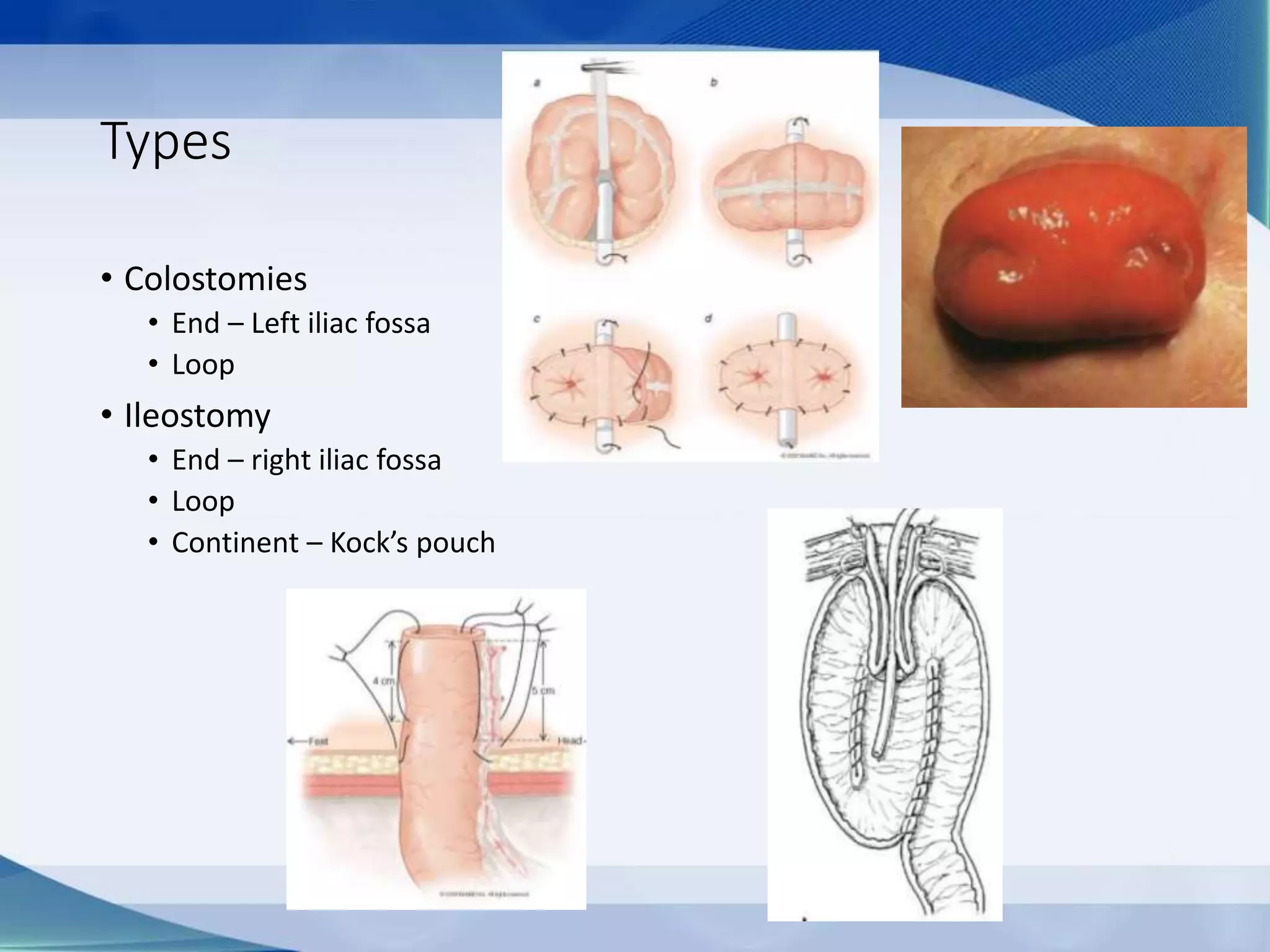
