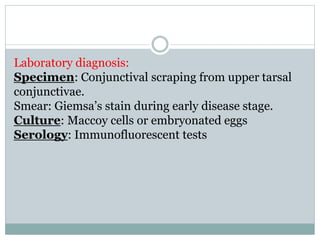
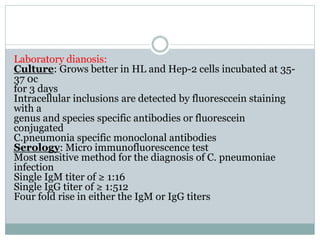
Mycoplasma and Chlamydia are important human pathogens. Mycoplasma pneumoniae causes atypical pneumonia in young people and is treated with erythromycin or tetracycline. Mycoplasma hominis and Ureaplasma urealyticum are normal flora but can cause genital infections treated similarly. Chlamydia trachomatis causes trachoma, genital infections, and lymphogranuloma venereum. It is diagnosed via staining or culture and treated with tetracycline or erythromycin. Chlamydia pneumoniae causes pneumonia and other respiratory infections diagnosed serologically and treated with tetracycline or macrolides.