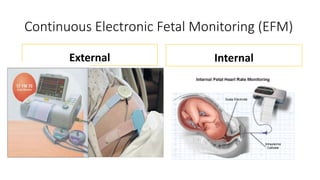
1) Intrapartum fetal heart rate monitoring via intermittent auscultation or continuous electronic fetal monitoring is used to determine if the fetus is well-oxygenated during labor and delivery.
2) Key components of electronic fetal monitoring include assessing the baseline heart rate, variability, presence of accelerations or decelerations.
3) Different patterns have different clinical significance, with a Category I pattern considered normal and low risk while a Category III pattern indicates abnormal tracings associated with an increased risk of hypoxia.