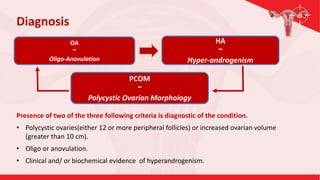
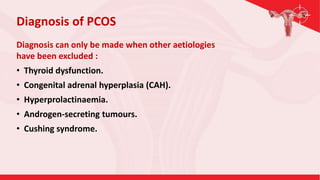
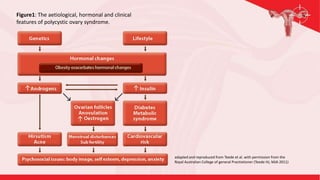
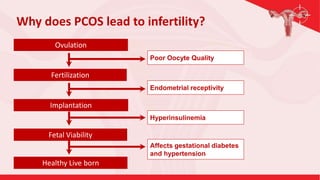
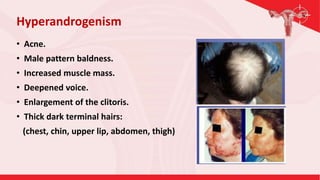
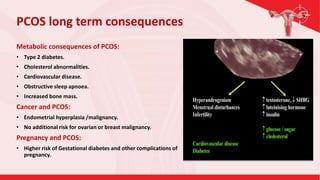
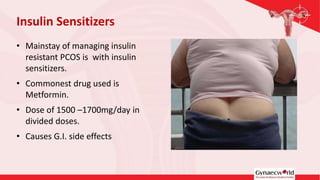
Polycystic Ovary Syndrome (PCOS) is a major health problem affecting women of reproductive age. It is diagnosed when a woman has two of three criteria - polycystic ovaries, irregular periods, and high androgen levels. Treatment focuses on lifestyle changes like weight loss and exercise to reduce insulin resistance and improve fertility outcomes. Medications may also be used to treat symptoms and help induce ovulation. A multidisciplinary approach is often needed to manage PCOS and its long term health consequences.