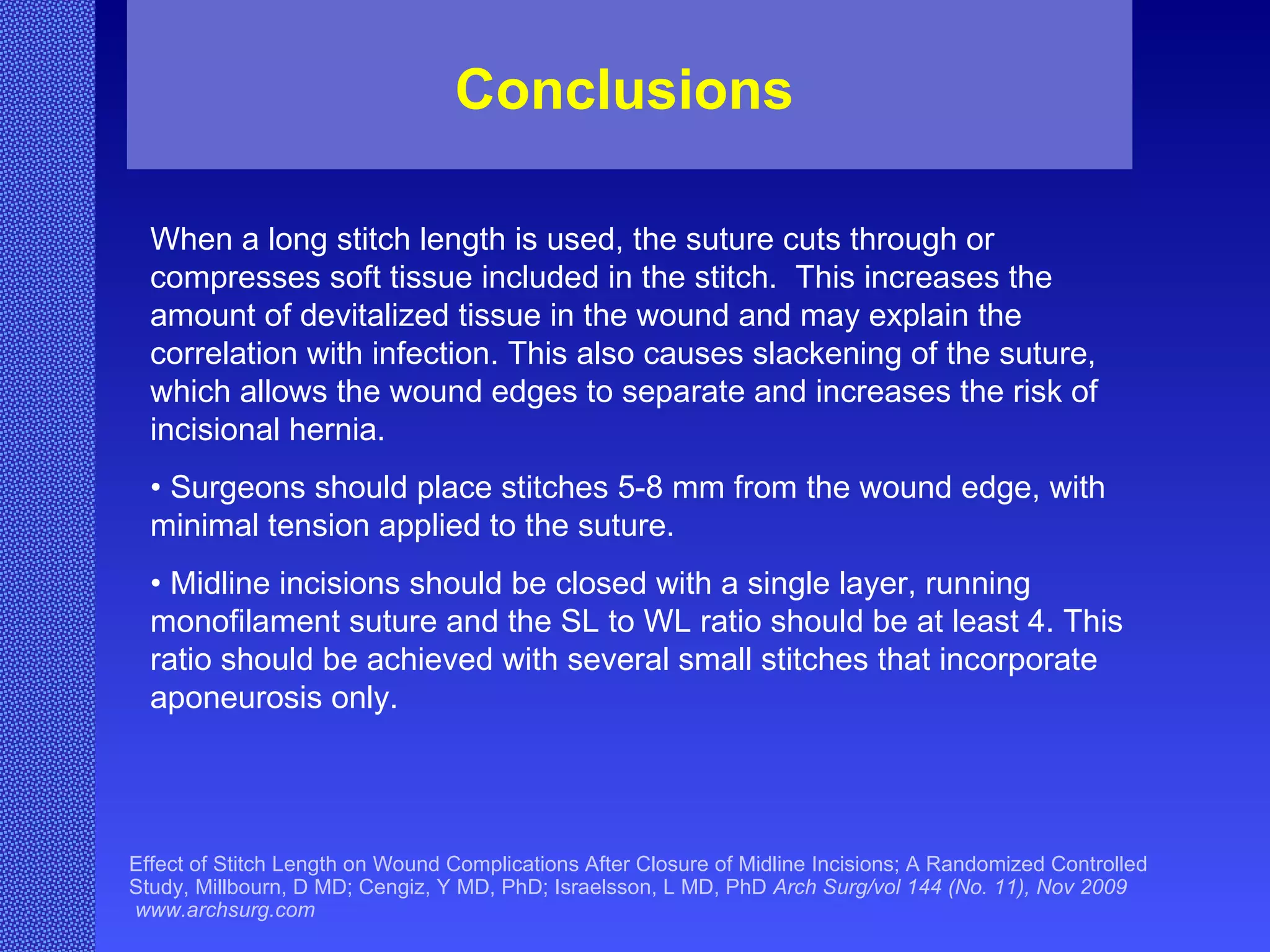
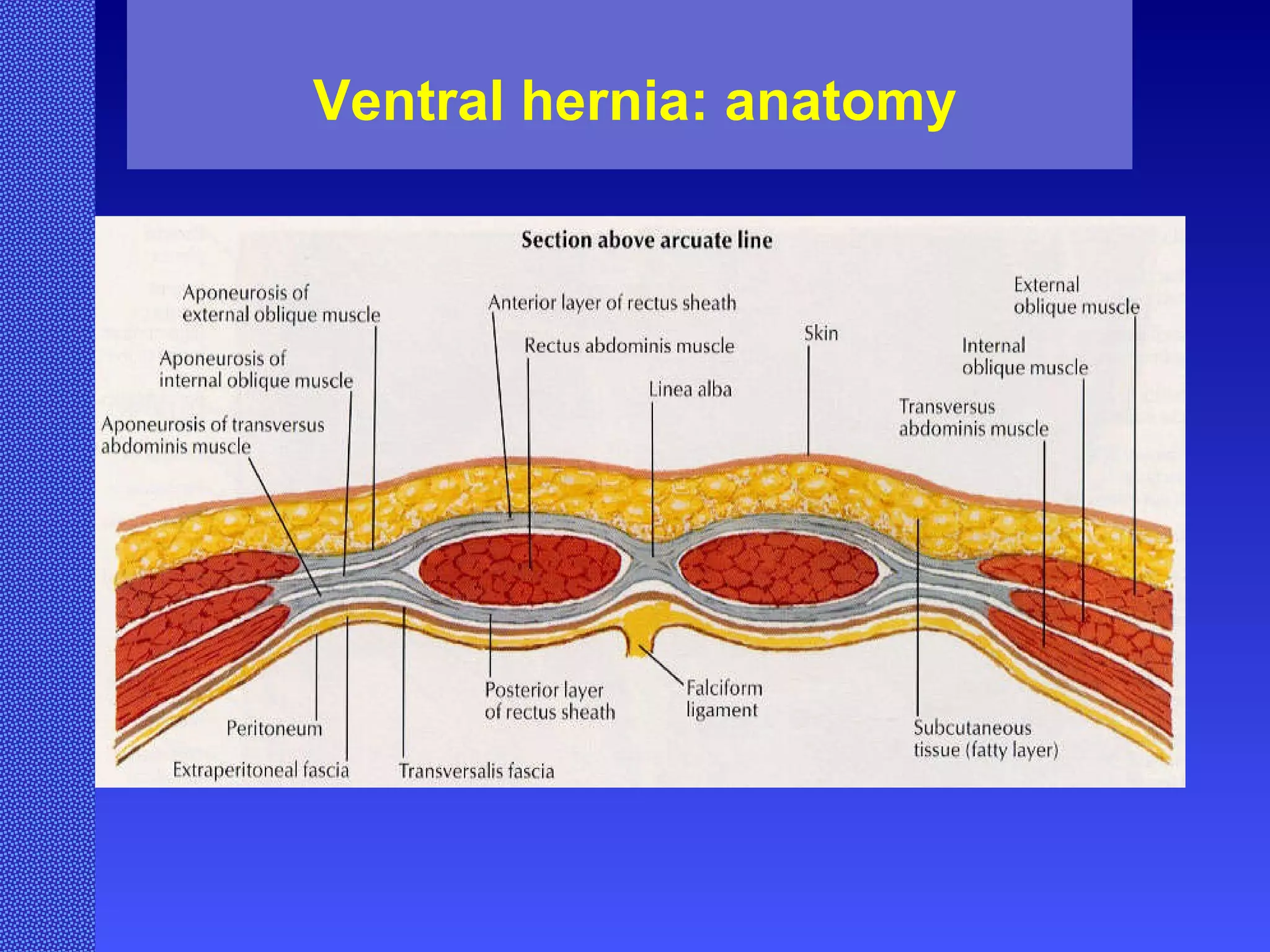
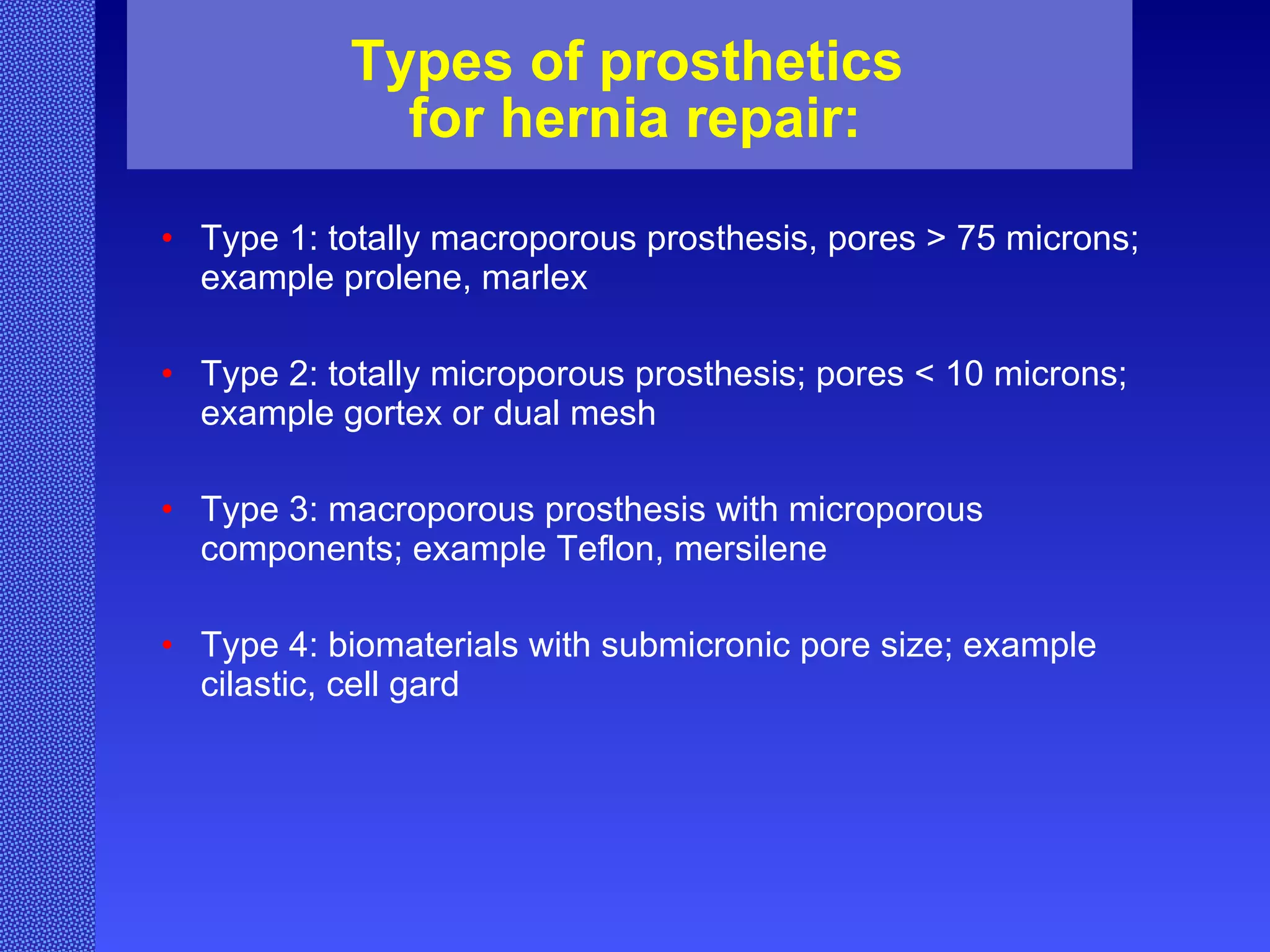
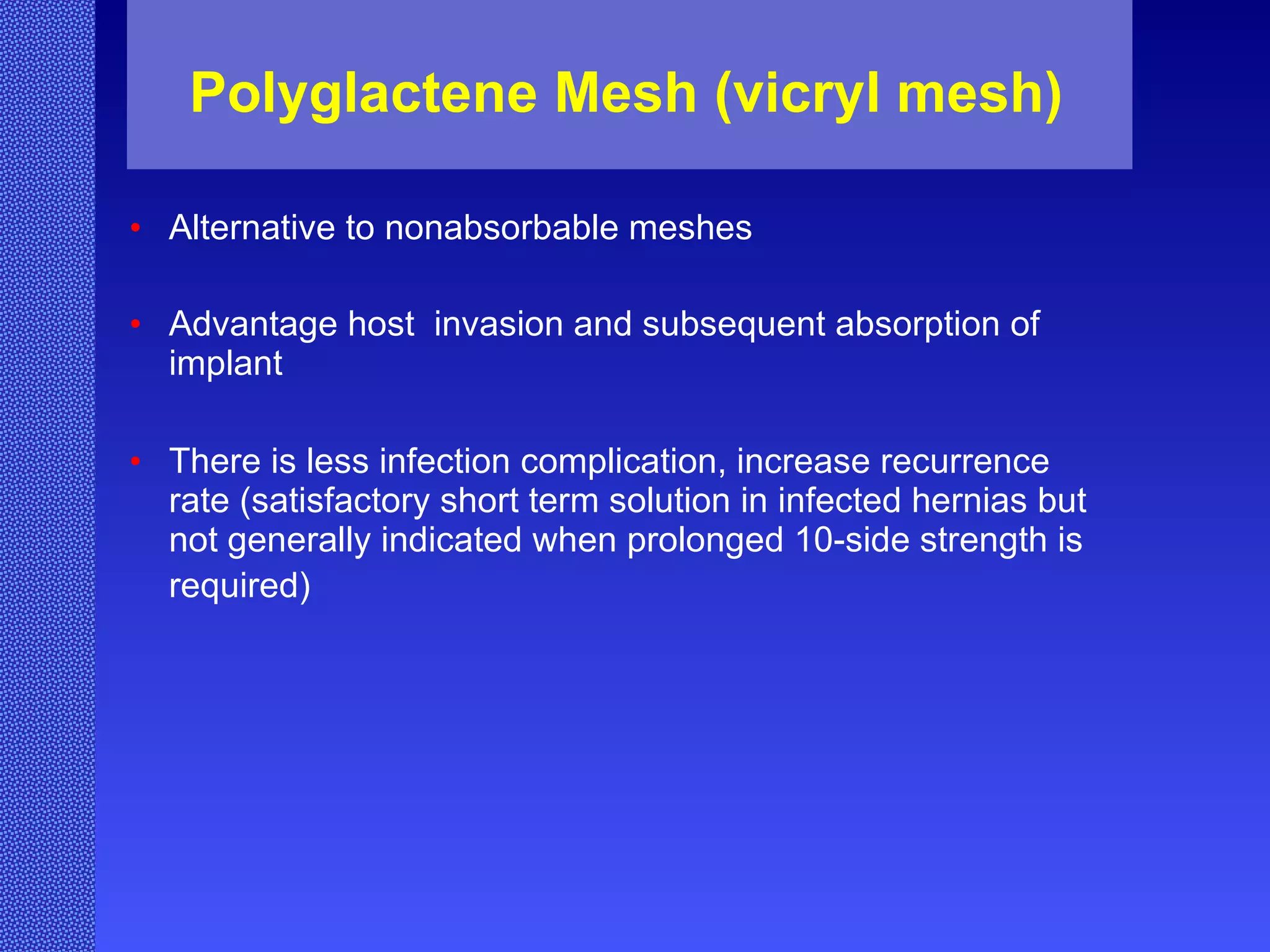