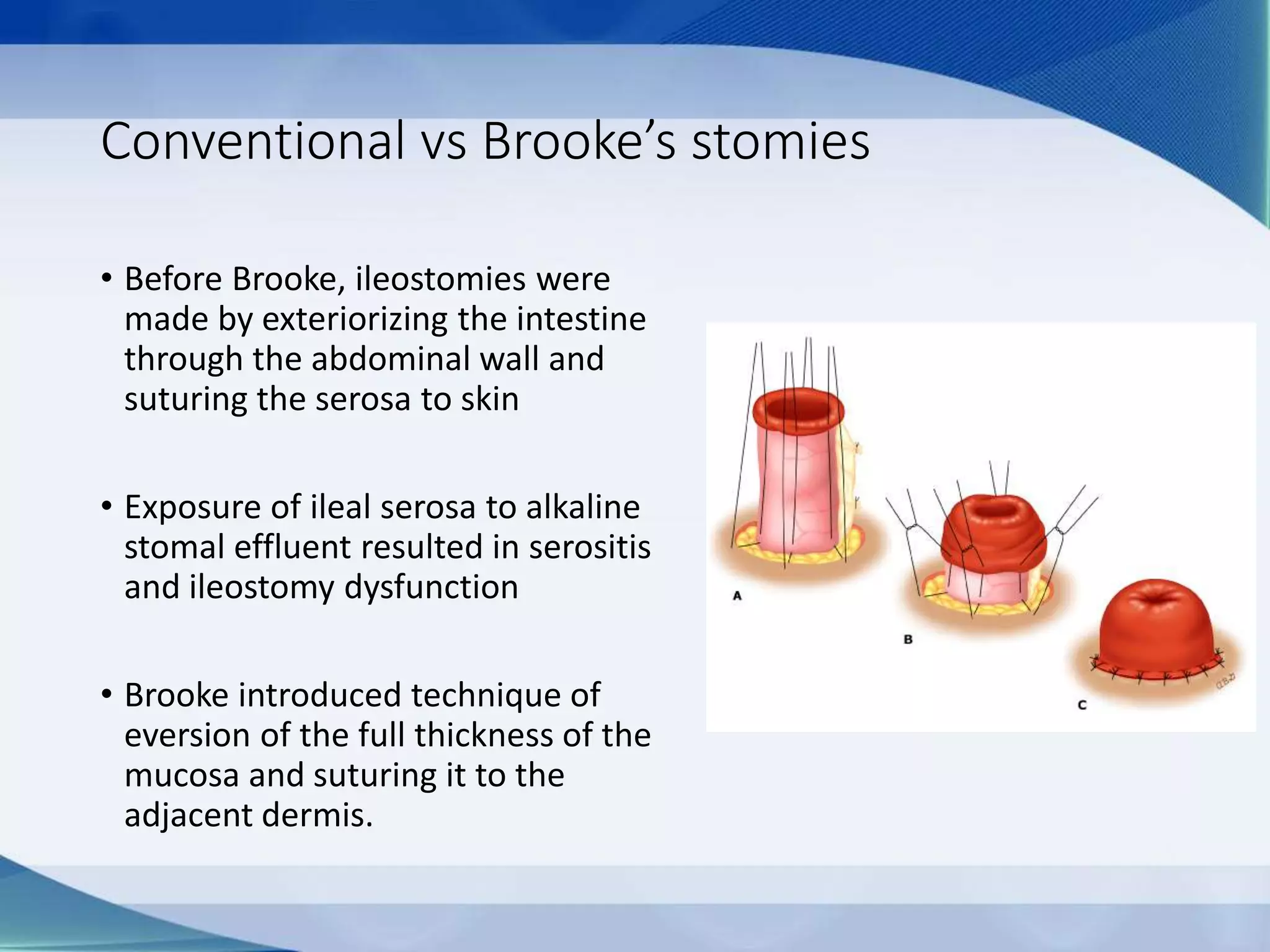
