The document provides information about lumbar puncture and CSF analysis. It defines a lumbar puncture as inserting a needle into the spinal canal to obtain CSF samples. Key points include:
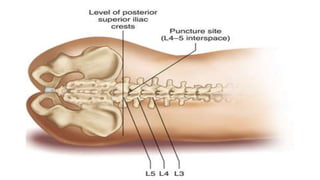
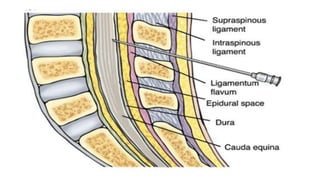
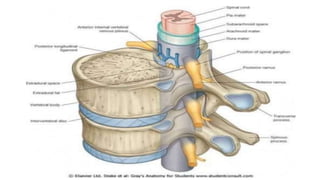
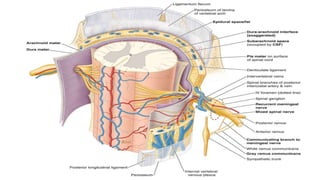
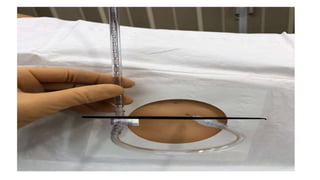
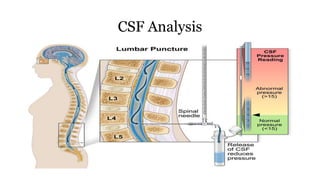
- Lumbar puncture is done between the L3 and L4 vertebrae under local anesthetic to obtain CSF for analysis or inject medications.
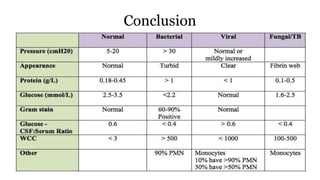
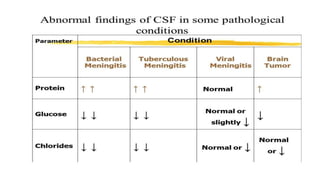
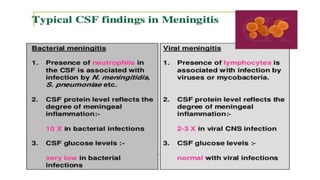
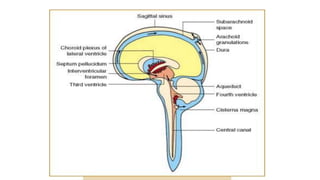
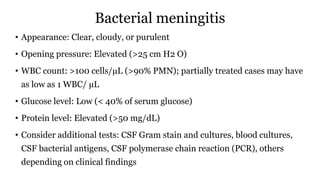
- CSF samples are analyzed to detect conditions like meningitis, tumors, or infections by examining appearance, pressure, cell count, glucose, and protein levels.
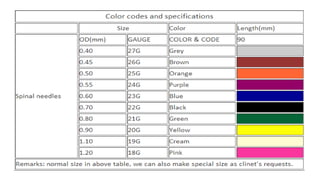
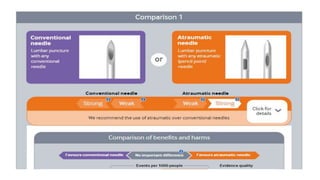
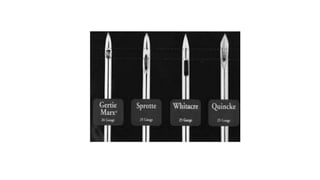
- Complications are rare but include headache, nerve damage, or infection. Smaller needles and atraumatic needles reduce risks.
- Nursing considerations involve proper patient positioning, encouraging hydration before and after, and keeping the patient
![Research evidence
• The smaller the needle used for the lumbar puncture, the lower the
risk that the patient will experience a post–lumbar puncture
headache. Data suggest an inverse linear relation between needle
gauge and headache incidence, and some authors recommend using
a 22-gauge needle regardless of what size needle is supplied with the
kit.
• Lambert DH, Hurley RJ, Hertwig L, Datta S. Role of needle gauge and tip configuration in the production
of lumbar puncture headache. Reg Anesth. 1997 Jan-Feb. 22(1):66-72. [Medline].](https://image.slidesharecdn.com/lpcsfanalysis-210806045753/85/Lumbar-puncture-and-CSF-Analysis-24-320.jpg)

![Research evidence cont..
• The use of atraumatic needles has been shown to significantly
reduce the incidence of post–lumbar puncture headache (3%) when
compared to the use of standard spinal needles (approximately
30%). In addition, it may lead to cost savings. However, obtaining
pressures can be more difficult with atraumatic needles.
• Lavi R, Yarnitsky D, Yernitzky D, Rowe JM, Weissman A, Segal D. Standard vs atraumatic Whitacre
needle for diagnostic lumbar puncture: a randomized trial. Neurology. 2006 Oct 24. 67(8):1492-4.
[Medline].](https://image.slidesharecdn.com/lpcsfanalysis-210806045753/85/Lumbar-puncture-and-CSF-Analysis-27-320.jpg)

![Normal results in adults
• Appearance: Clear
• Opening pressure: 10-20 cm H2 O
• WBC count: 0-5 cells/µL (< 2 polymorphonucleocytes [PMN]);
normal cell counts do not rule out meningitis or any other pathology
• Glucose level: >60% of serum glucose
• Protein level: < 45 mg/dL](https://image.slidesharecdn.com/lpcsfanalysis-210806045753/85/Lumbar-puncture-and-CSF-Analysis-33-320.jpg)
![Aseptic (viral) meningitis
• Appearance: Clear
• Opening pressure: Normal or elevated
• WBC count: 10-1000 cells/µL (lymph but PMN early)
• Glucose level: >60% serum glucose (may be low in HSV infection)
• Protein level: Elevated (>50 mg/dL)
• Consider additional tests: CSF Gram stain and cultures, blood cultures, CSF
bacterial antigens, CSF PCR (eg, herpes simplex virus [HSV], varicella-
zoster virus [VZV]), others depending on clinical findings](https://image.slidesharecdn.com/lpcsfanalysis-210806045753/85/Lumbar-puncture-and-CSF-Analysis-35-320.jpg)