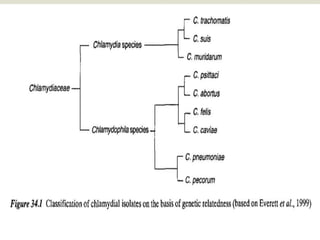
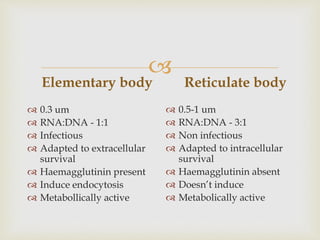
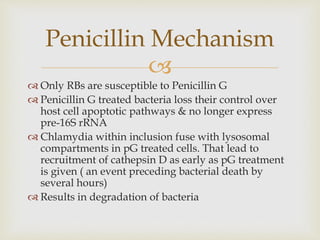
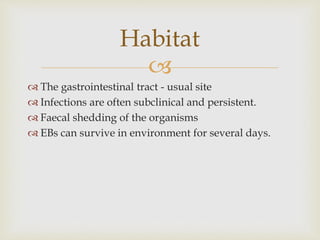
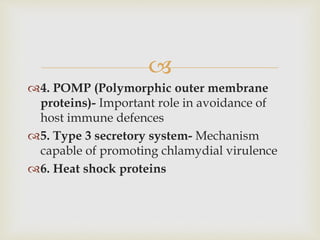
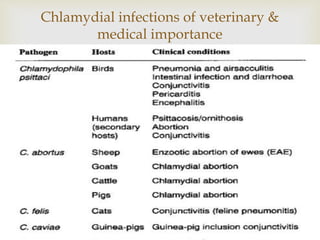
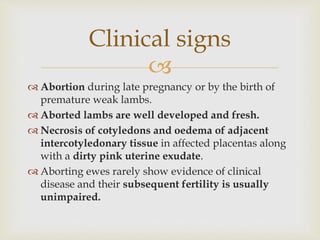
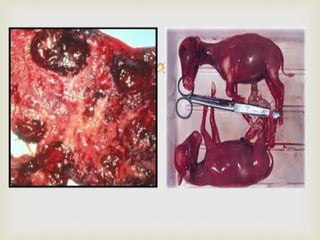
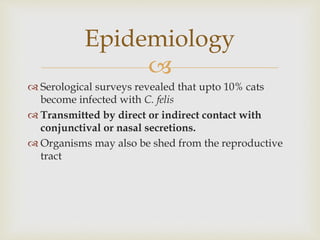
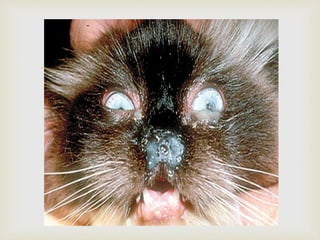
This document discusses the taxonomy, morphology, life cycle, pathogenesis and clinical significance of Chlamydia. It describes Chlamydia as intracellular bacteria that cause respiratory, enteric, and reproductive tract infections in animals and humans. Chlamydia have unique developmental cycles involving infectious elementary bodies and reproductive reticulate bodies. They are unable to generate ATP and are dependent on host cell metabolism. Chlamydial infections can cause diseases like enzootic abortion in ewes, feline chlamydiosis, and avian chlamydiosis.