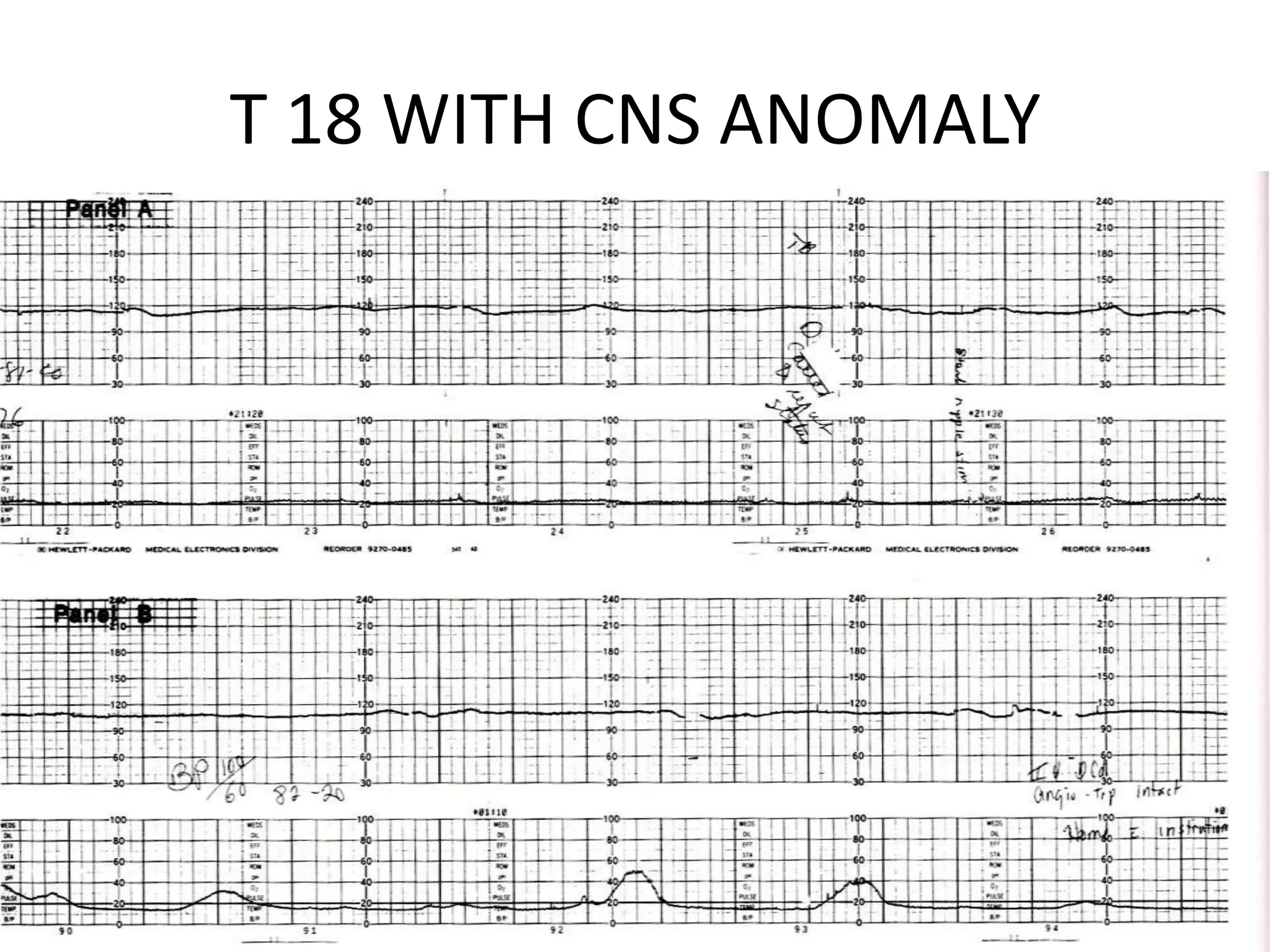
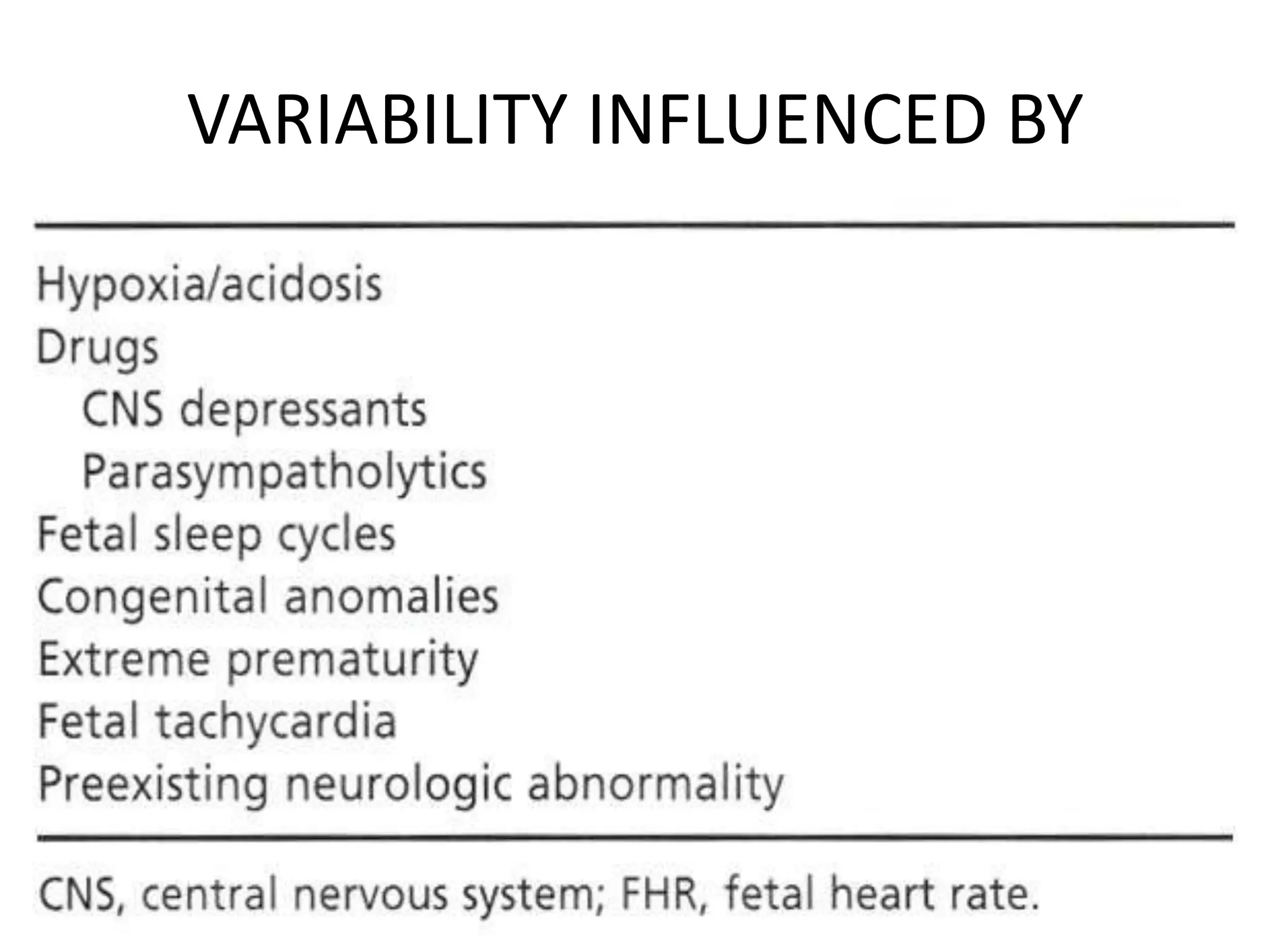
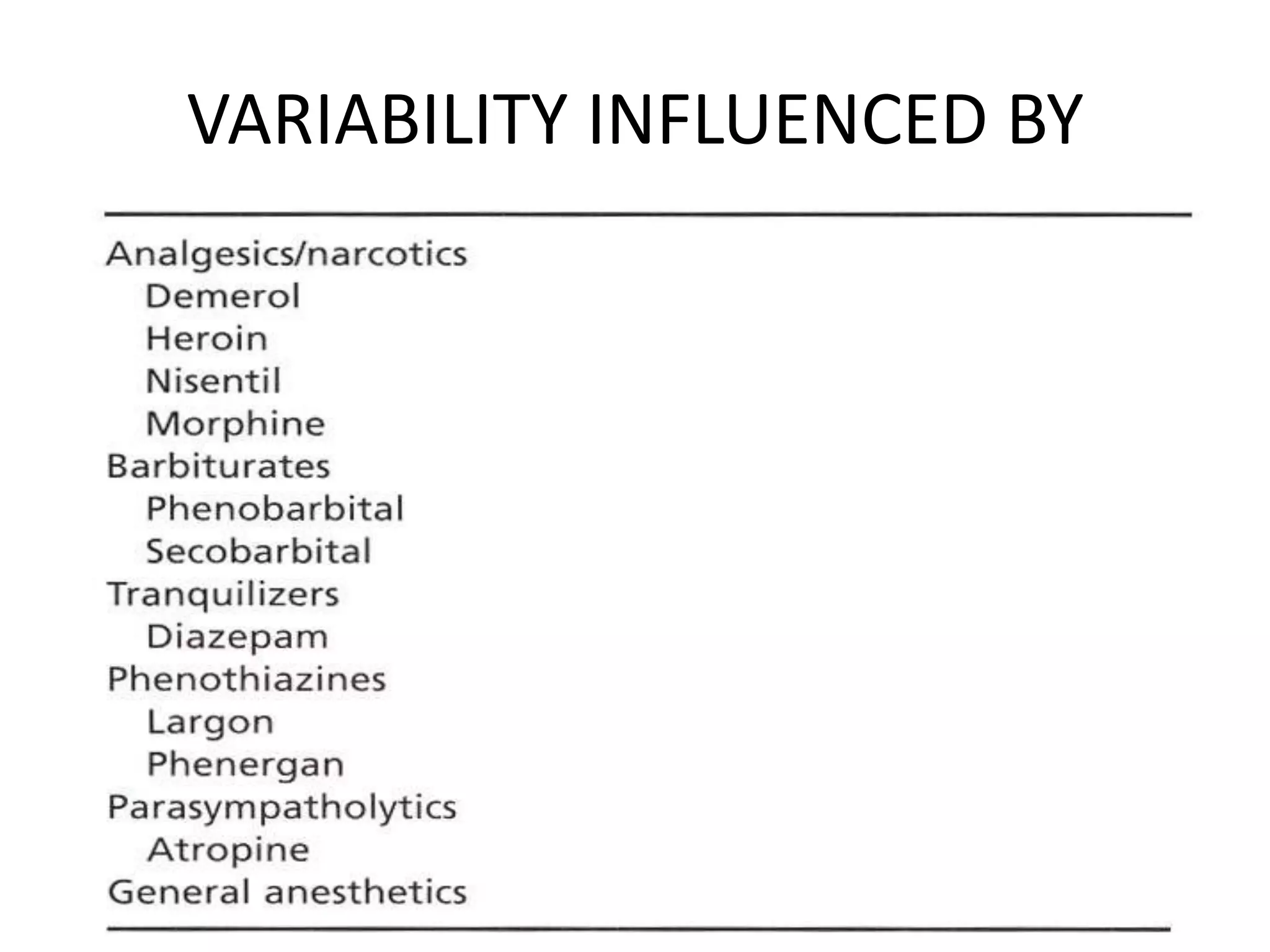
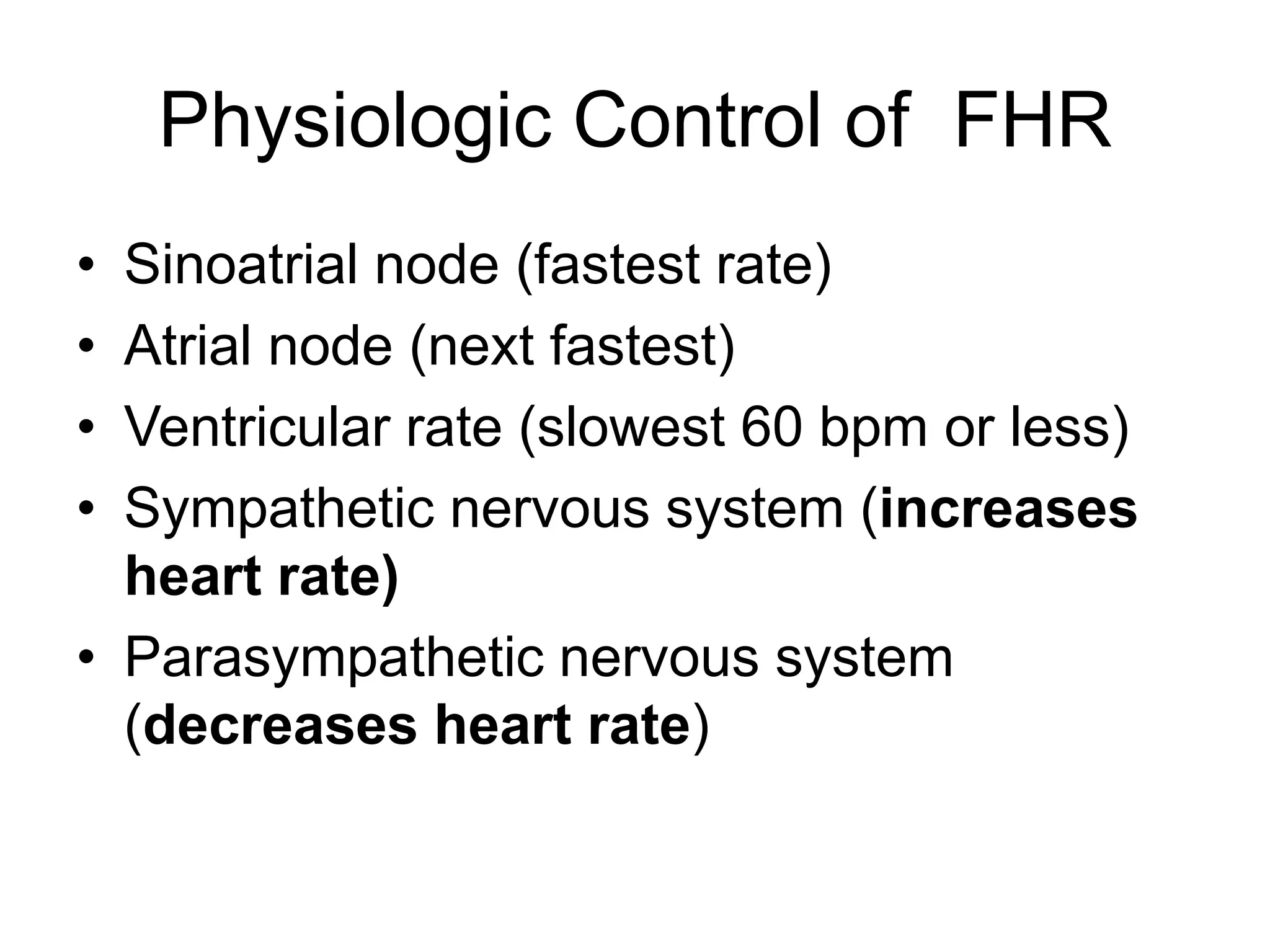
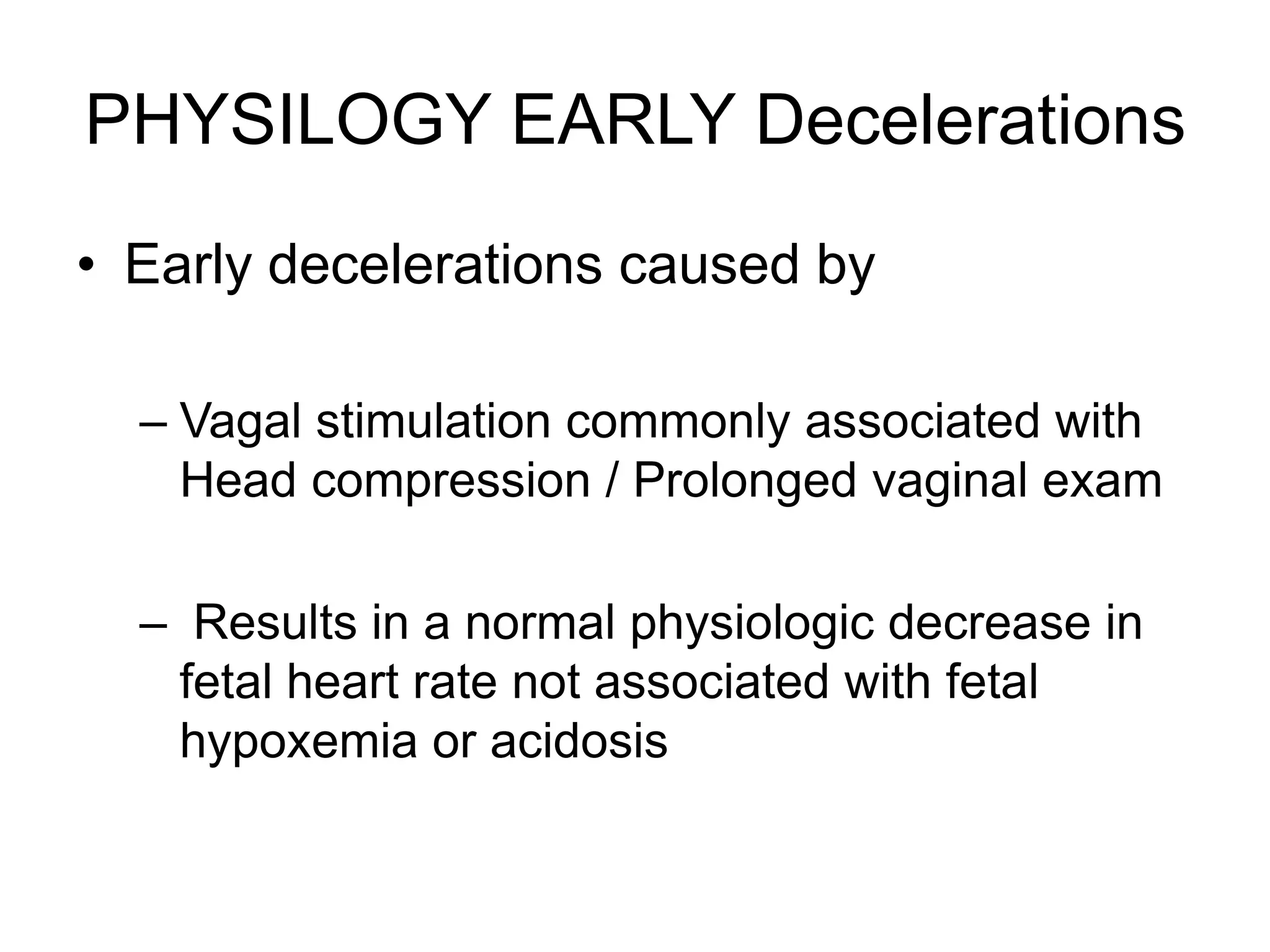
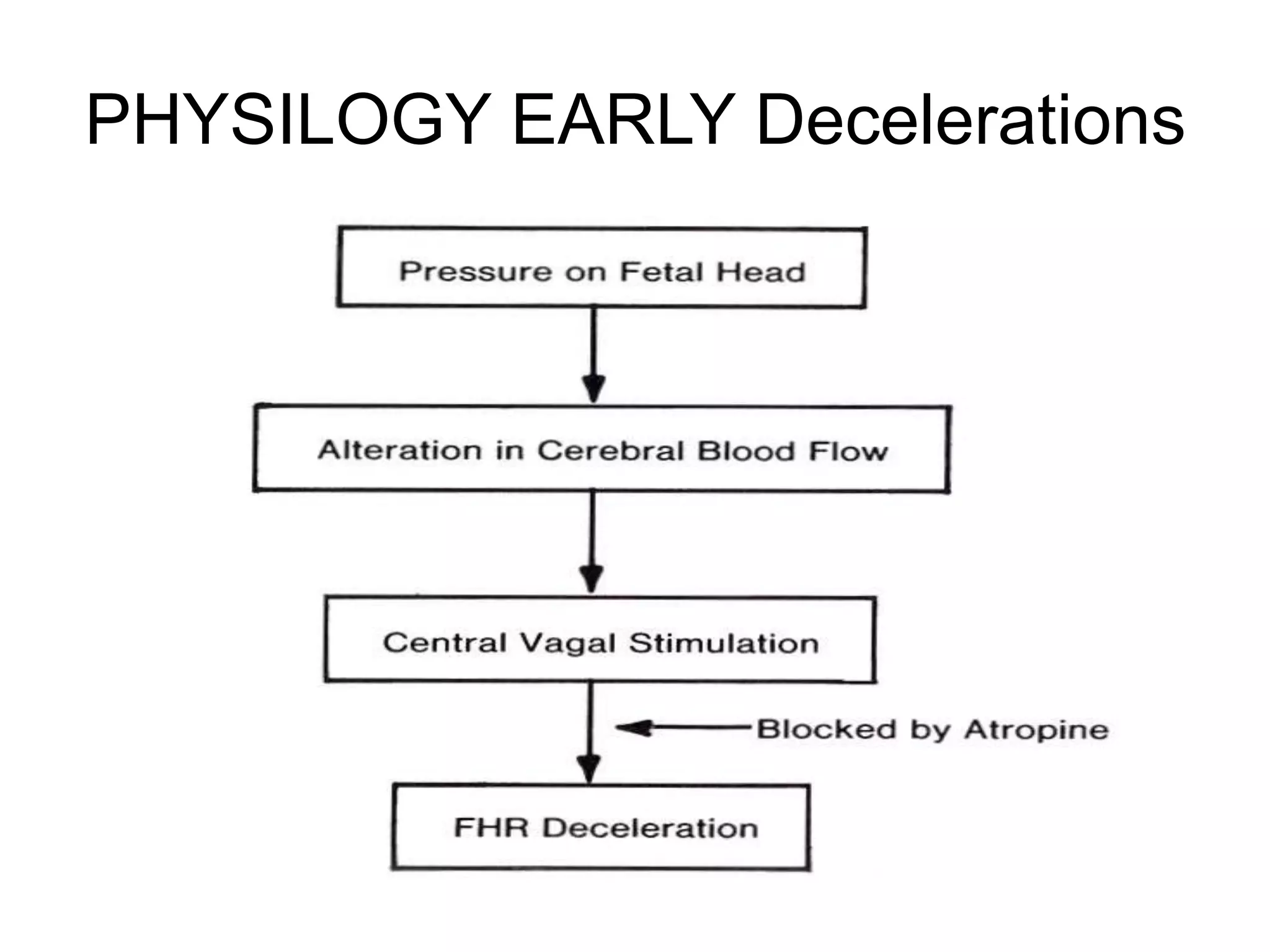
