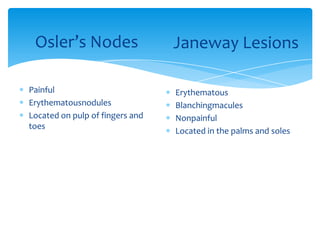
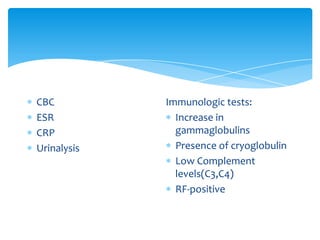
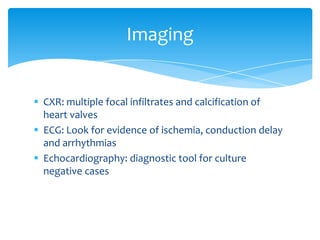
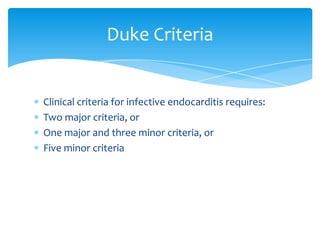
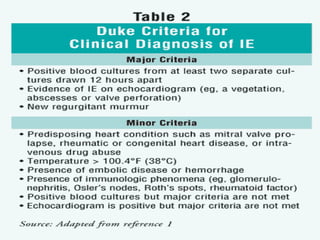
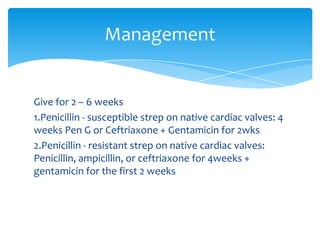
Infective endocarditis occurs when bacteria or fungi colonize the heart valves. It is classified into four groups depending on the valve affected and cause. The most common predisposing factors are intravenous drug use, prosthetic valves, previous endocarditis and dental procedures. Clinical presentations include fever, heart murmur, petechiae and neurological changes. Diagnosis involves blood cultures, echocardiography and application of the Duke Criteria. Treatment involves antibiotics for 2-6 weeks depending on the causative organism and affected valve.