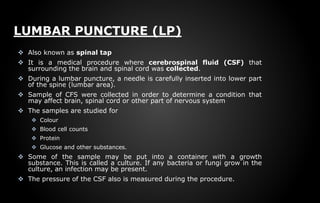
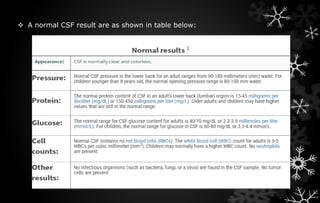
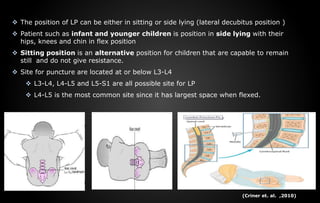
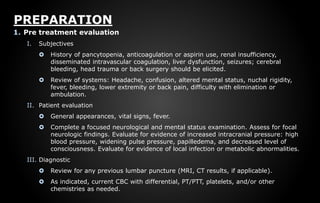
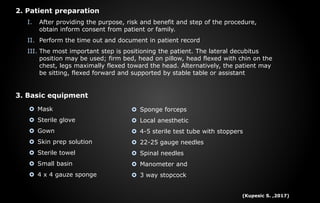
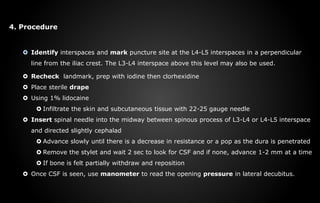
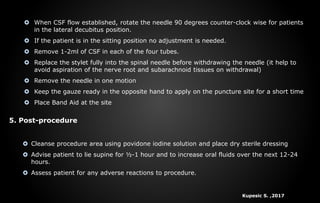
A lumbar puncture, or spinal tap, is a medical procedure for collecting cerebrospinal fluid (CSF) from the lower spine to diagnose conditions affecting the brain and nervous system. Indications include diagnosing CNS infections, cancer, and bleeding, while contraindications include increased intracranial pressure and coagulation disorders. The procedure involves careful positioning, skin preparation, and insertion of a spinal needle to collect CSF, followed by post-procedure care to monitor for complications.