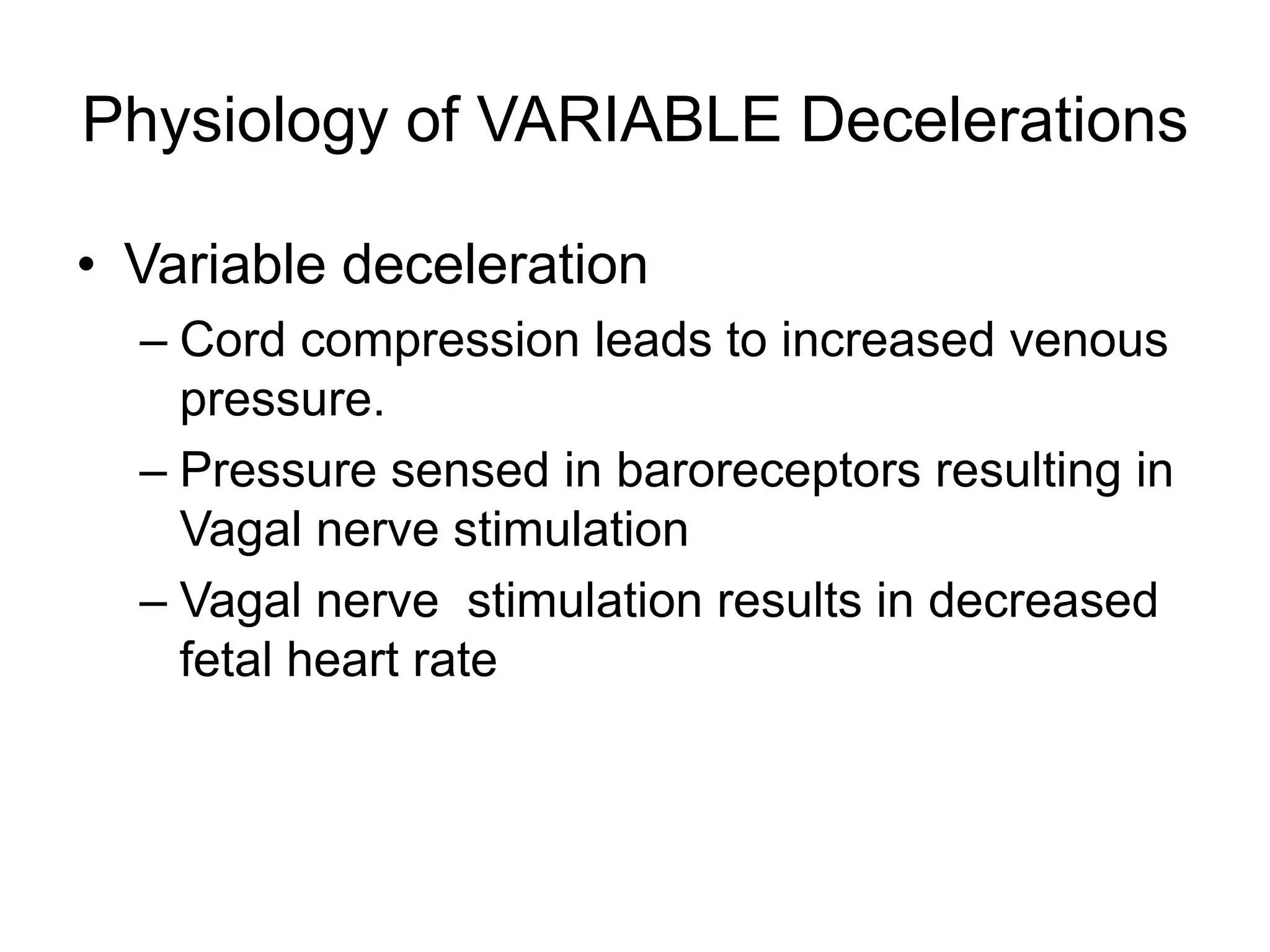
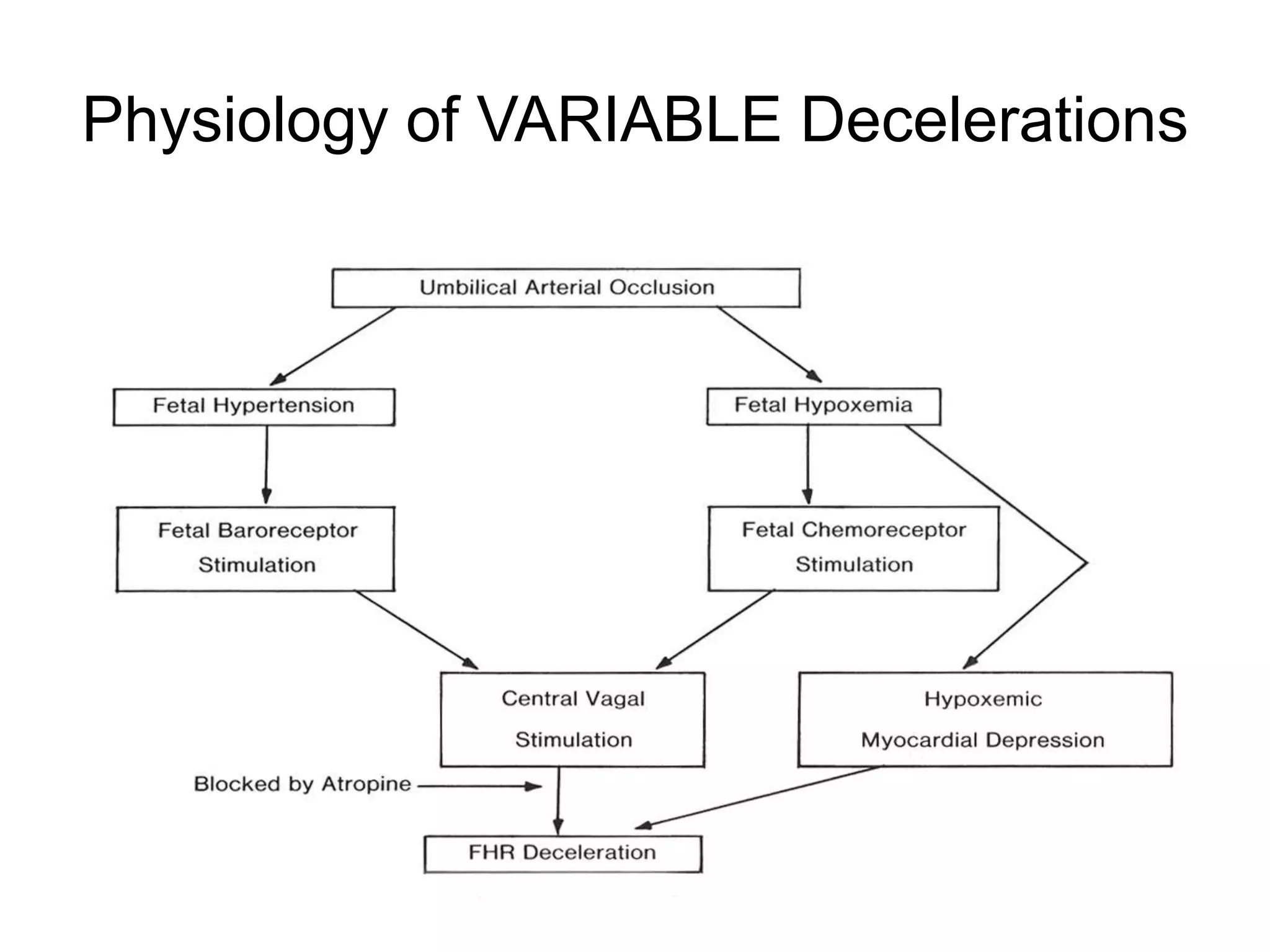
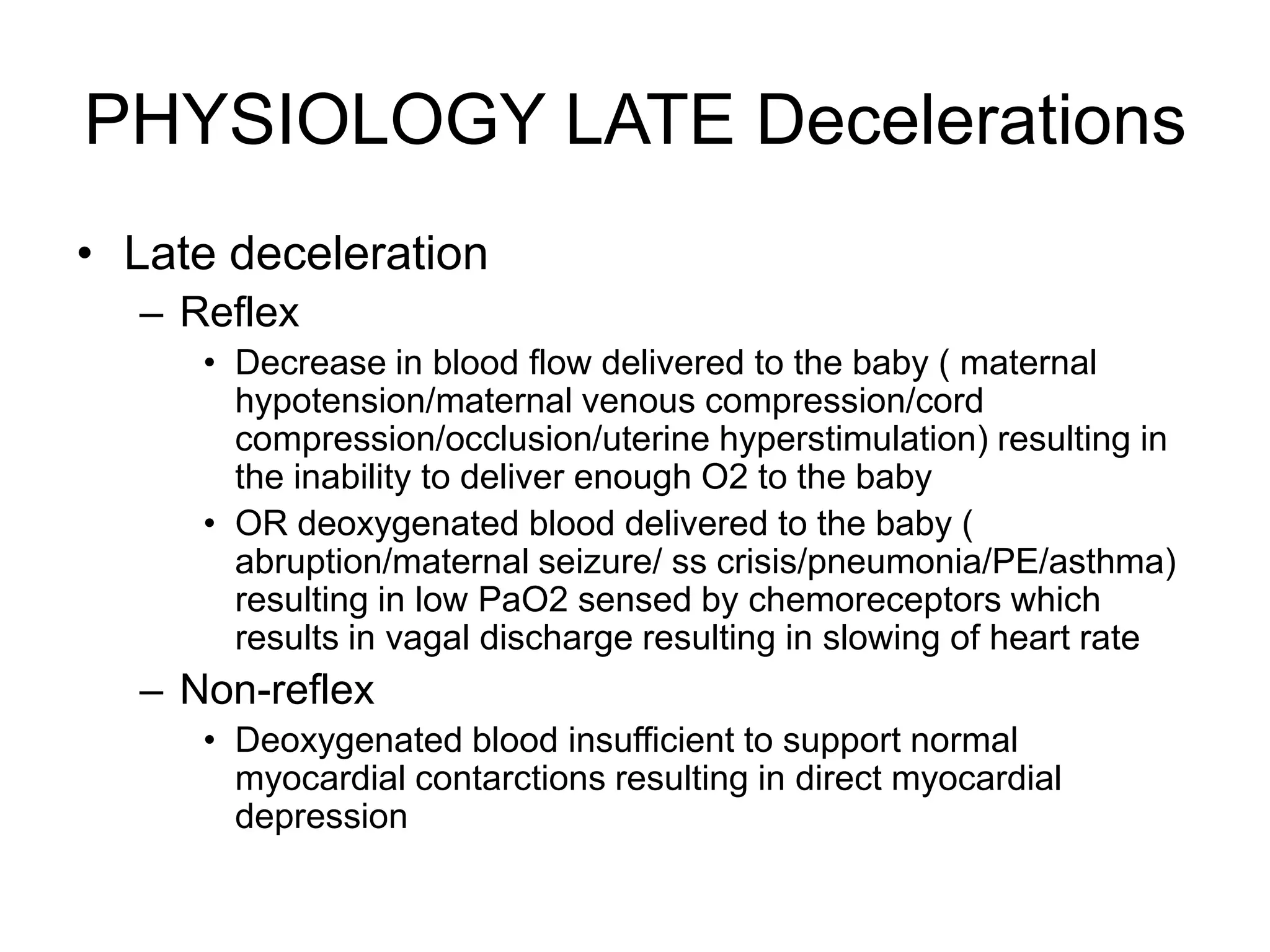
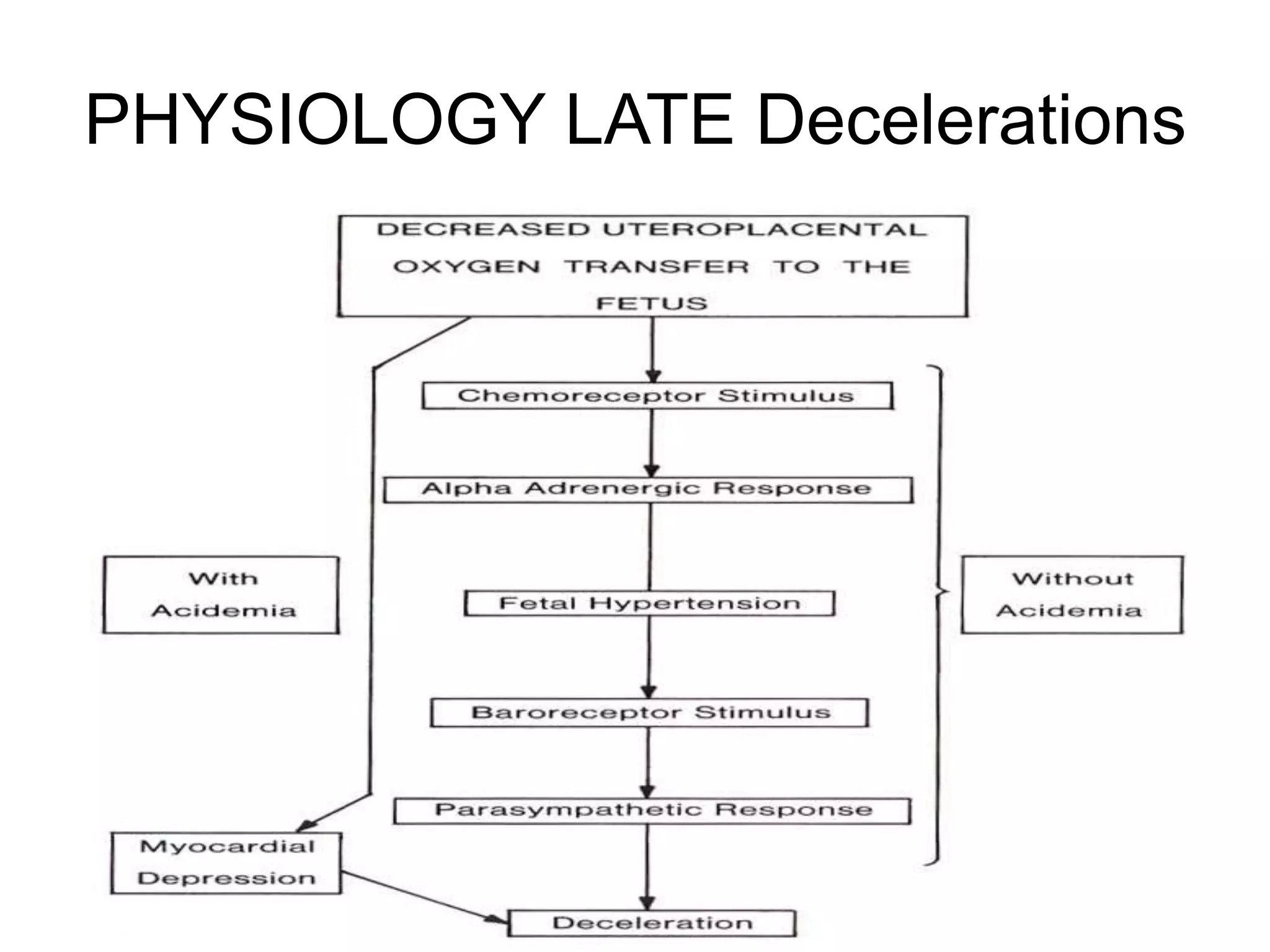
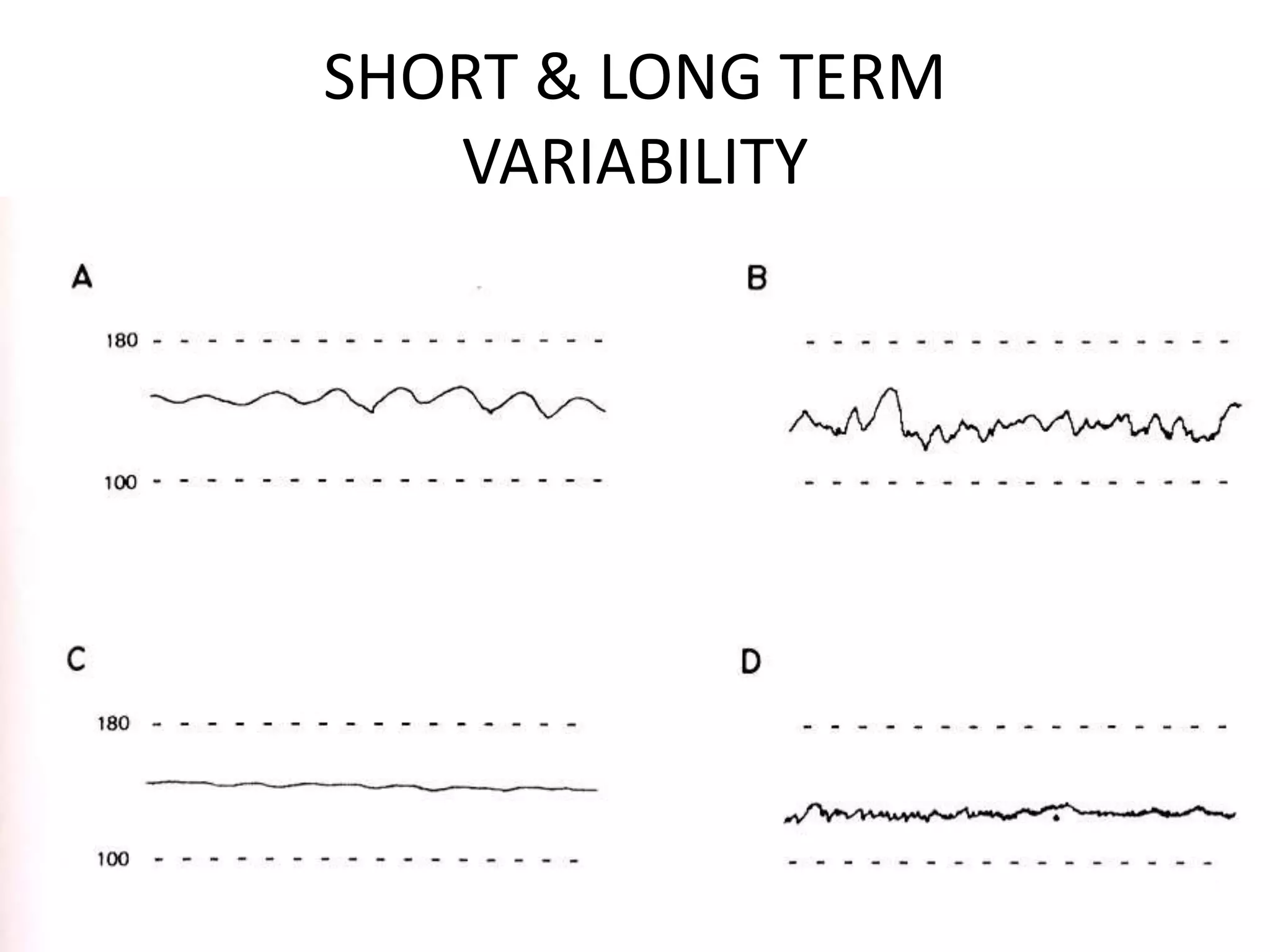
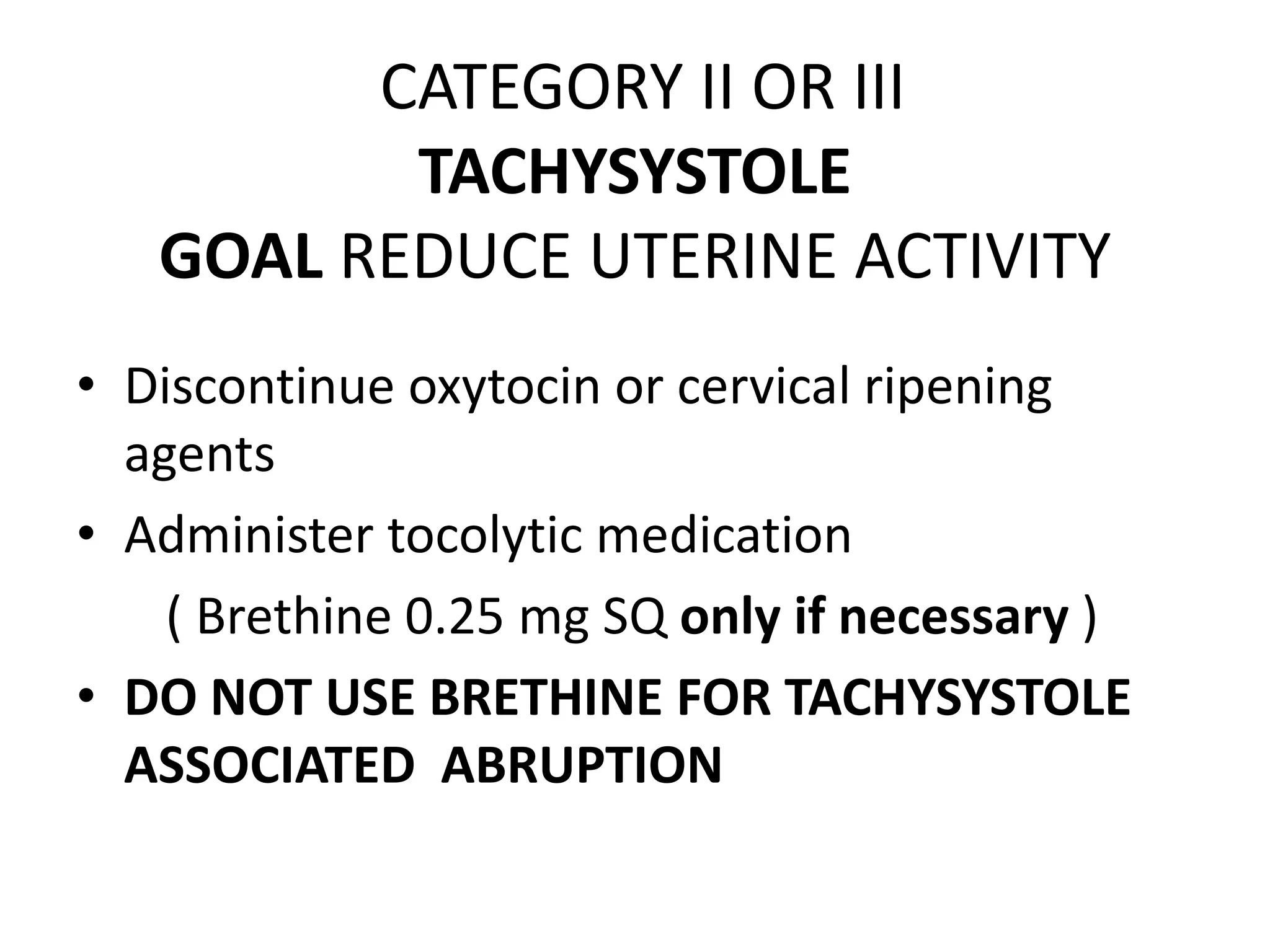
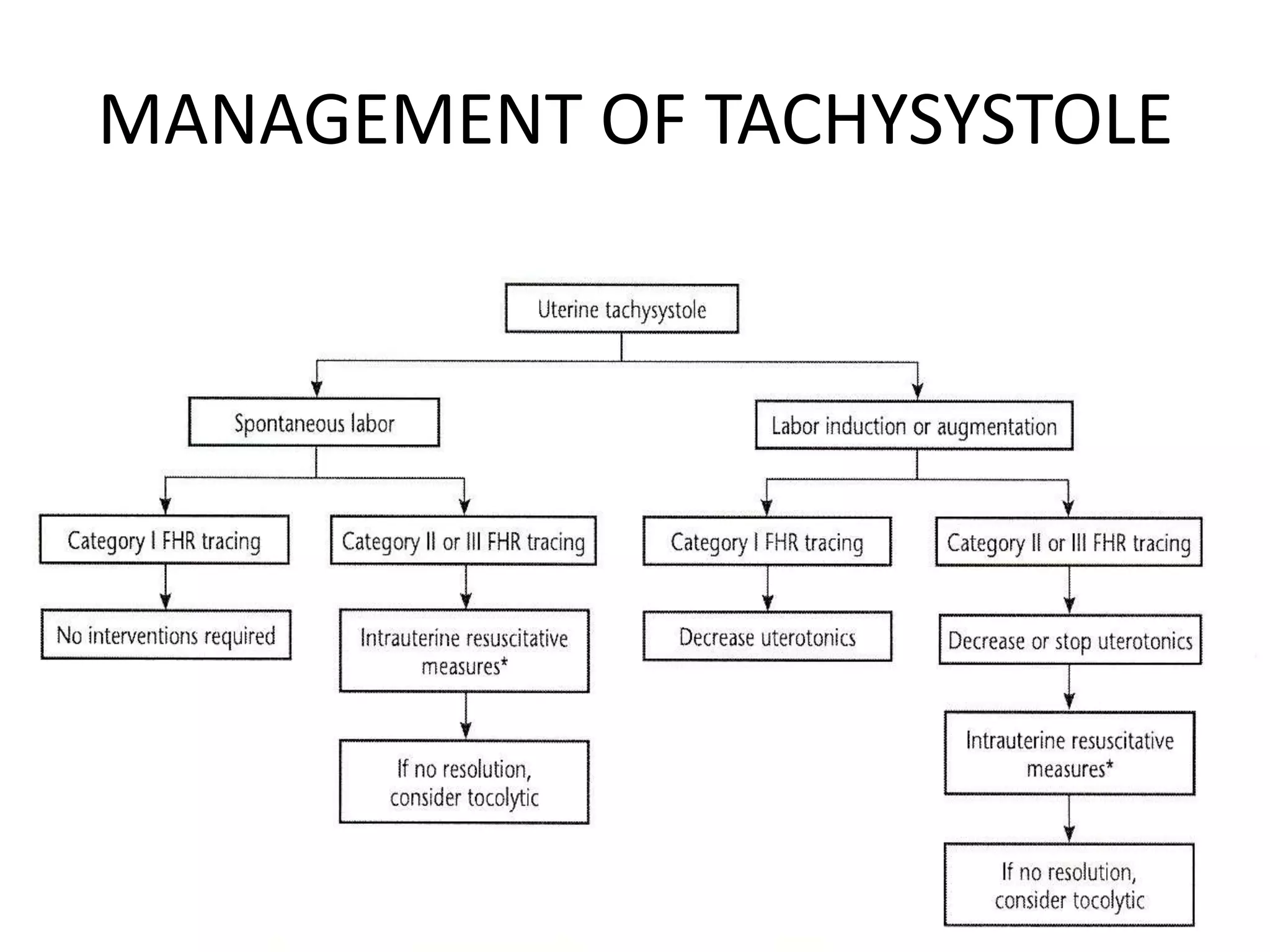
