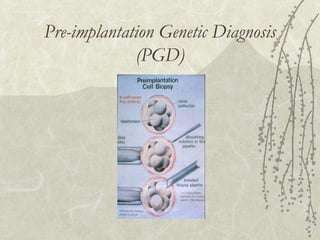
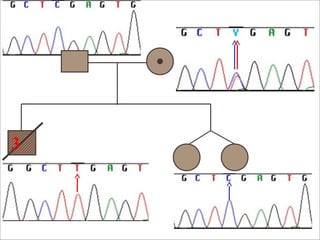
This document discusses genetic counseling and the prevention of genetic diseases. It describes genetic counseling as a process that helps people understand and adapt to the risks of genetic contributions to disease. The document outlines several methods for preventing genetic diseases, including genetic counseling, carrier detection in mothers, neonatal screening, pre-implantation genetic diagnosis, and family education. It provides details on the roles of genetic counselors and geneticists in helping diagnose genetic conditions and counsel families.