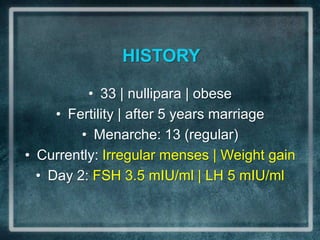
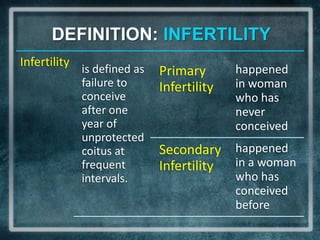
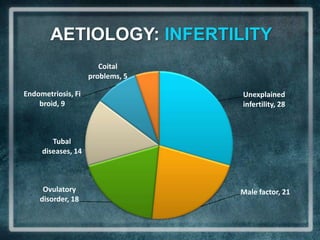
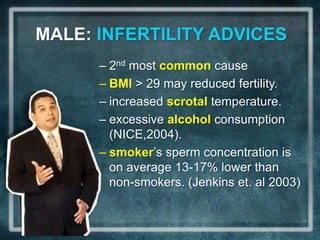
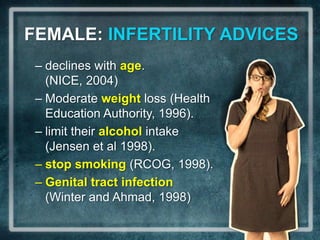
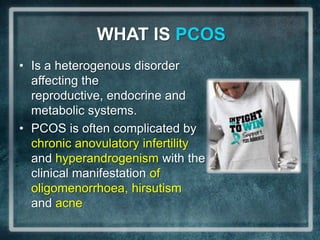
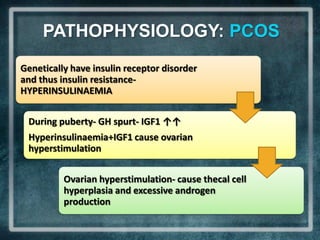
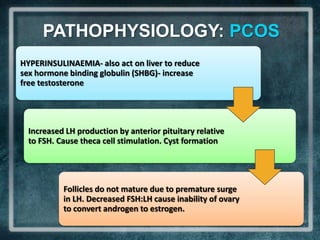
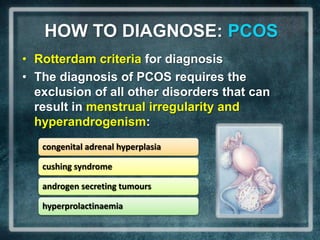
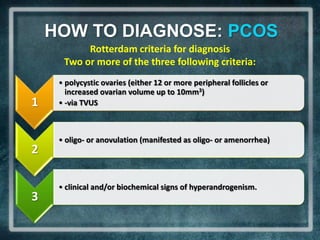
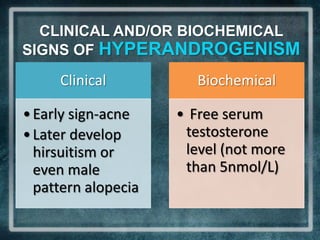
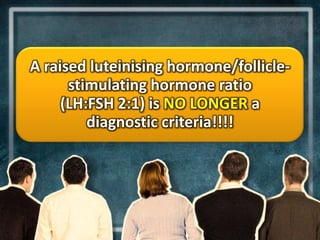
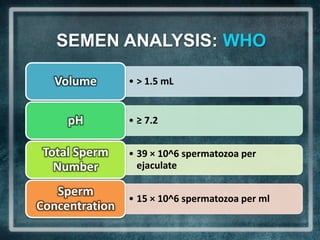
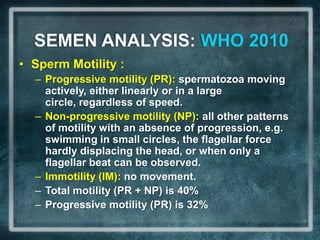
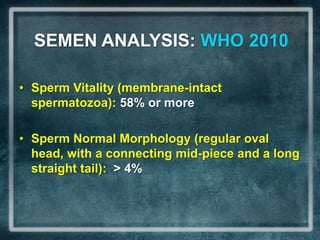
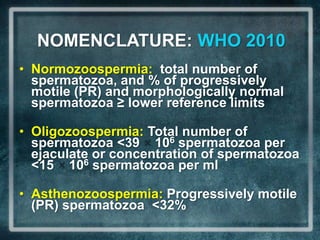
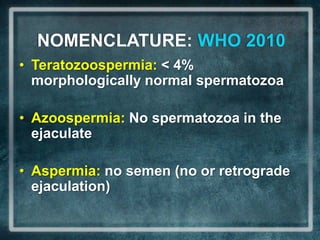
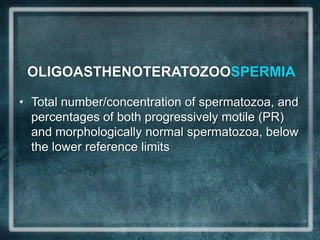
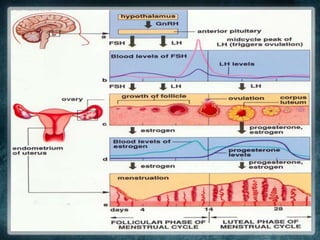
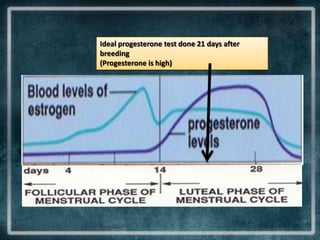
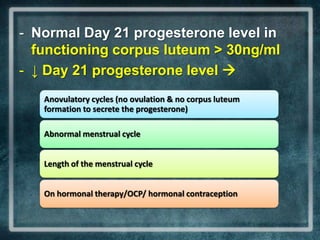
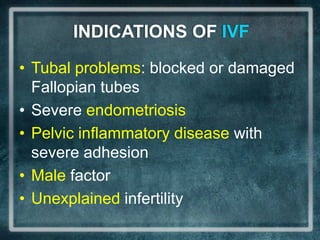
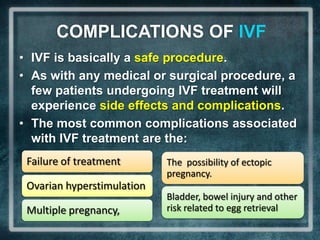
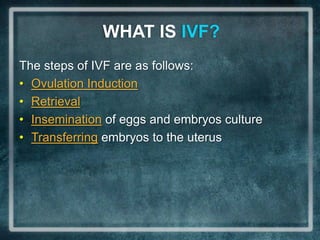
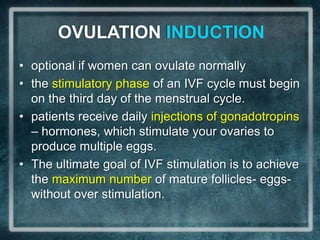