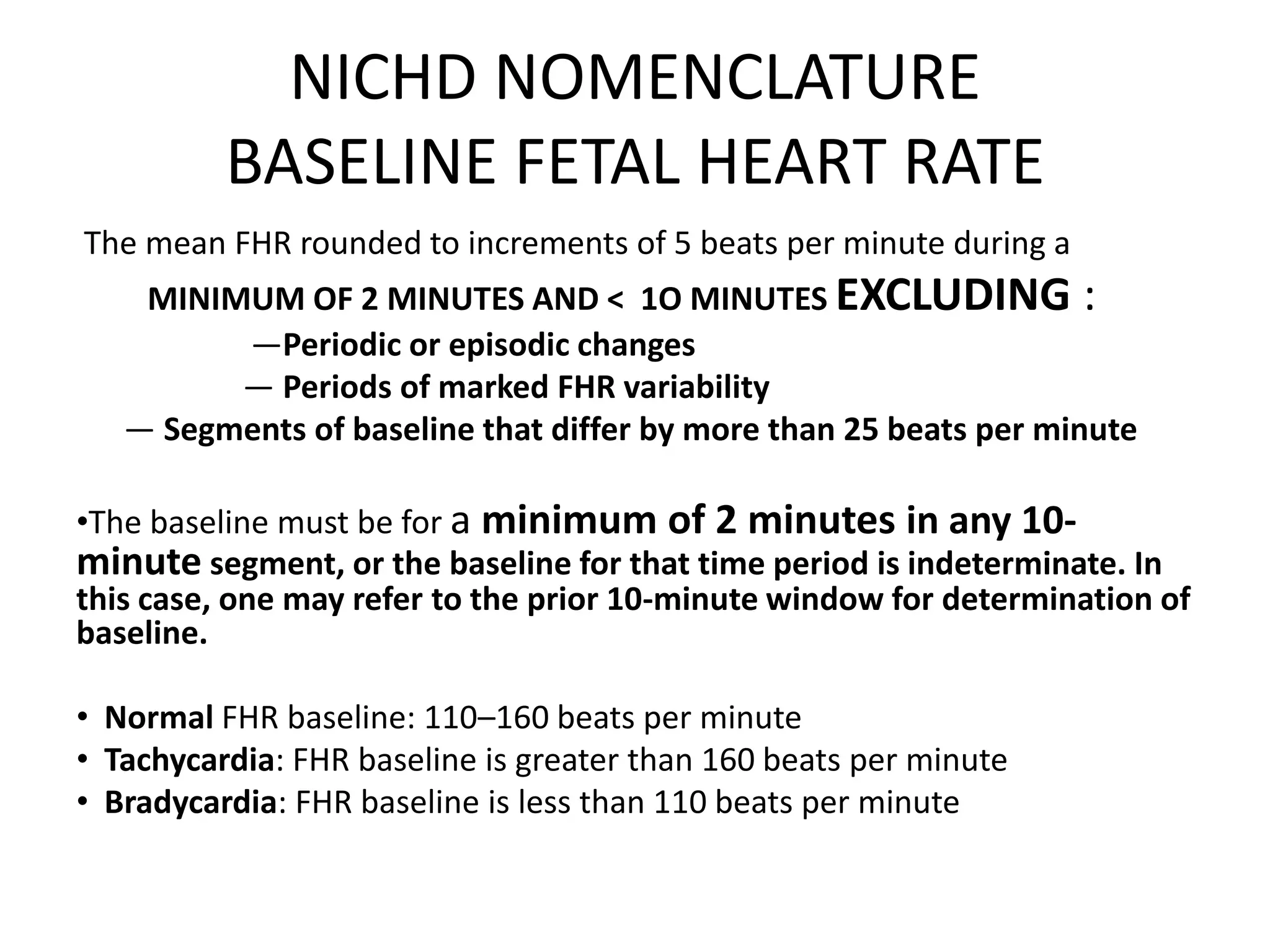
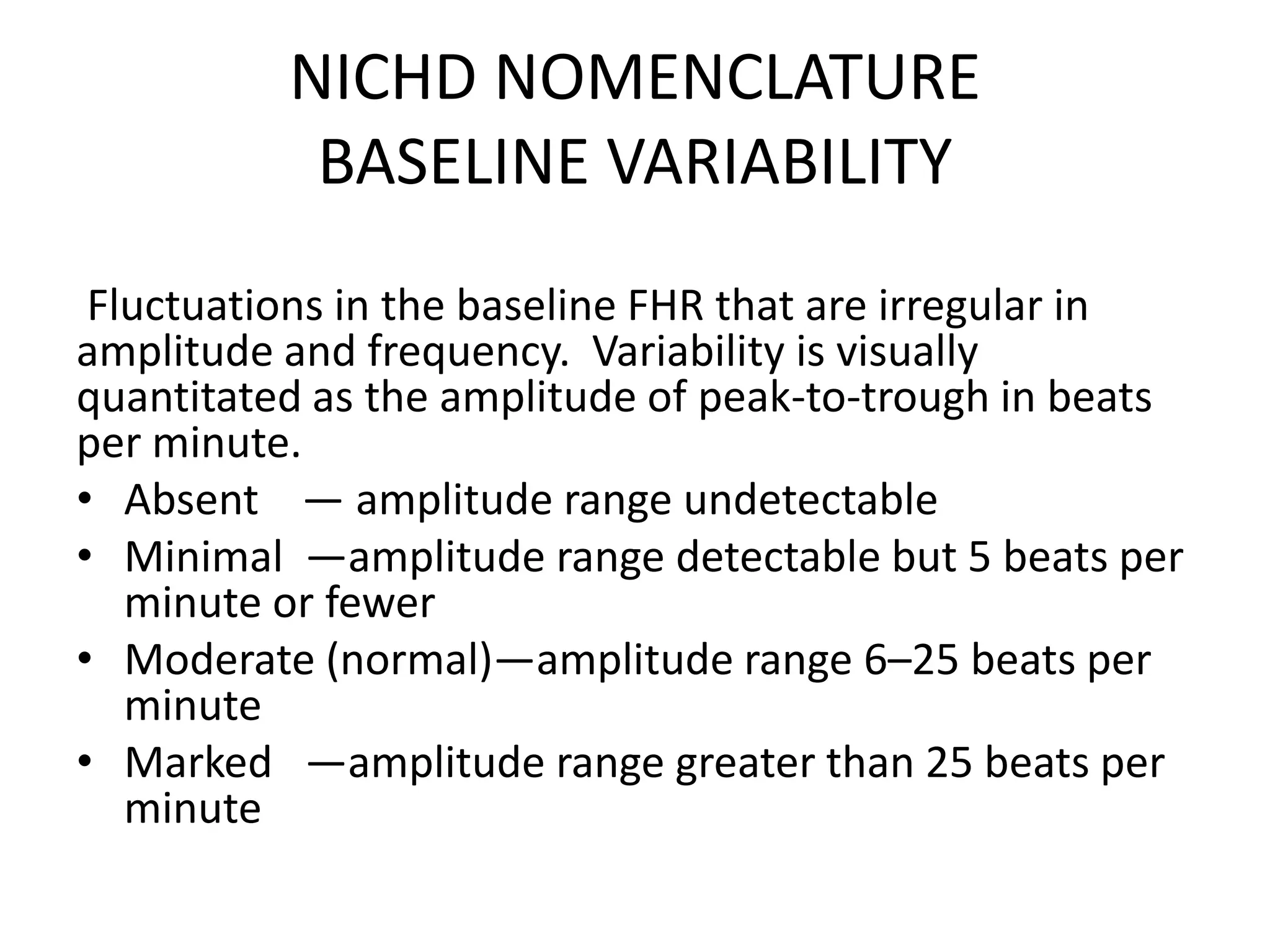
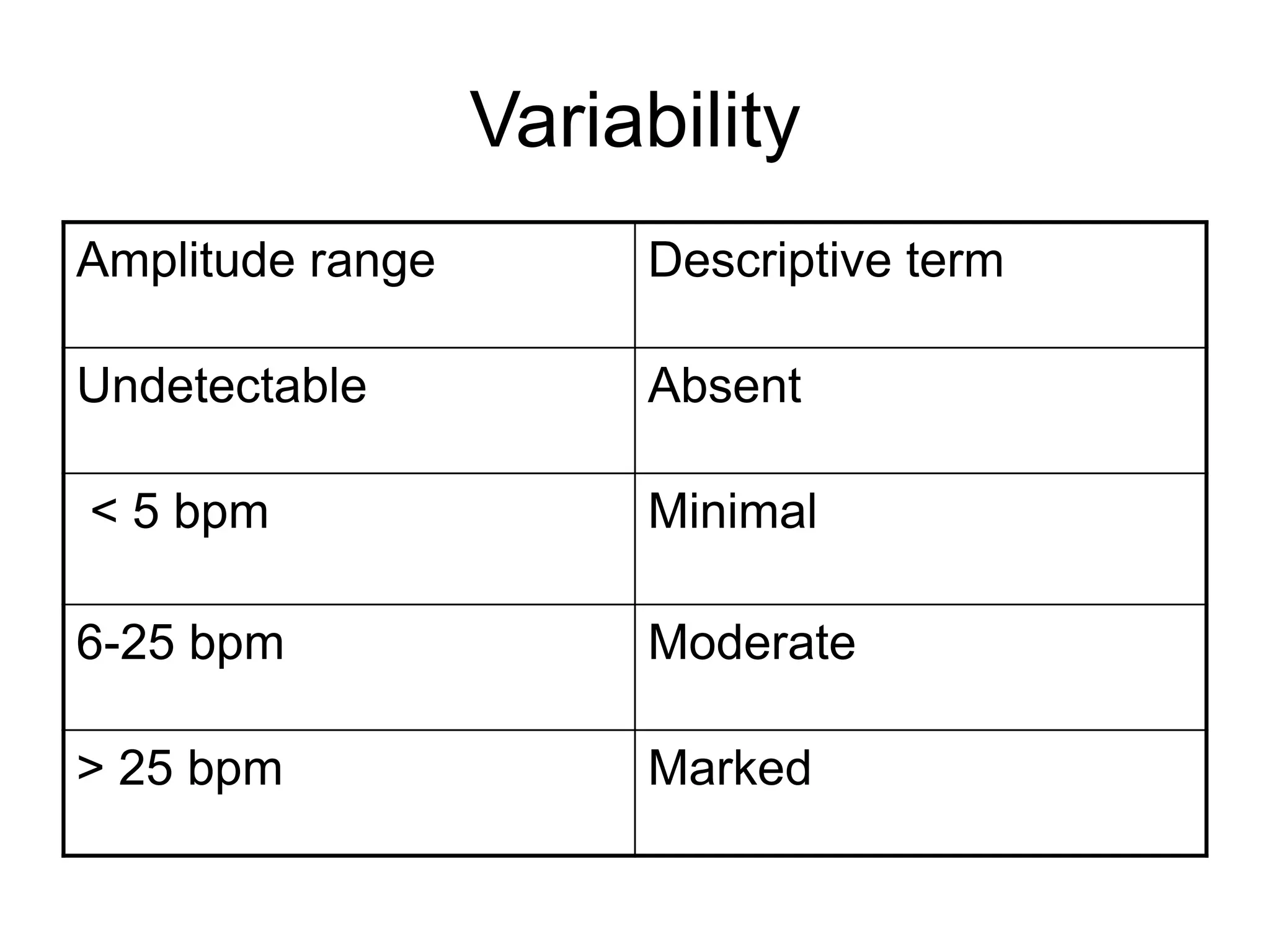
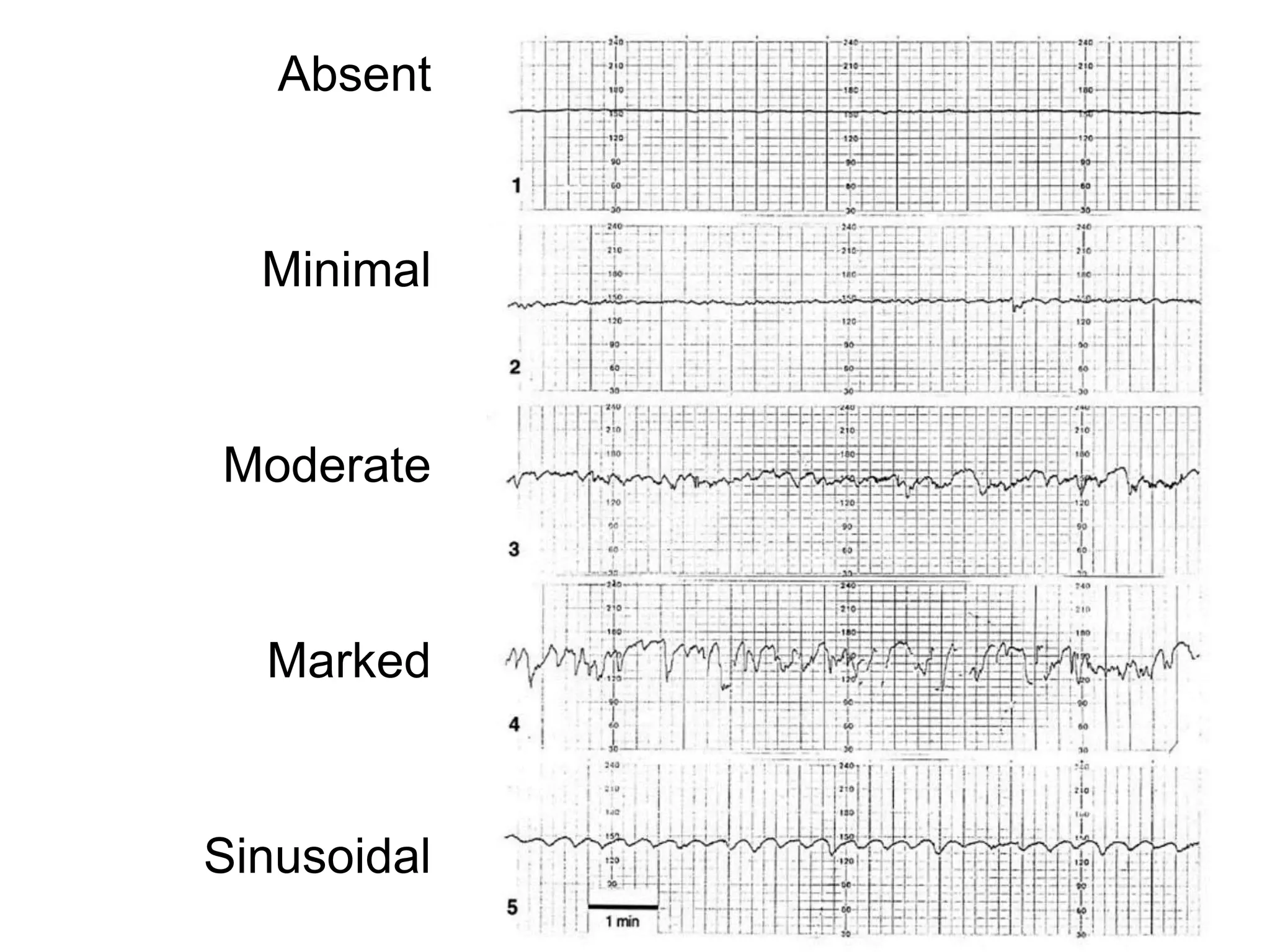
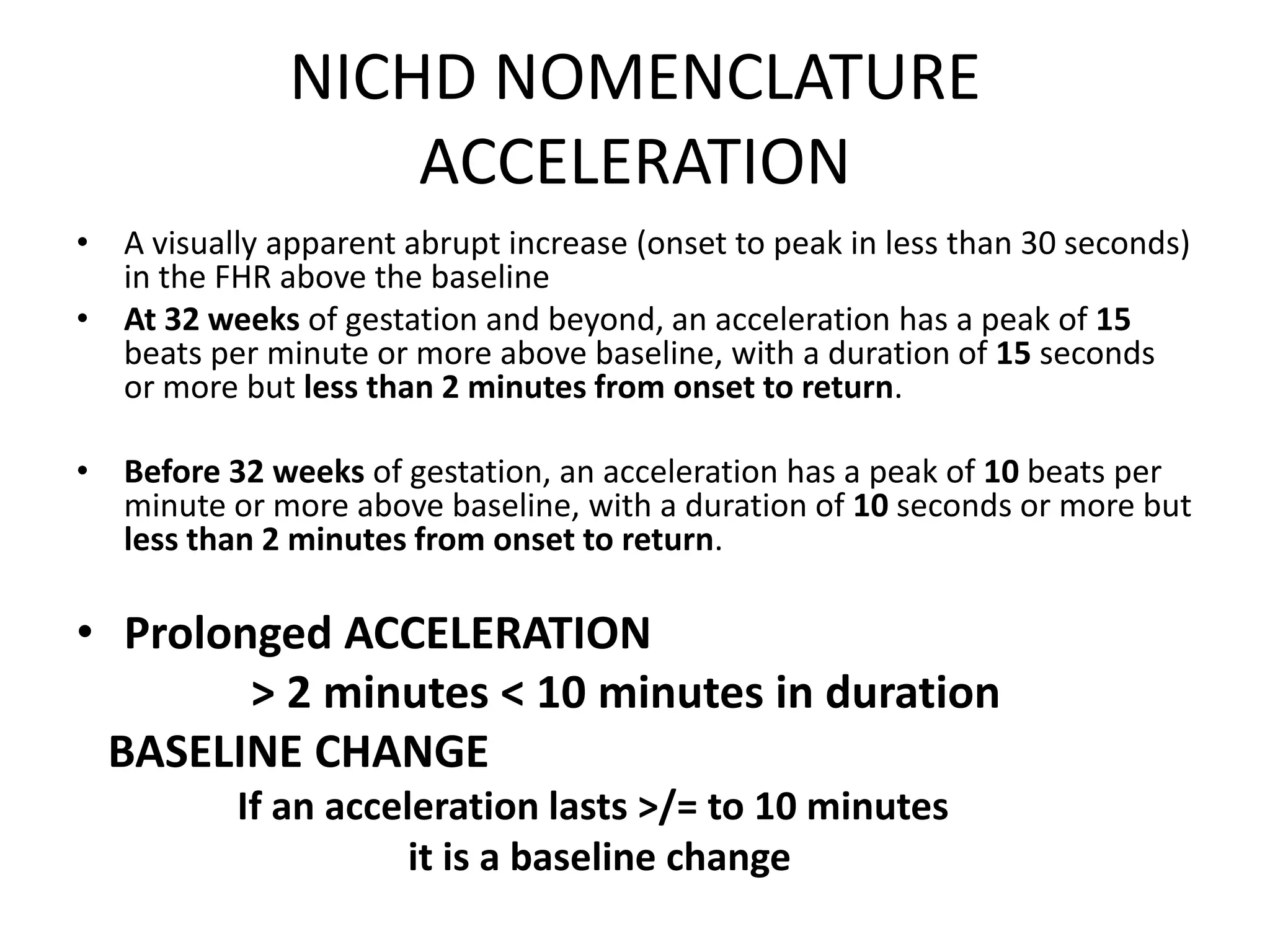
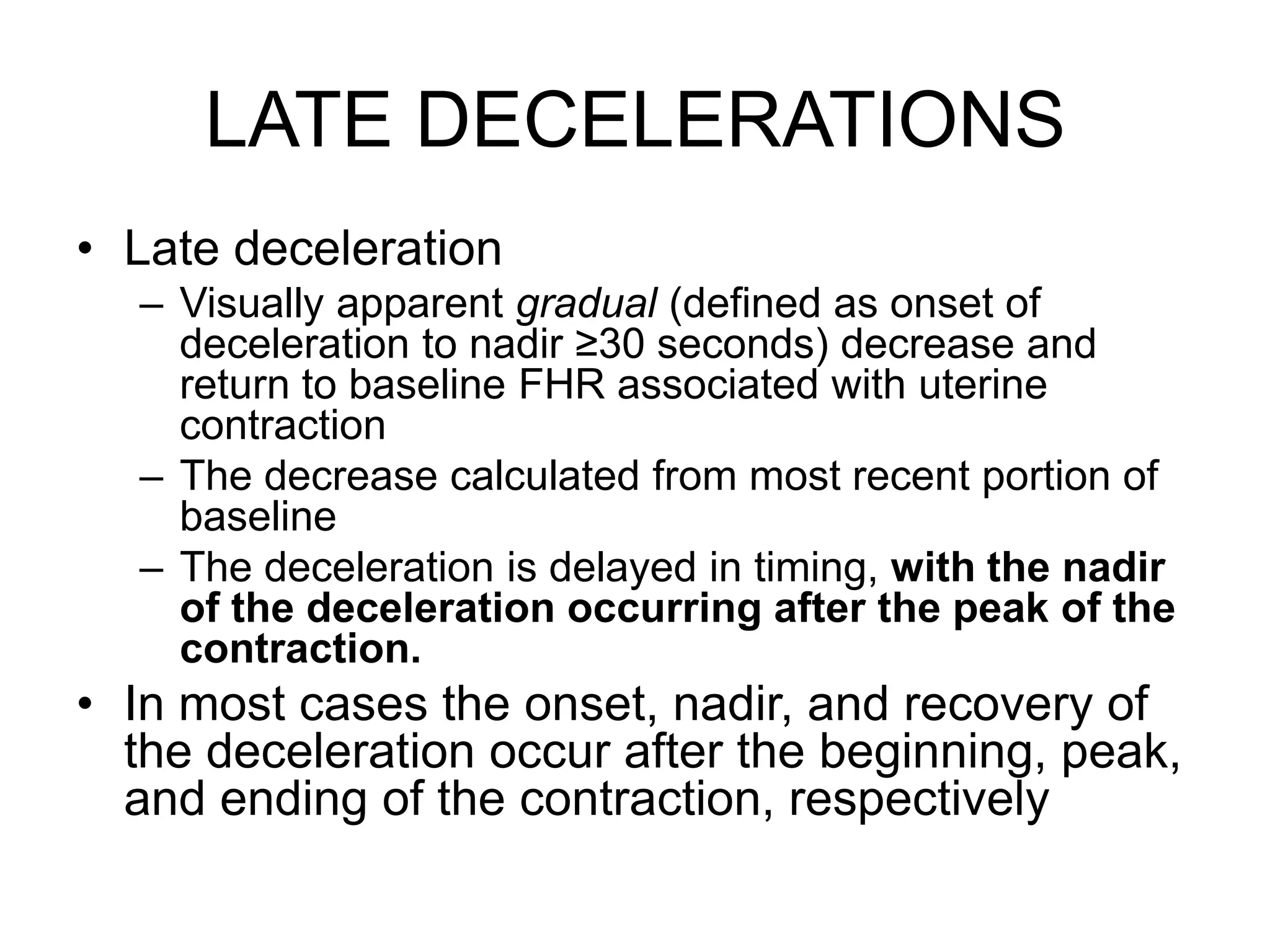