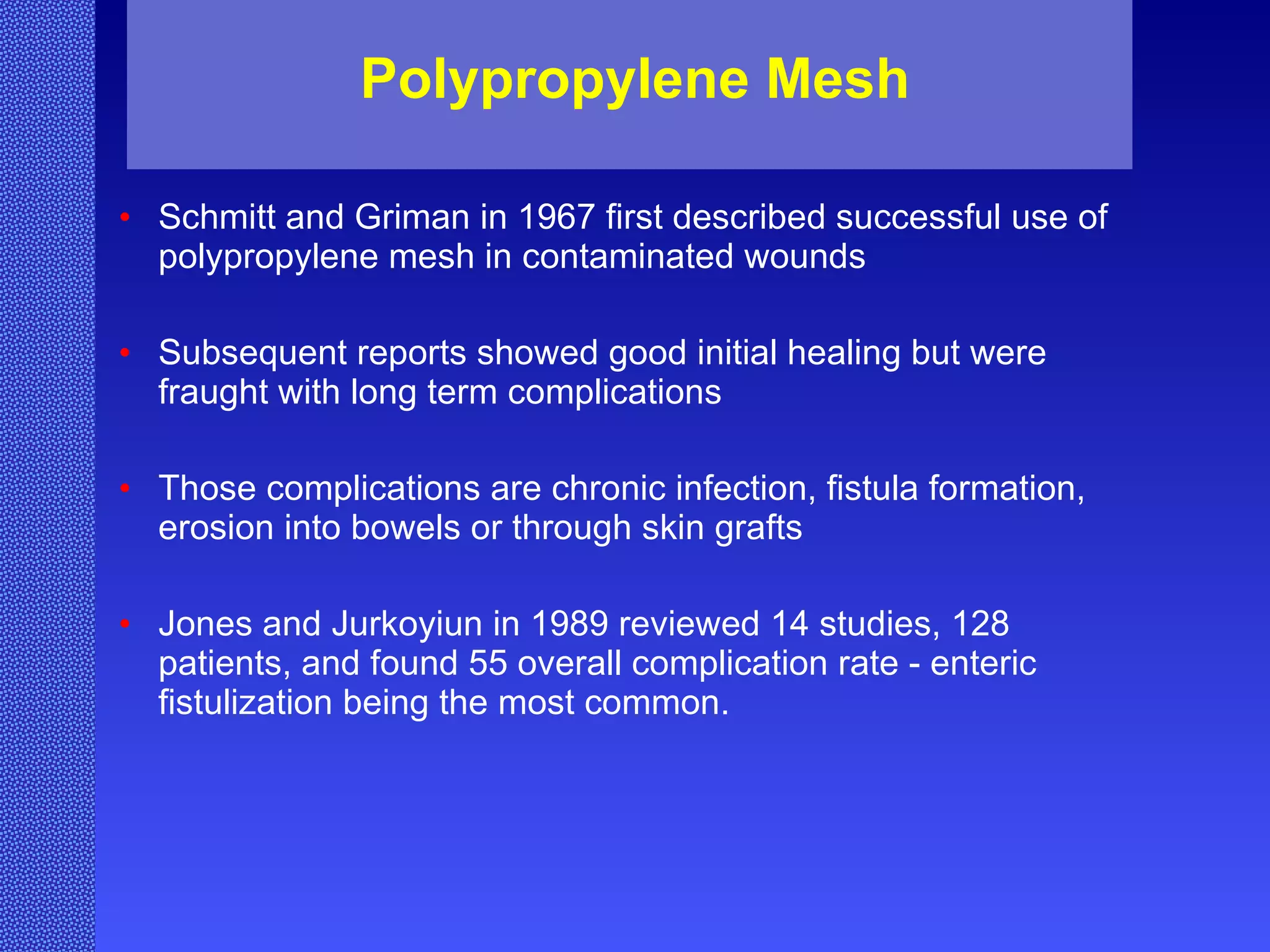
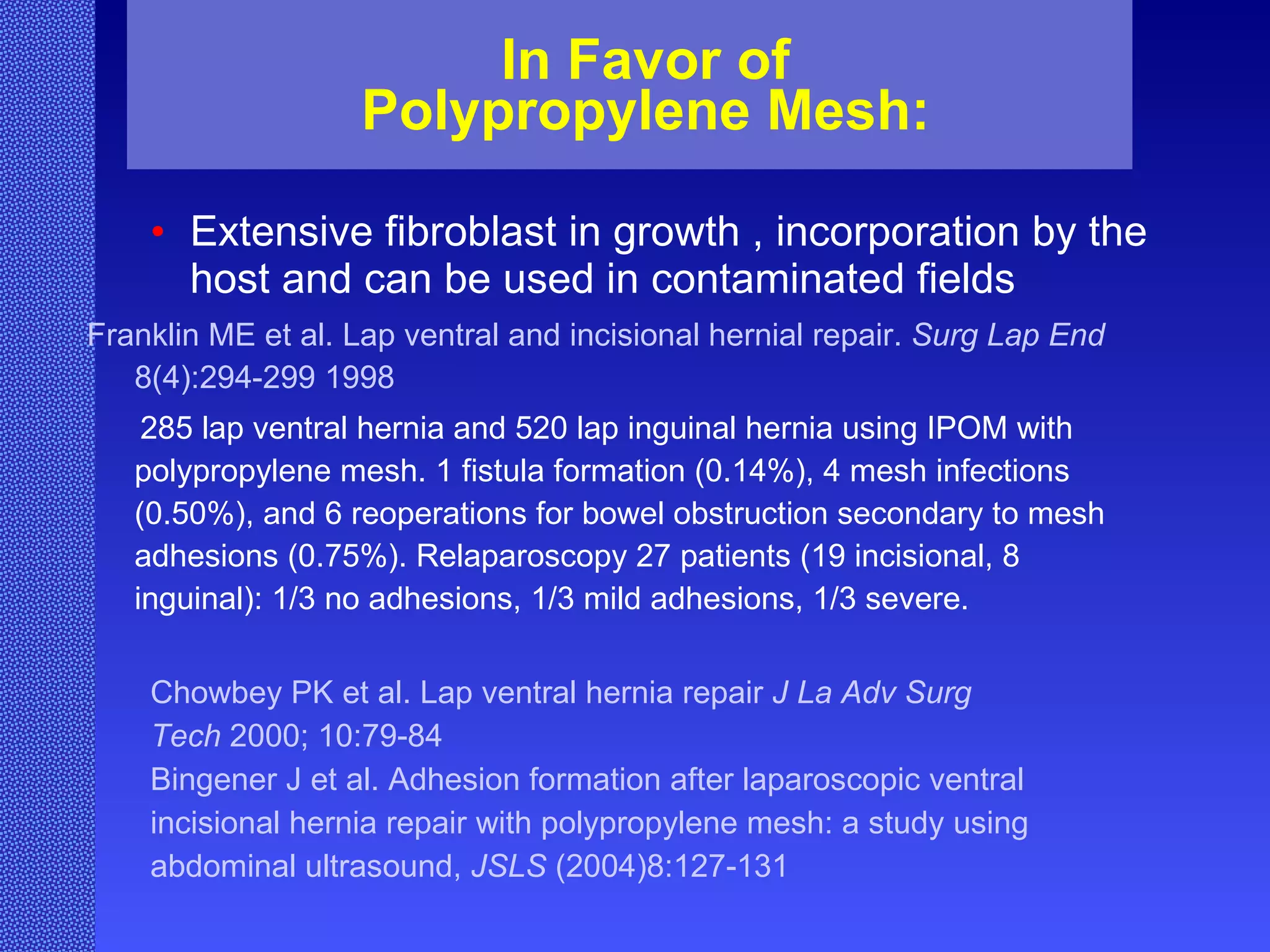
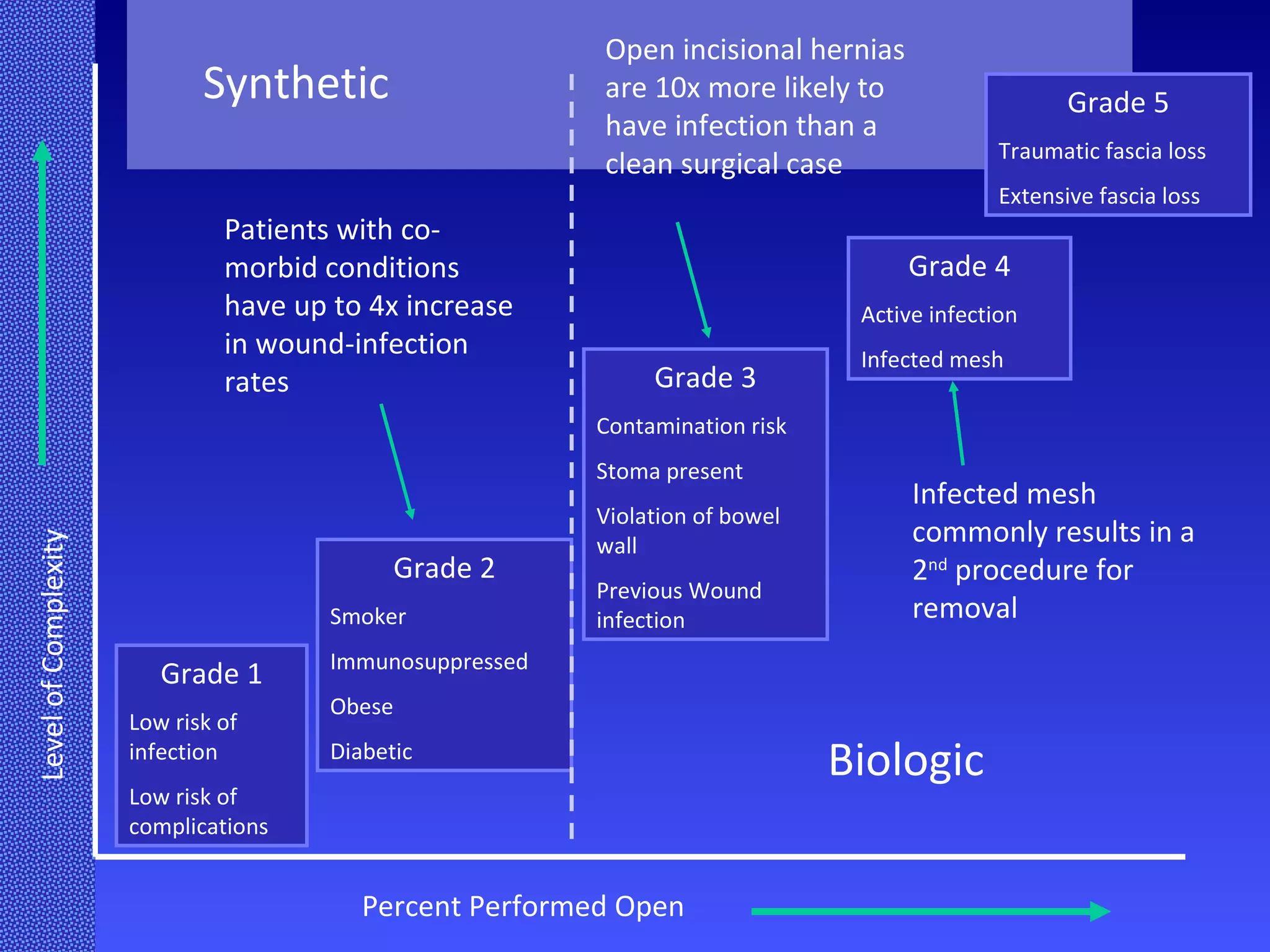
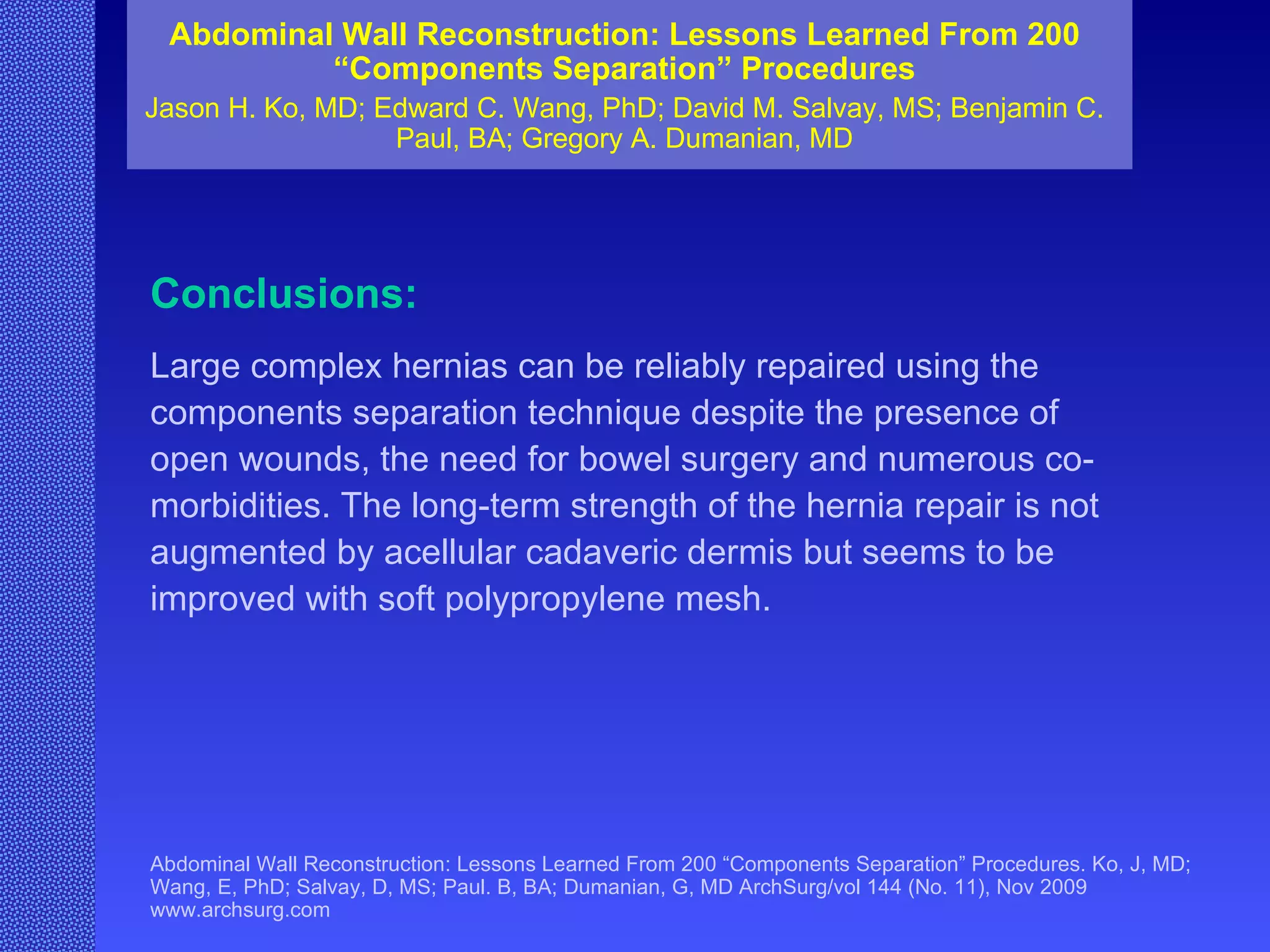
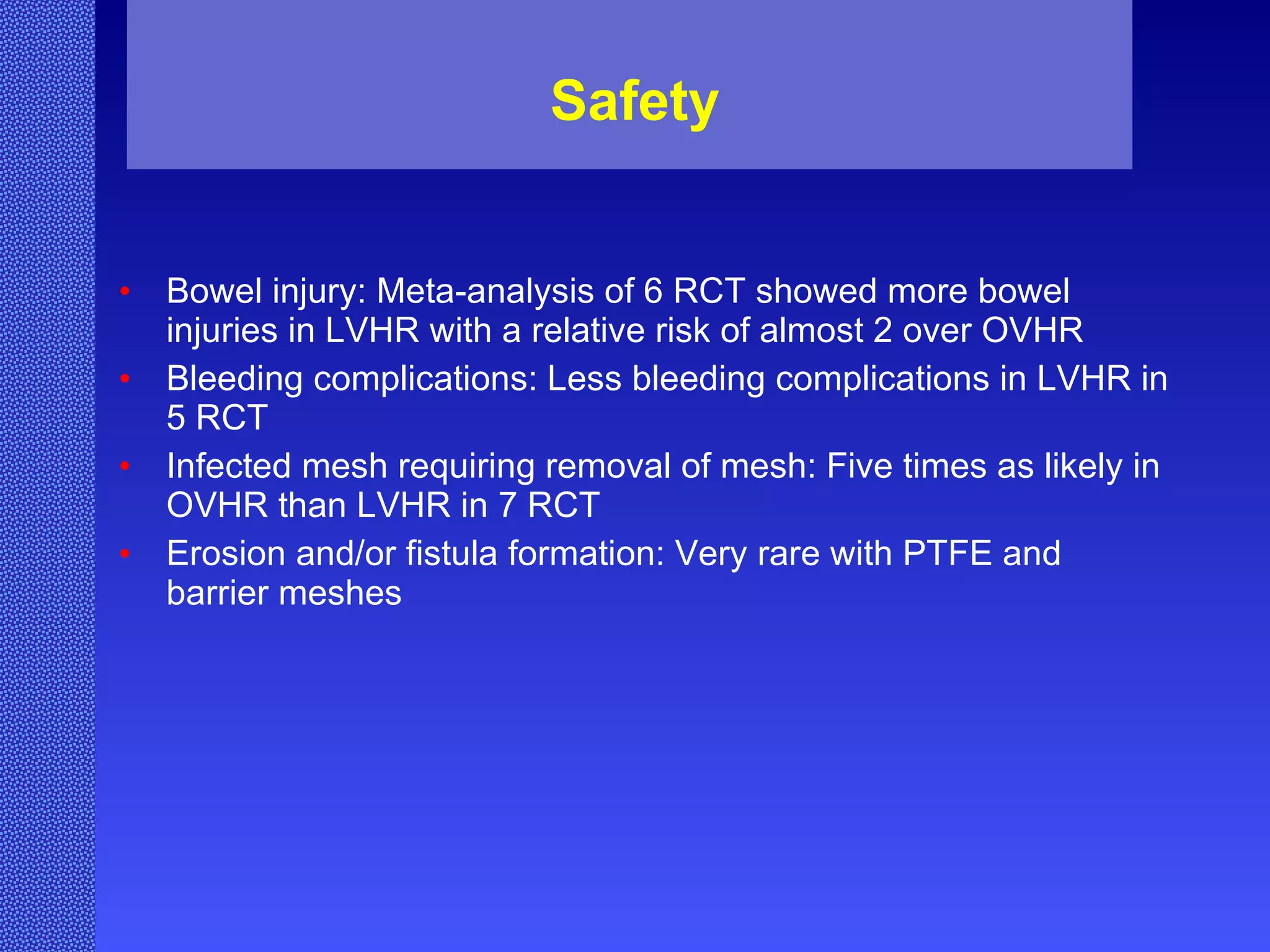
The document discusses surgical meshes and methods of fixation for hernia repair. It covers biologic and synthetic meshes and factors that influence hernia occurrence. Direct closure of hernias has a high recurrence rate of around 50%, which is reduced to around 5-18% when meshes are used. Long stitch lengths during closure are associated with higher rates of surgical site infection and hernia recurrence compared to short stitch lengths. Polypropylene meshes allow for tissue ingrowth but can cause complications like chronic infection, fistulas and erosion over time. Other synthetic mesh options discussed include ePTFE meshes.






![Safety Review of 5245 patients entered into NSQIP (between 2005 and 2006) with comparable ASA class, wound class, and age revealed: No difference in return to OR within 30 days [2.6% vs. 2.6%] Less deep infections in the laparoscopic group [0.5% vs. 1.6% p=0.001] Hwang, CS, Journal of Surgical Research, 3/2009](https://image.slidesharecdn.com/surgicalmeshesandmethodsoffixation-110216105541-phpapp01/75/Surgical-Meshes-and-Methods-of-Fixation-146-2048.jpg)