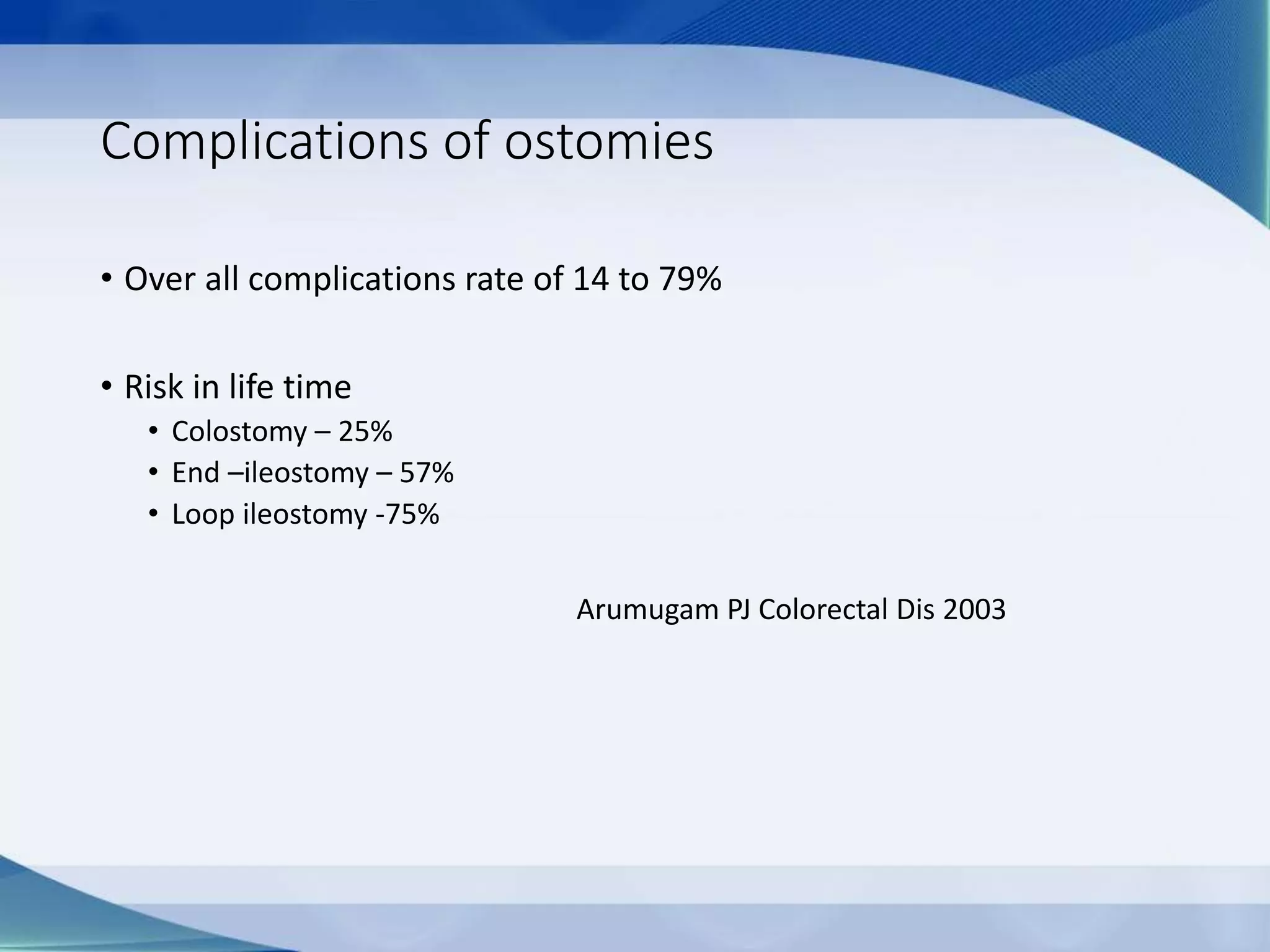
