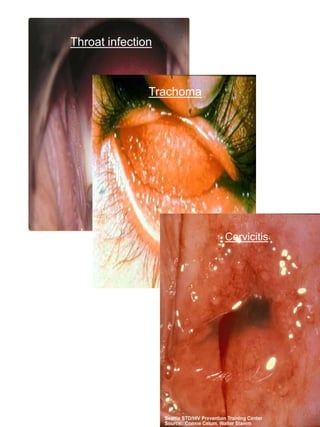
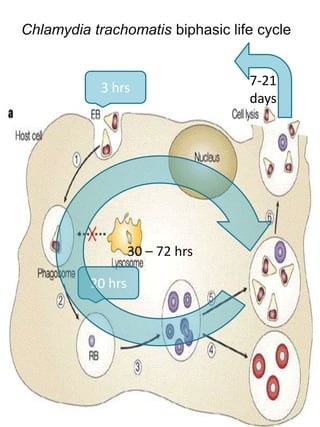
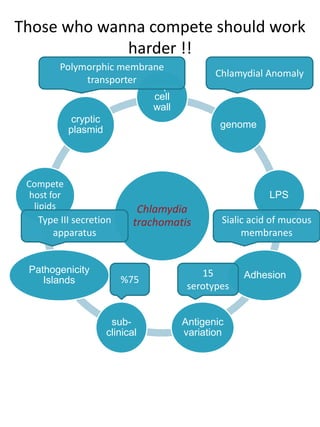
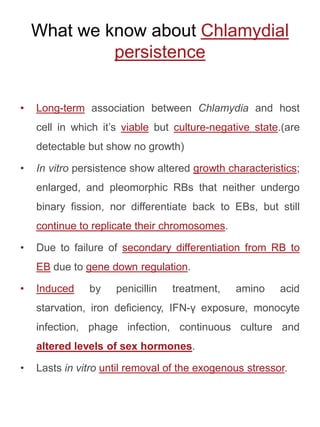
Chlamydia trachomatis is an obligate intracellular bacterium with a unique biphasic life cycle alternating between the infectious but metabolically inactive elementary body (EB) and non-infectious but metabolically active reticulate body (RB). It has developed several virulence factors that allow it to evade the host immune system, including a cryptic plasmid, type III secretion system, and the ability to enter a persistent dormant state. C. trachomatis causes a variety of diseases in humans by targeting mucosal surfaces and remains an important global public health issue.