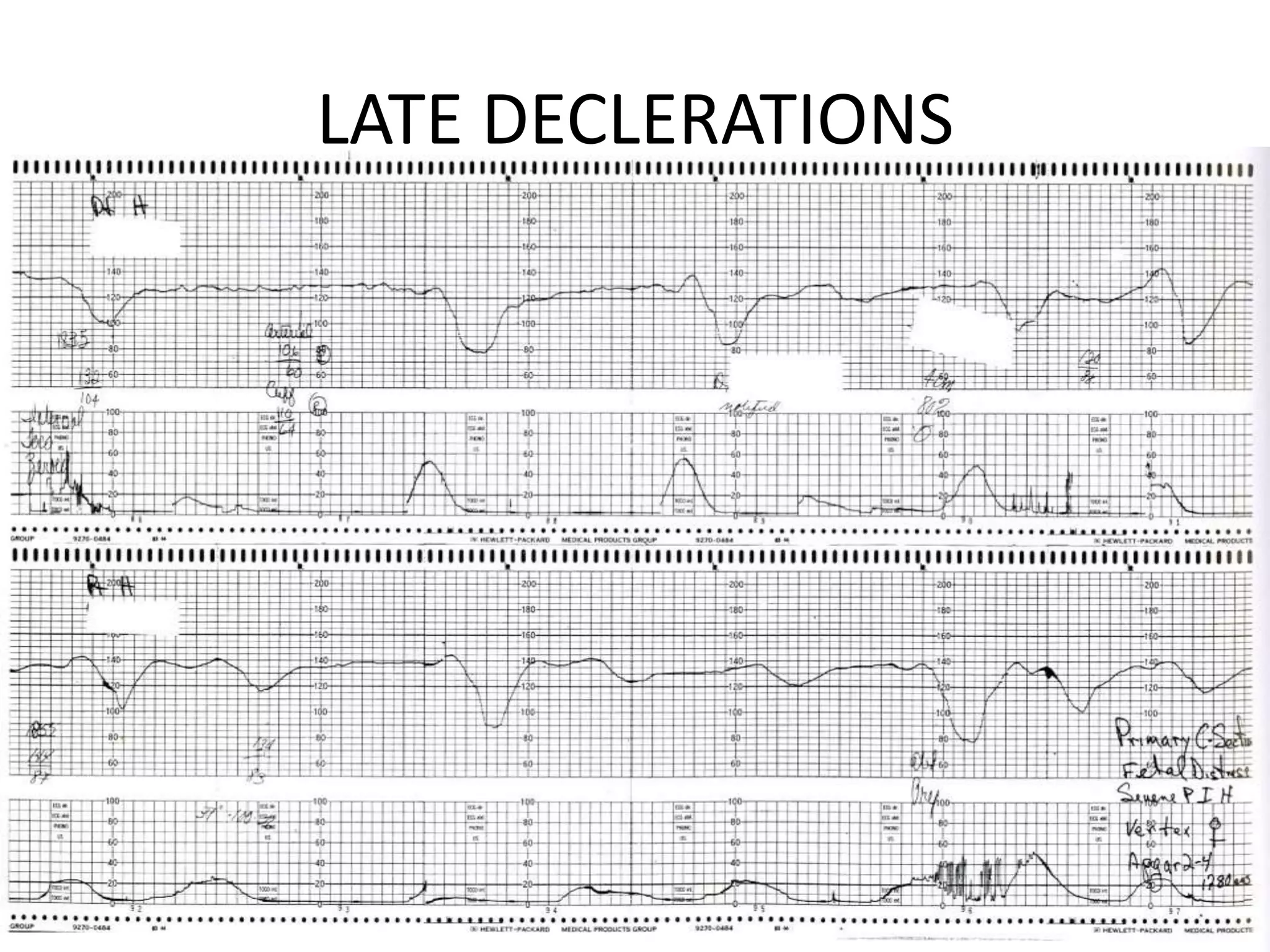
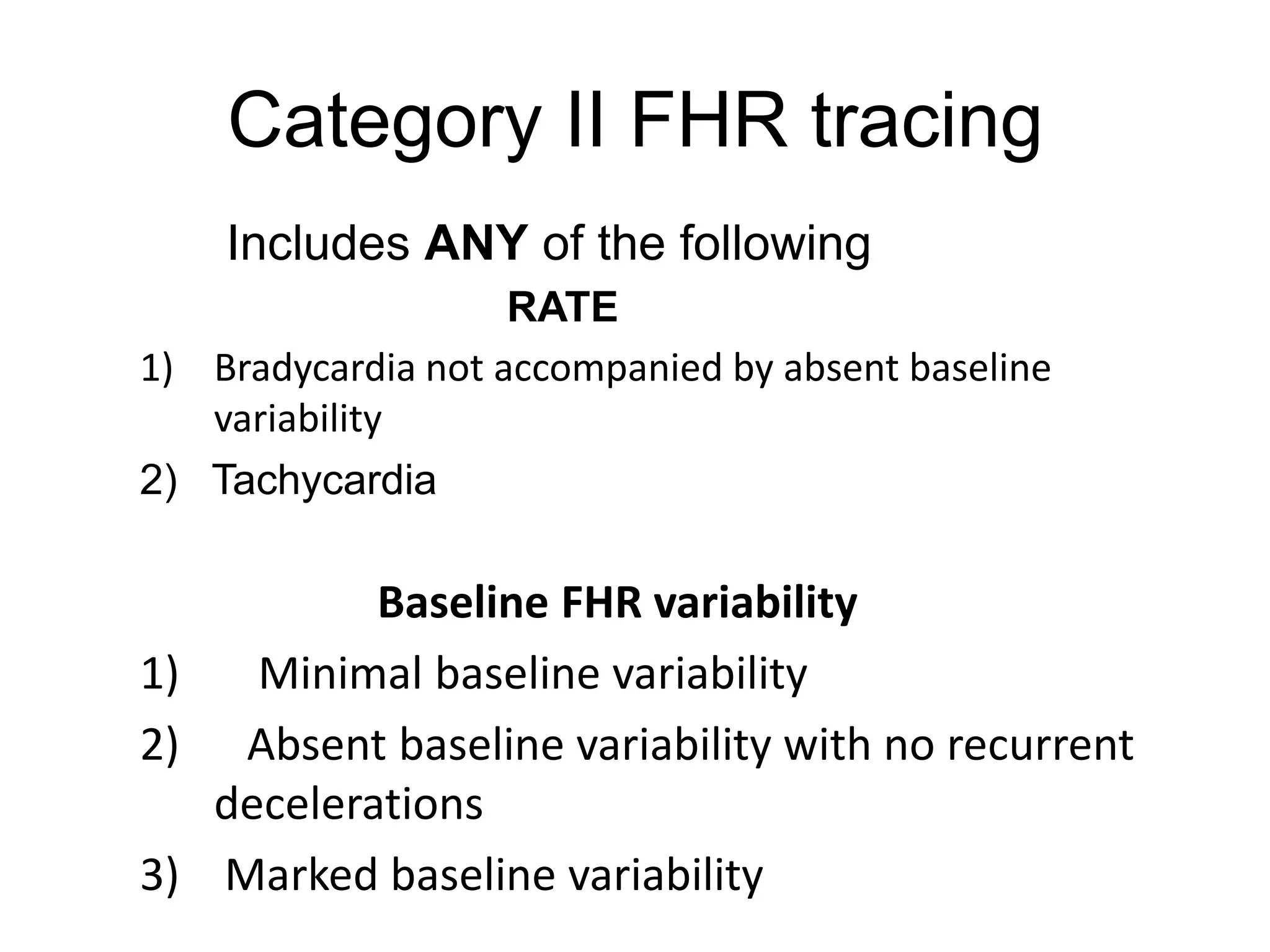
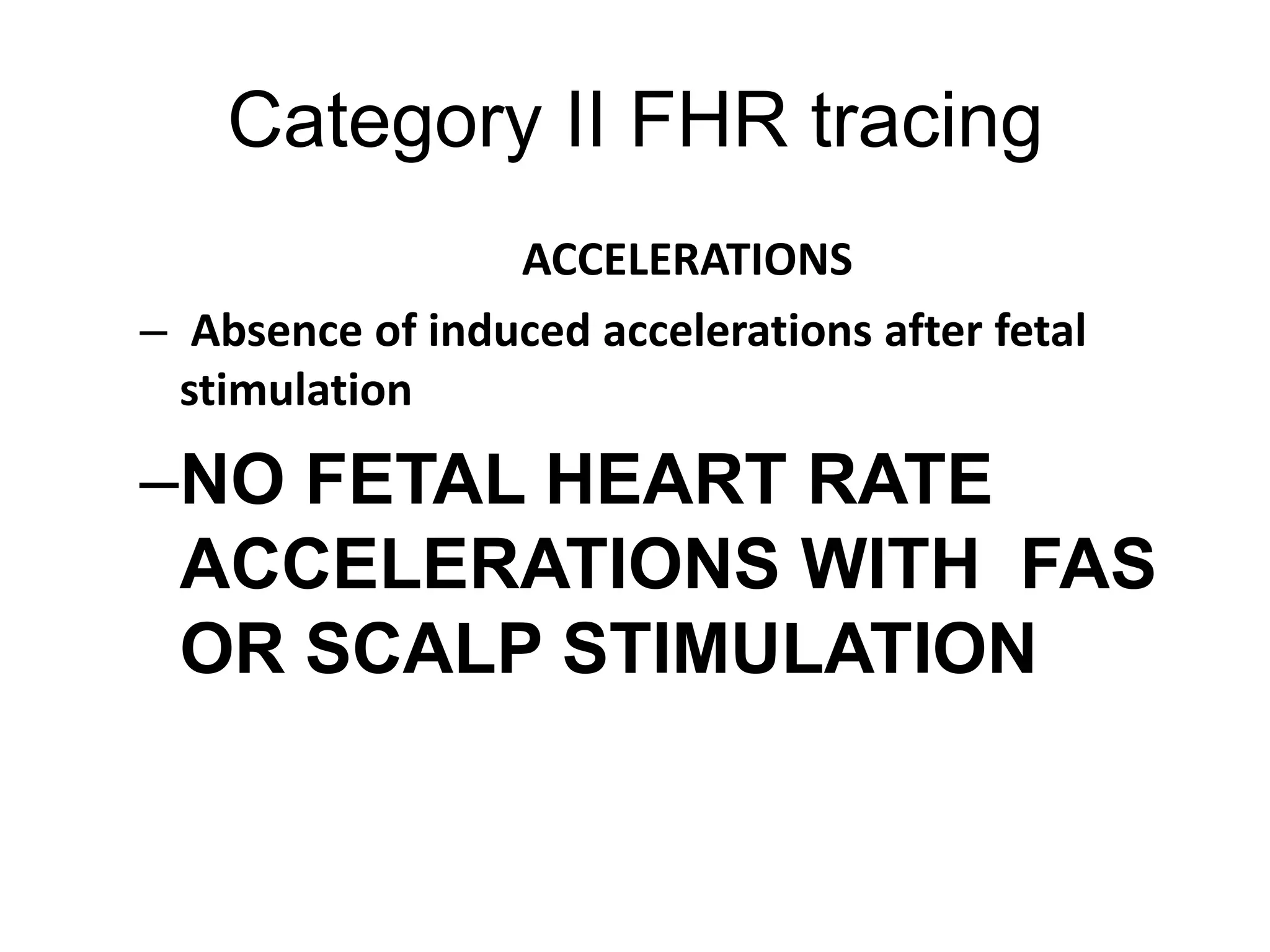
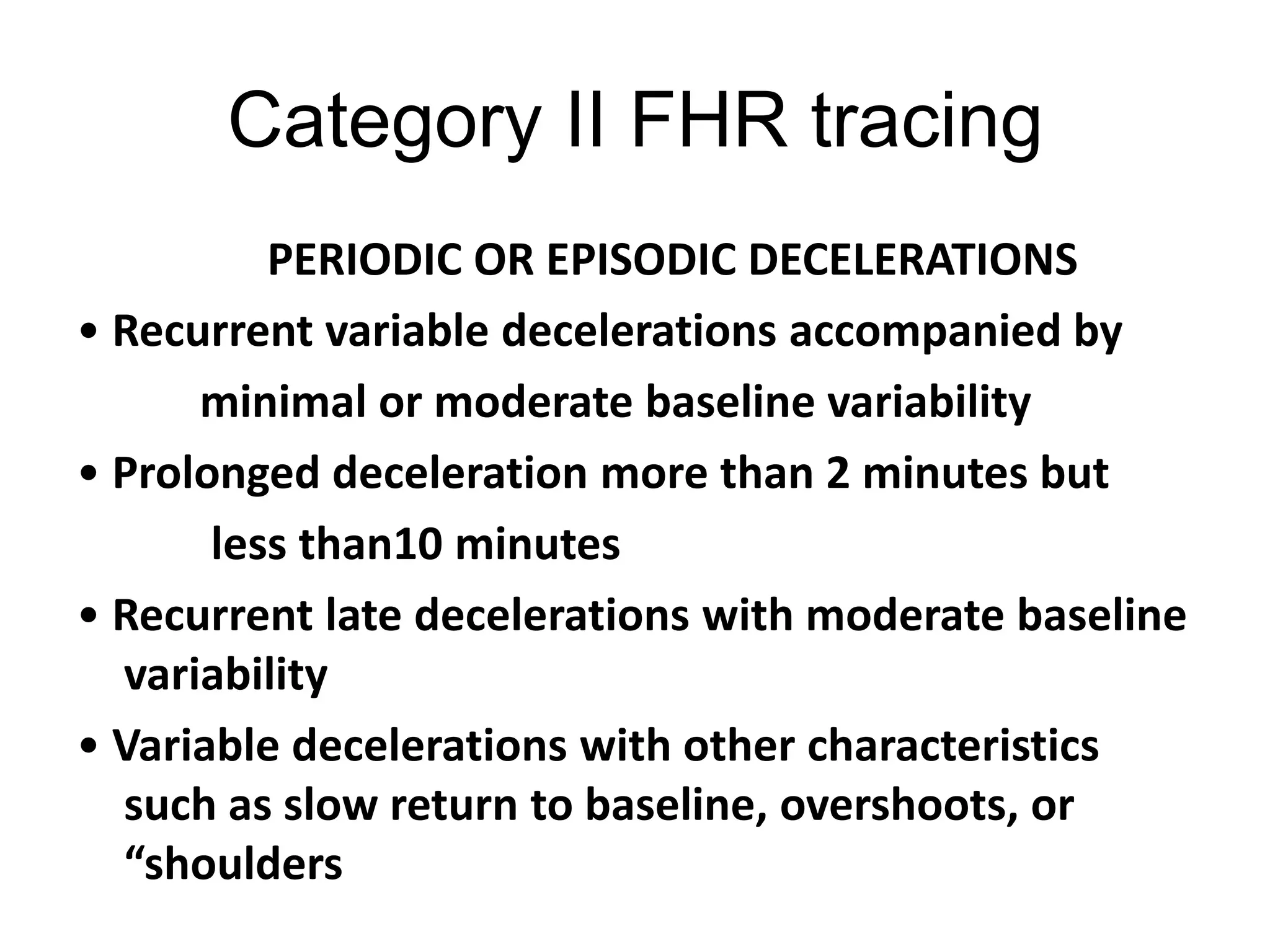
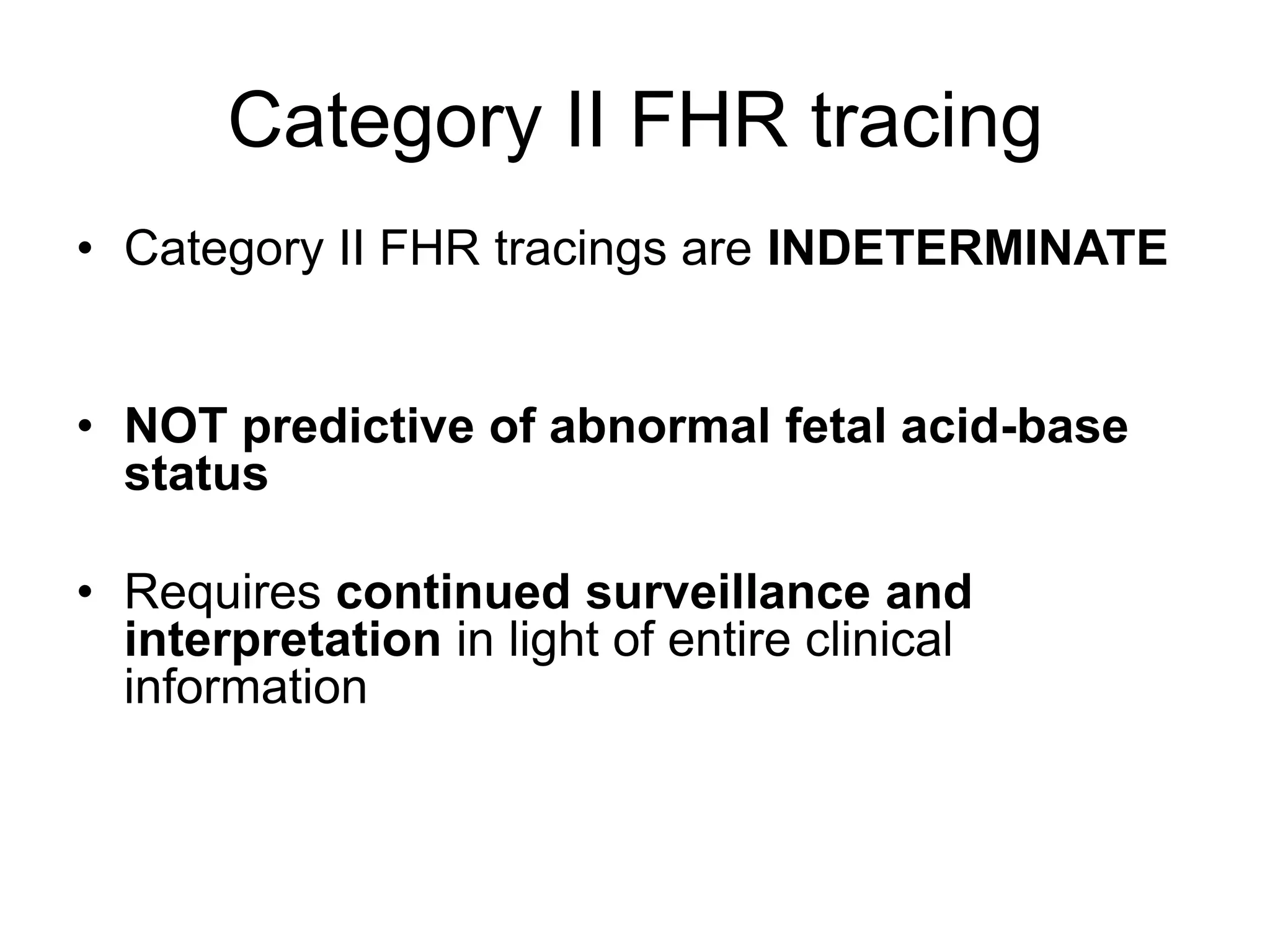
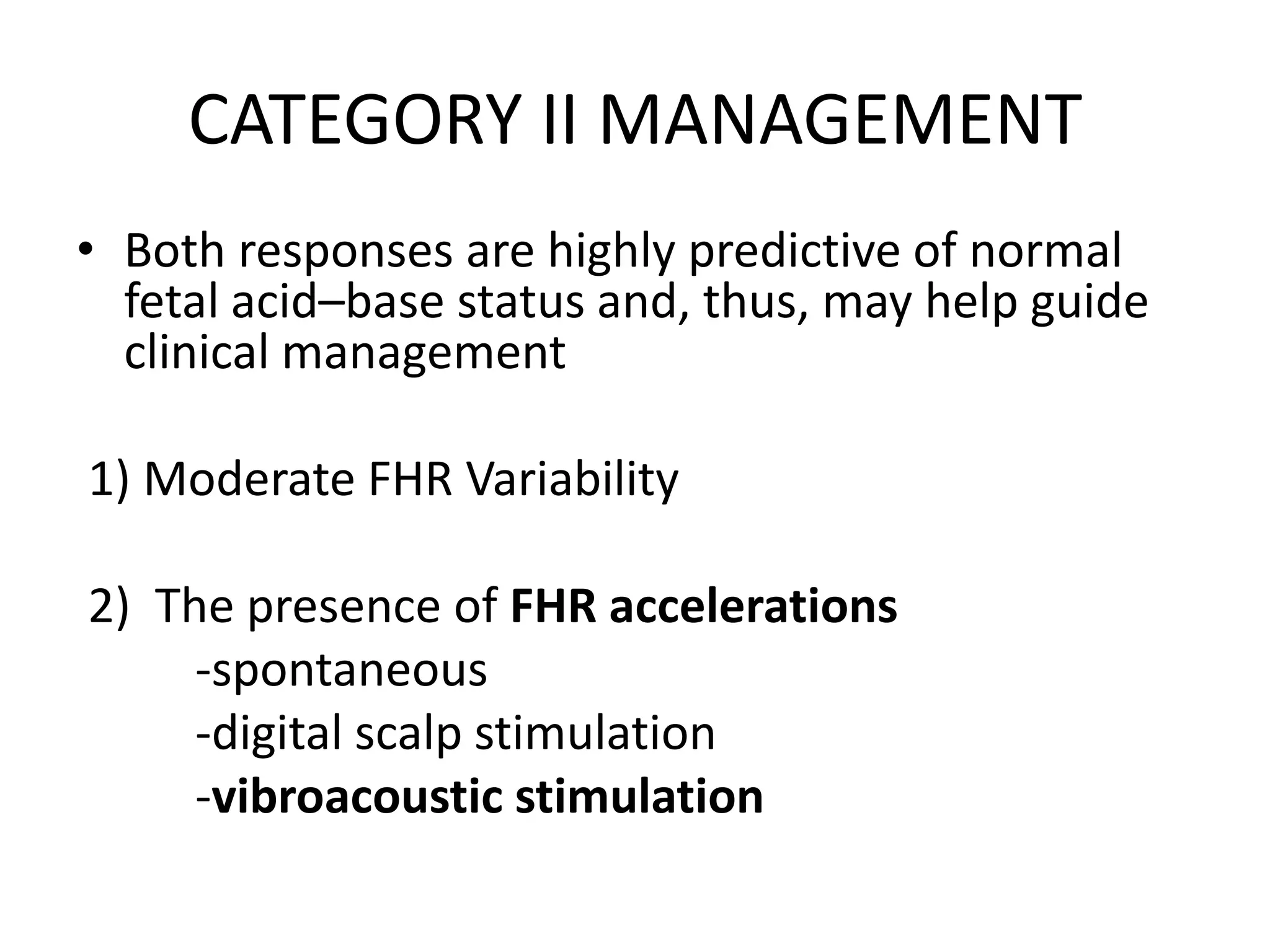
