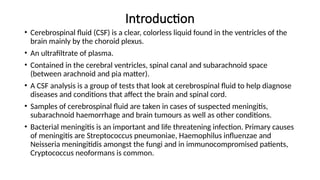
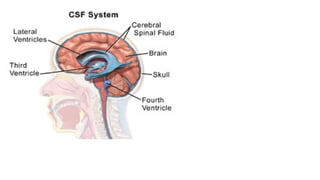
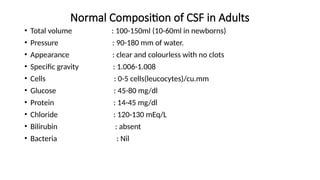
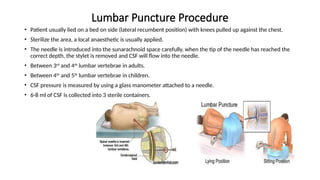
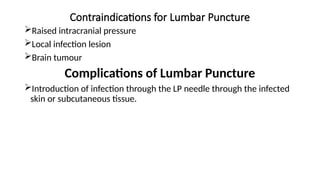
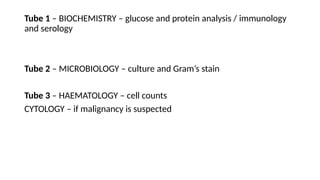
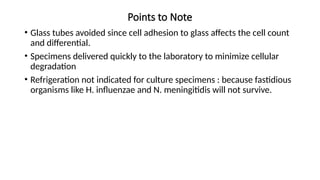
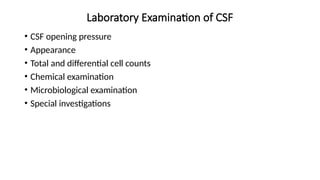
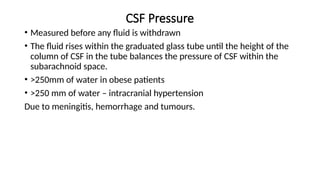
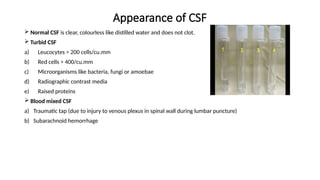
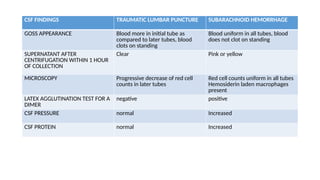
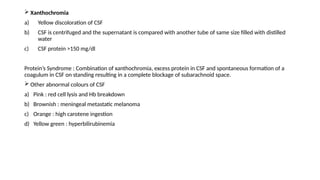
This document provides a comprehensive overview of cerebrospinal fluid (CSF), including its functions, normal composition, collection methods, and indications for analysis. It details the lumbar puncture procedure for CSF collection and highlights the diagnostic value in various diseases such as meningitis, brain tumors, and spinal conditions. Additionally, it discusses laboratory examination procedures and the significance of CSF appearance and composition in diagnosing medical conditions.