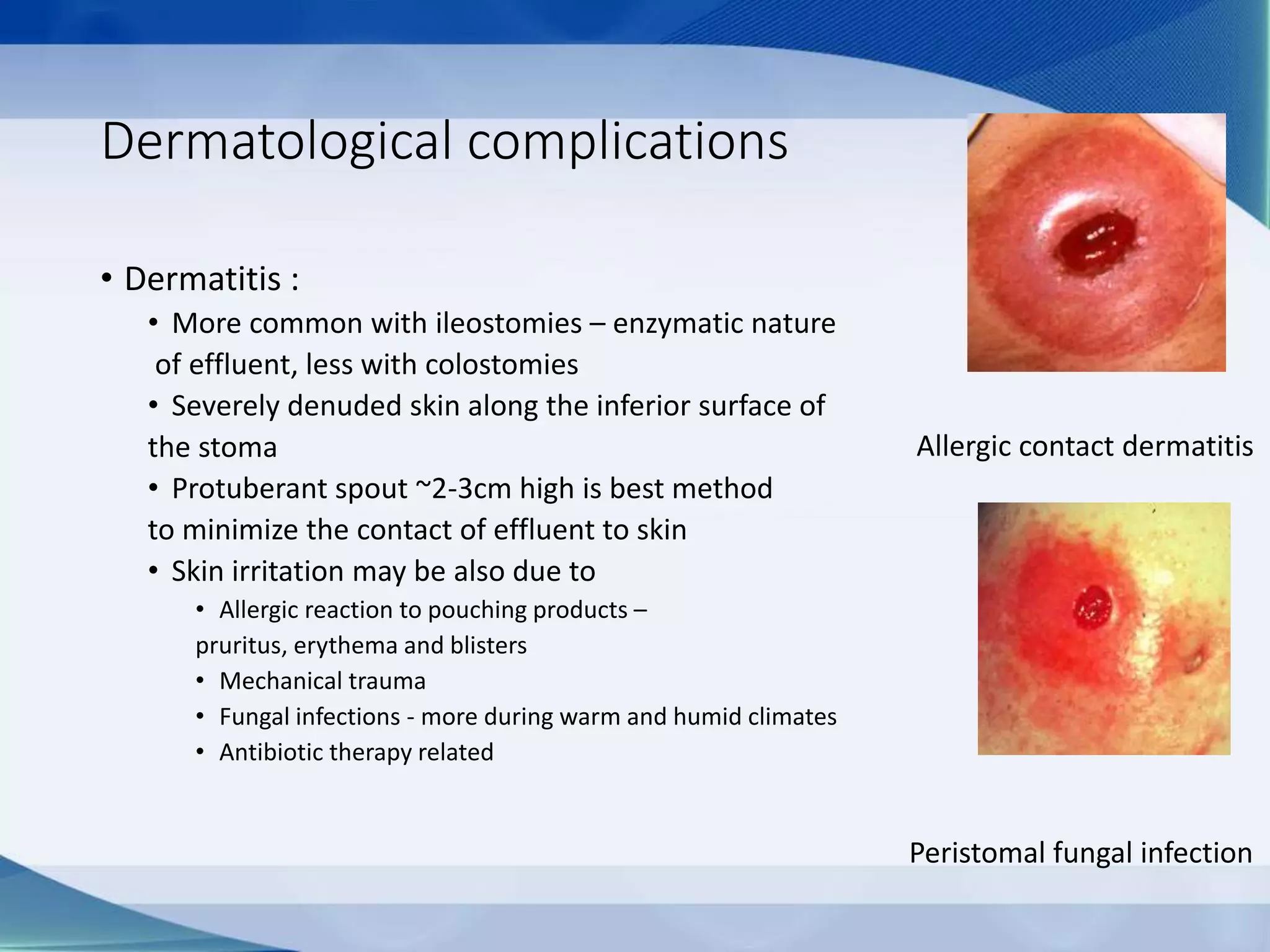