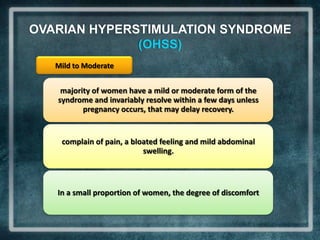
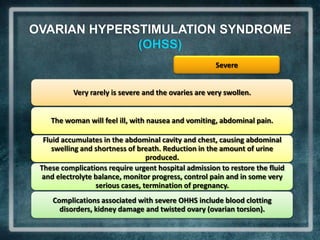
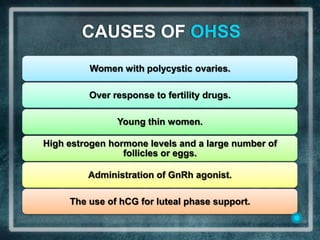
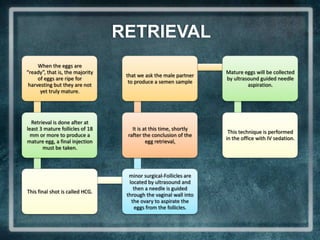
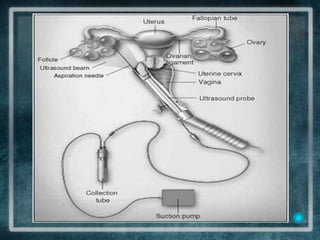
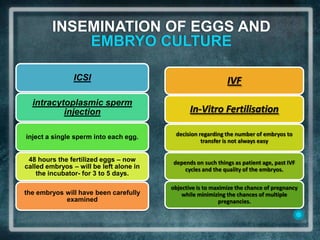
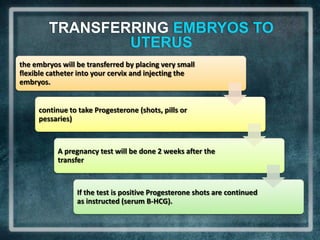
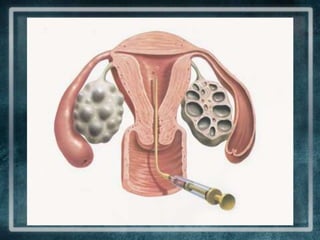
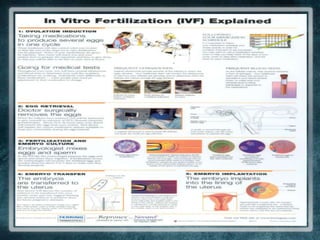
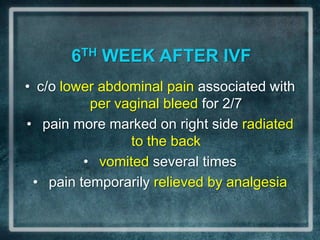
This document discusses a case of a 33-year-old nulliparous and obese woman presenting with infertility after 5 years of marriage. It defines infertility, discusses its etiologies including tubal disease, endovascular factors, and unexplained infertility. It also discusses lifestyle advice for improving fertility in males and females. The document then discusses polycystic ovarian syndrome (PCOS), describing its pathophysiology, diagnostic criteria using Rotterdam criteria, and clinical and biochemical signs of hyperandrogenism. It also discusses scenarios involving male factor infertility and use of ovarian stimulation and IVF.