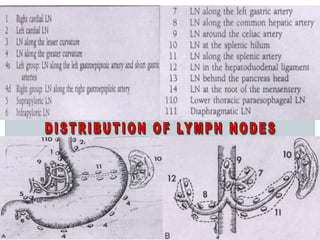
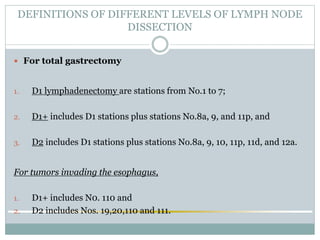
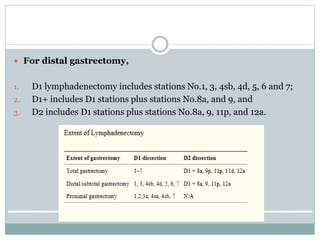
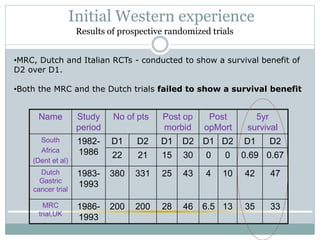
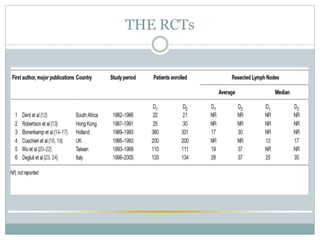
This document discusses the current evidence for D1 and D2 gastrectomy in treating gastric cancer. It begins by defining the lymph node stations and different levels of lymphadenectomy. It then reviews several key randomized controlled trials that compared D1 and D2 gastrectomy. While initial Western trials found higher morbidity and mortality with D2 without survival benefits, later long-term follow up and recent trials demonstrate lower recurrence rates and improved survival with D2 gastrectomy when performed safely. The consensus is that D2 gastrectomy with preservation of the spleen and pancreas can achieve radical treatment for gastric cancer with excellent outcomes when performed by experienced surgeons.
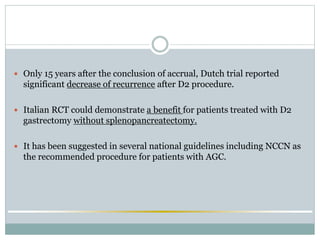
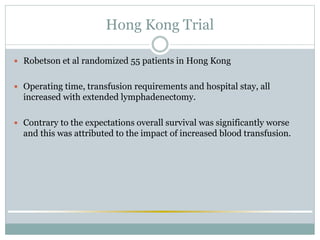
![ 15 year-follow up of the Dutch study
[Surgical treatment of gastric cancer: 15-year follow-up results of the randomised
nationwide Dutch D1D2 trial. Songun et al Lancet Oncol. 2010 May; 11(5):439-49]
1. Loco-regional recurrence rate is significantly lower in patients
treated with D2 lymphadenectomy vs D1.
2. Survival benefit with the enlarged dissection.](https://image.slidesharecdn.com/d2distalgastrectomyfinal-190919190439/85/D2-distal-gastrectomy-final-26-320.jpg)
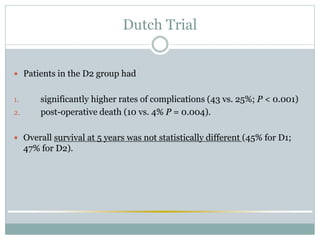
![ Studies recently demonstrated that even in Europe trained surgeons
could safely perform D2 with spleen and pancreas preservation and
More favourable recurrence pattern and cancer-related survival,
D2 seemed to be the recommended treatment for patients
with resectable gastric cancer .
[Extended lymph node dissection without routine spleno-pancreatectomy for treatment
of gastric cancer: low morbidity and mortality rates in a single center series of 250
patients.Biffi R et al J Surg Oncol. 2006 Apr 1; 93(5):394-400]](https://image.slidesharecdn.com/d2distalgastrectomyfinal-190919190439/85/D2-distal-gastrectomy-final-27-320.jpg)
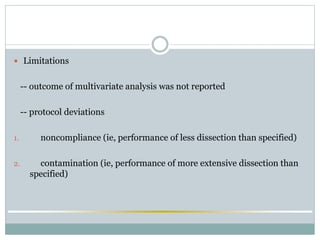
![ D2 dissection - limited risk of complications and mortality in the West, when
performed in specialized centers and avoiding spleno-pancreatectomy
[RCT comparing survival after D1 or D2 gastrectomy for gastric cancer.Degiuli M et al
Italian Gastric Cancer Study Group. Br J Surg. 2014 Jan; 101(2):23-31].
Only in selected cases more limited procedures (D1 plus) are adviced by
the GIRCG group.
1. high-risk patients (age > 70 yrs)
2. early forms with favourable pathological characteristics.](https://image.slidesharecdn.com/d2distalgastrectomyfinal-190919190439/85/D2-distal-gastrectomy-final-30-320.jpg)