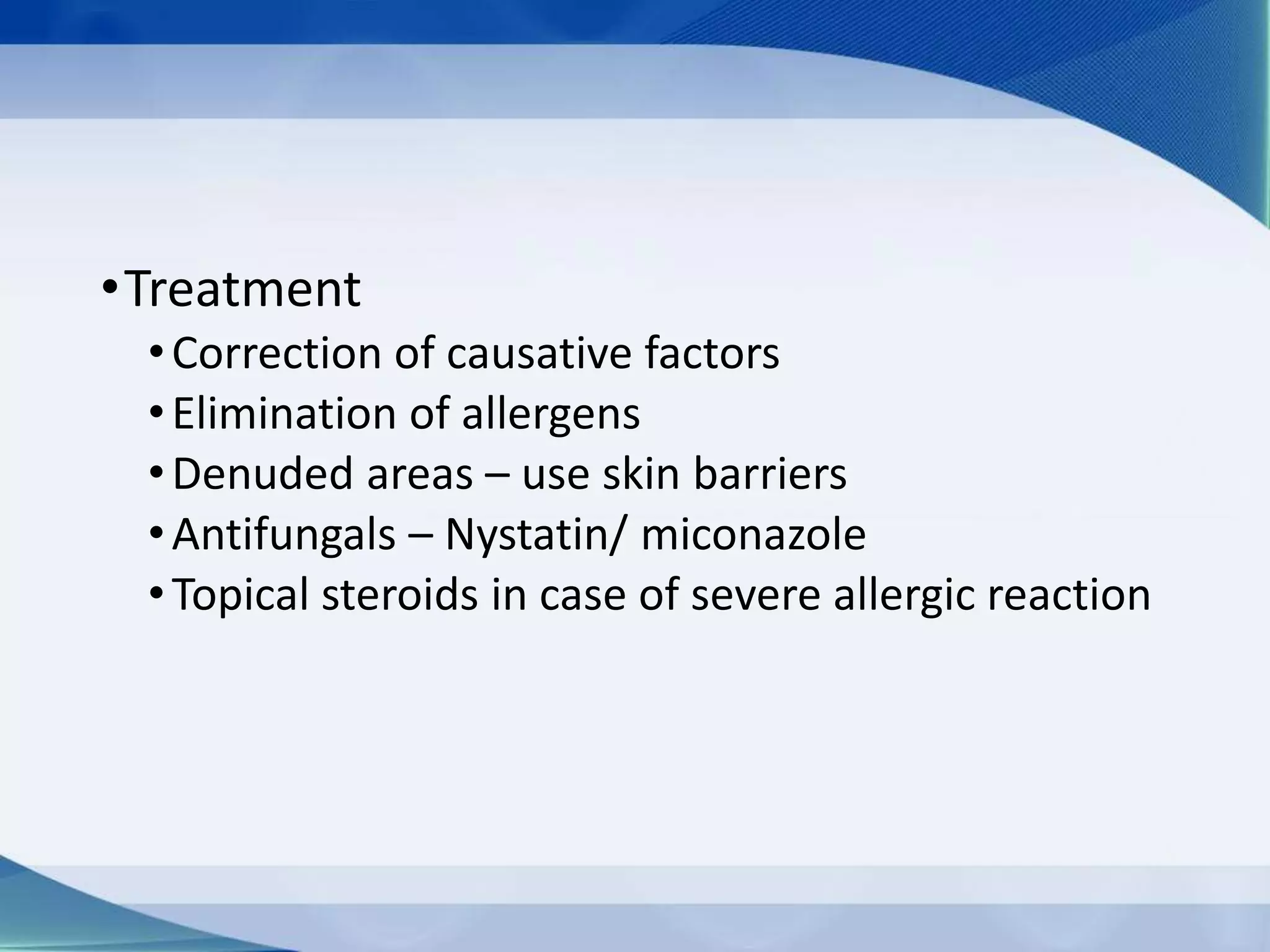