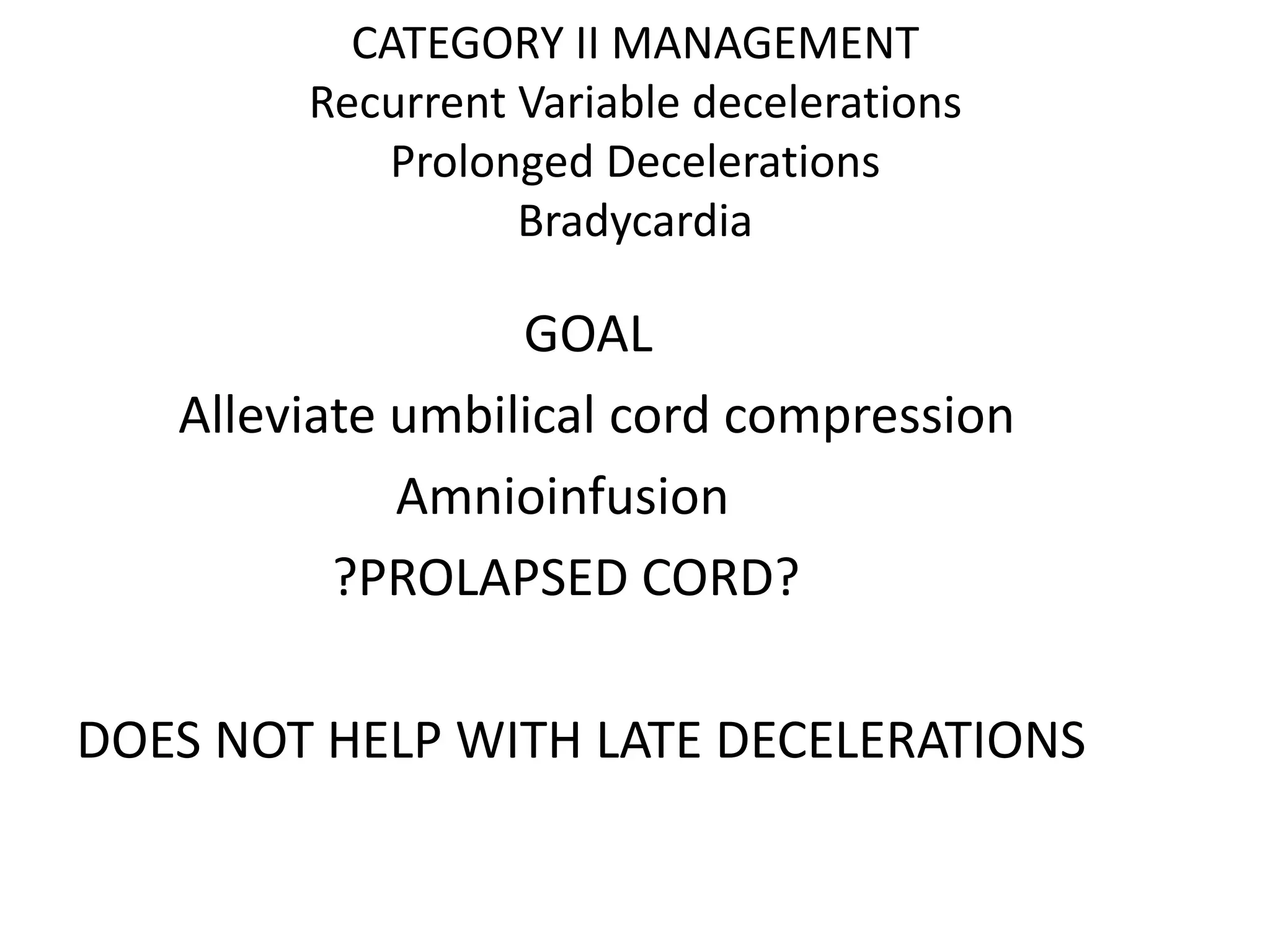
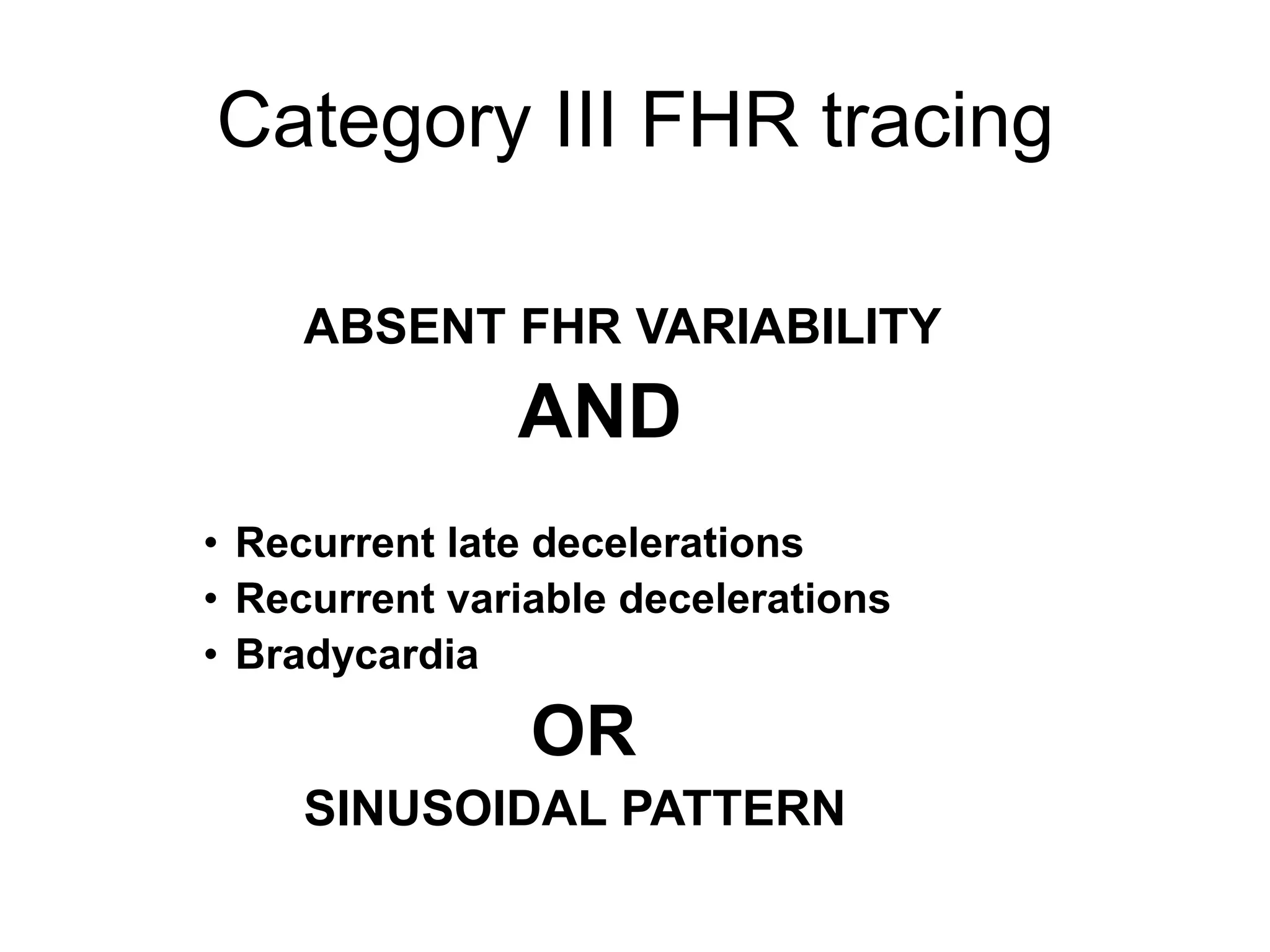
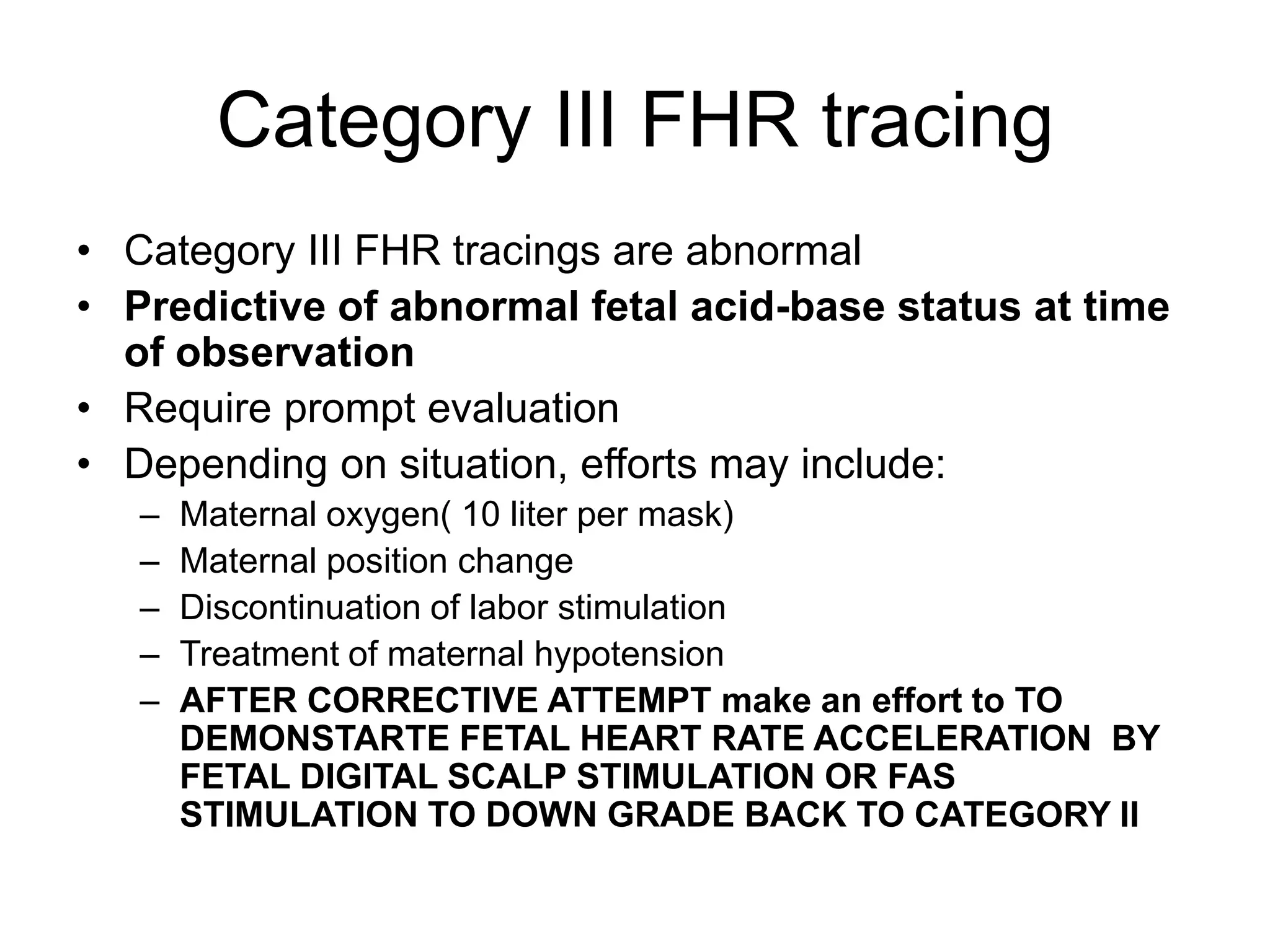
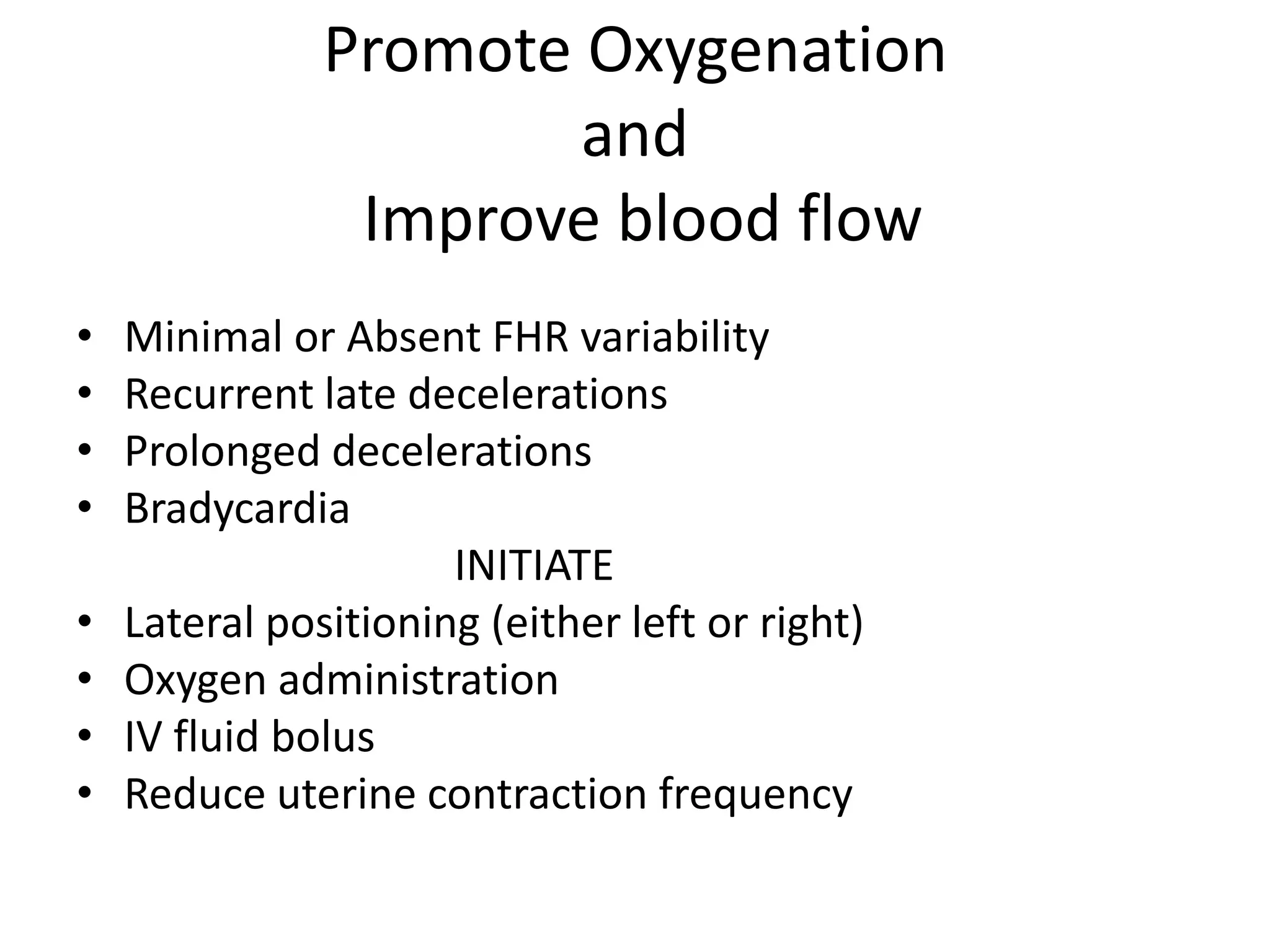
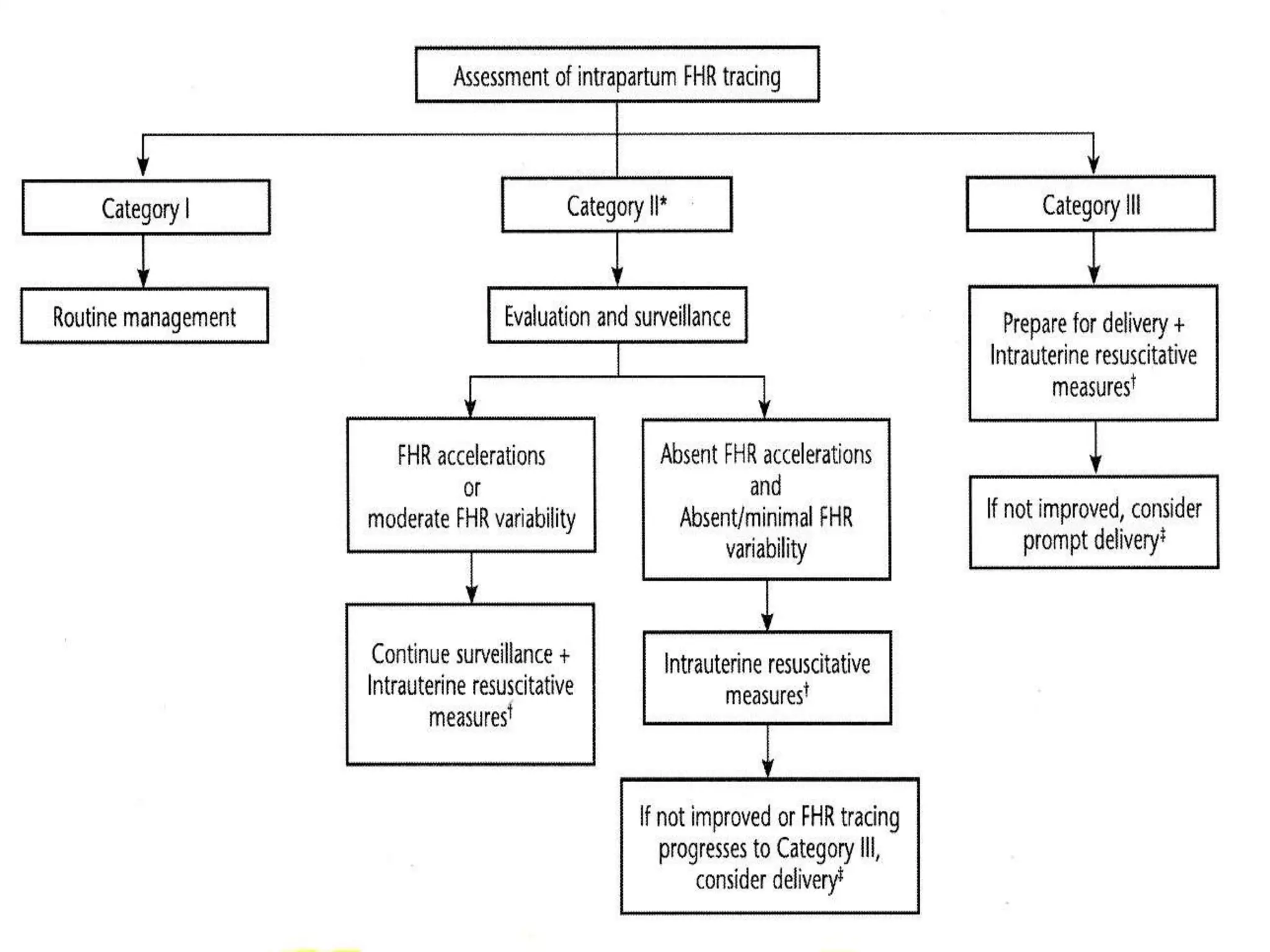
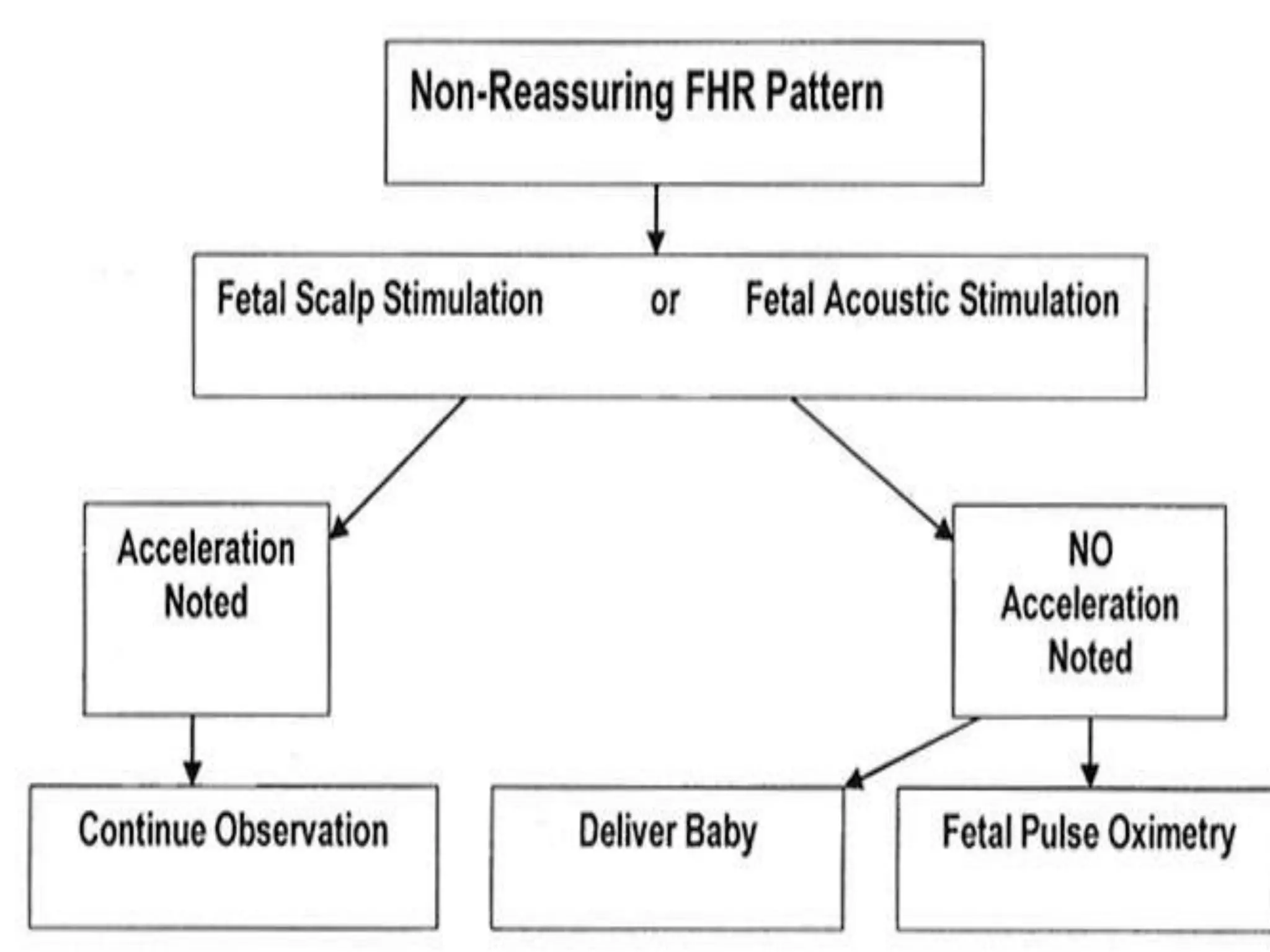