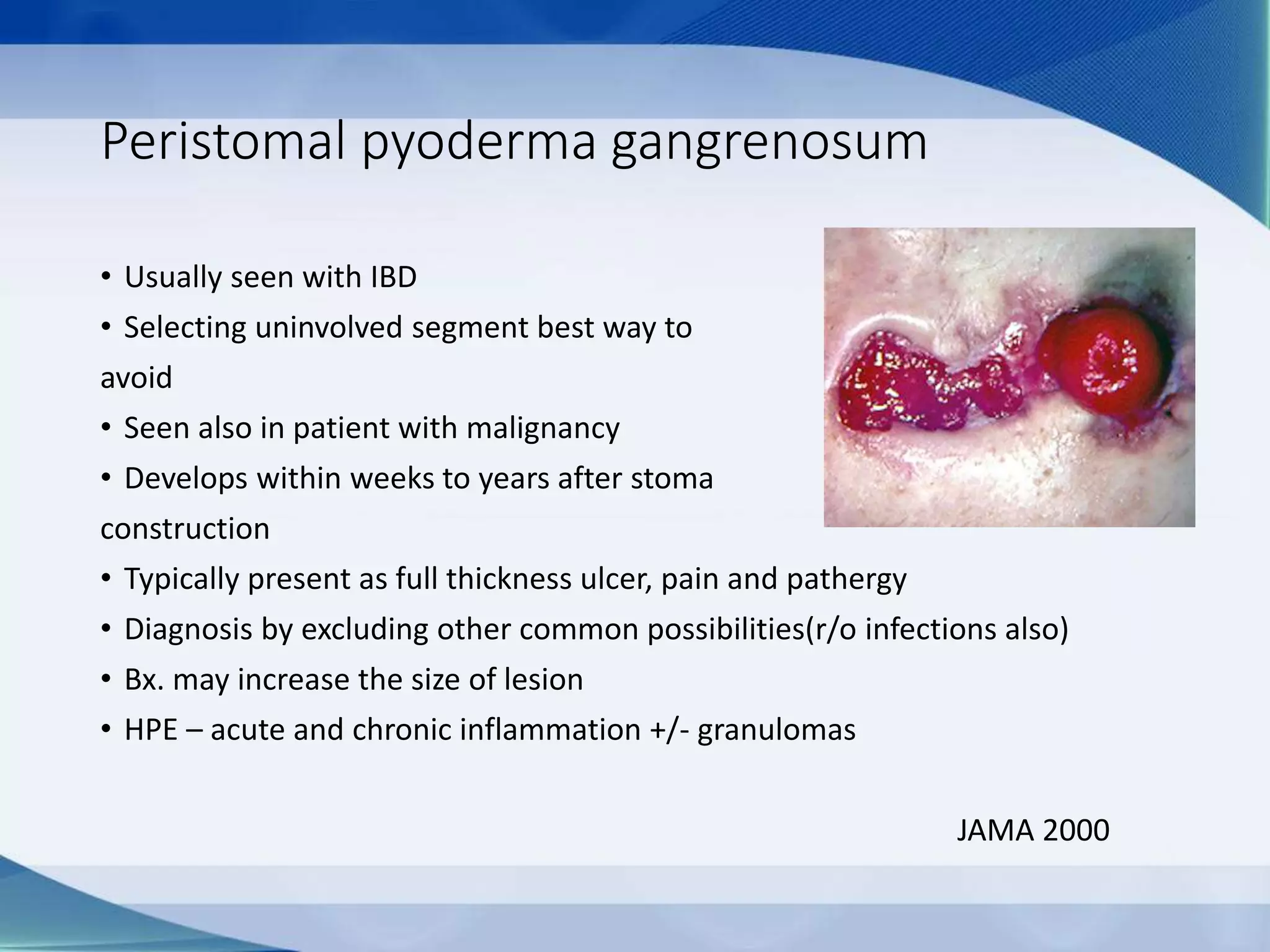