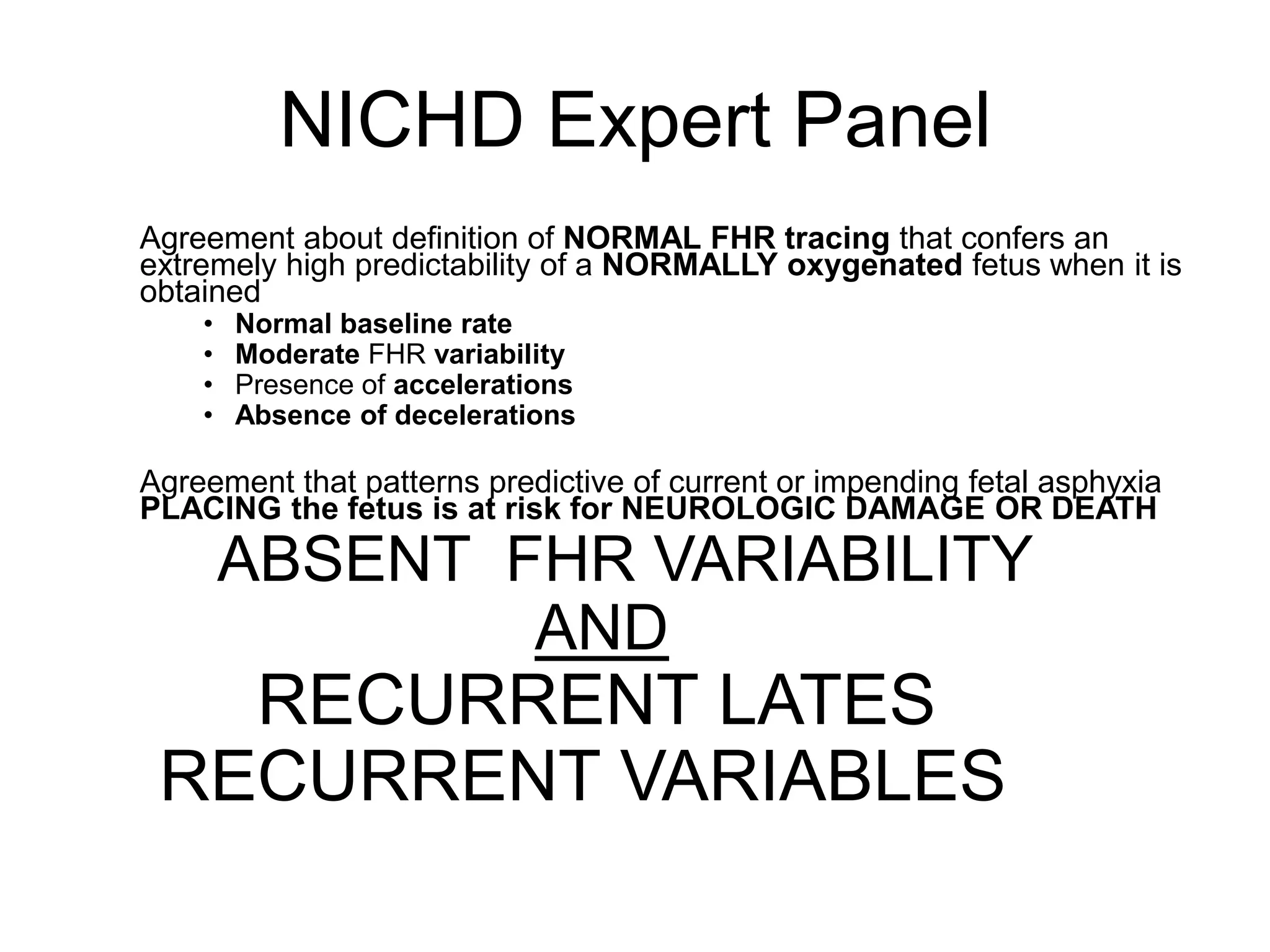
This document provides guidelines for the management and interpretation of intrapartum fetal heart rate tracings. It discusses important factors to consider when interpreting tracings such as gestational age, maternal conditions, and fetal conditions. It describes the physiology underlying different fetal heart rate patterns. It also presents the NICHD nomenclature for standardized description of tracings, including definitions for baseline rate, variability, accelerations, and decelerations. Tracings are categorized as Category I, II, or III based on patterns that reflect fetal acid-base status. Category I tracings are normal while Category III tracings indicate abnormal fetal status and need for prompt evaluation and treatment.