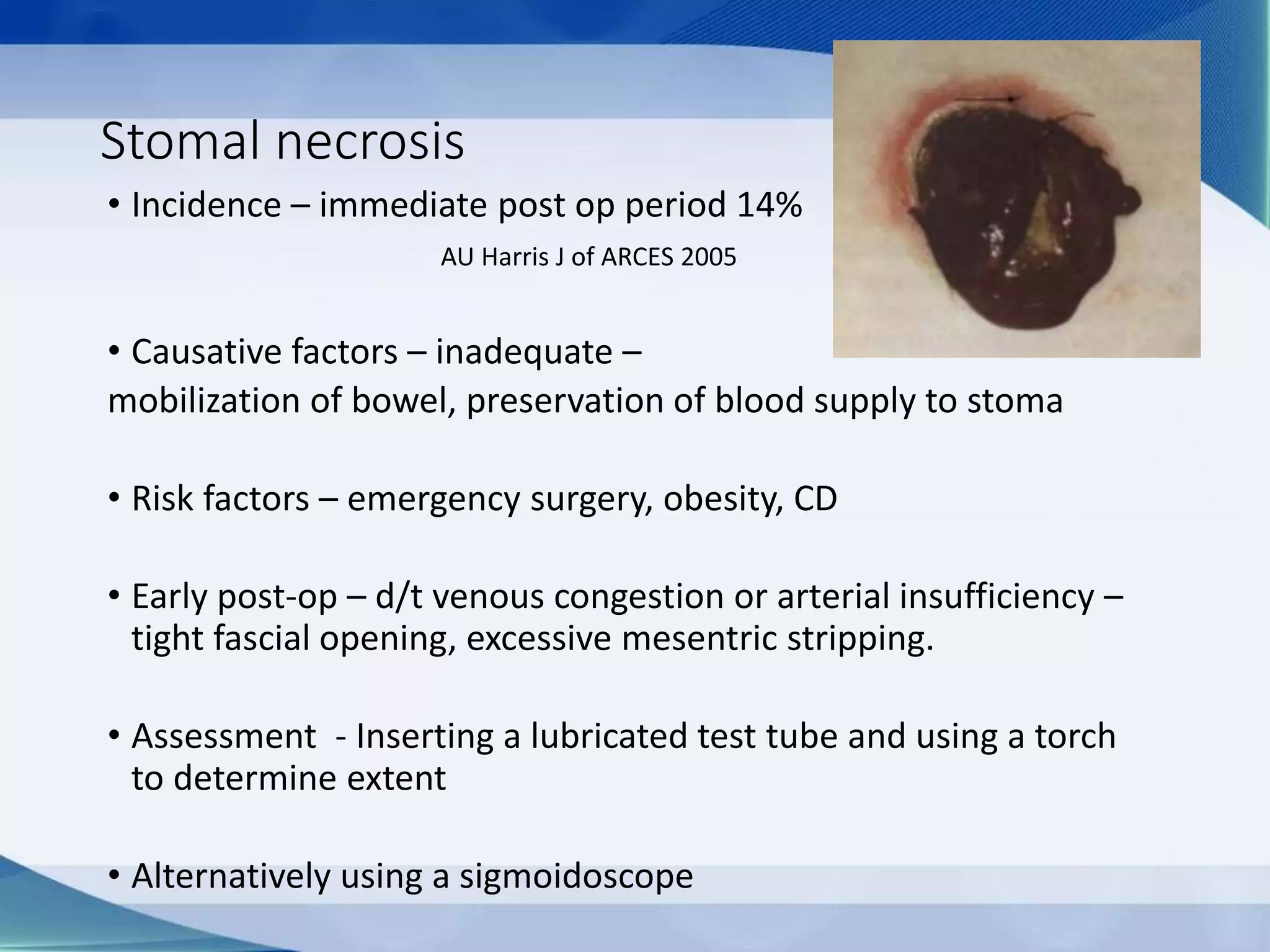
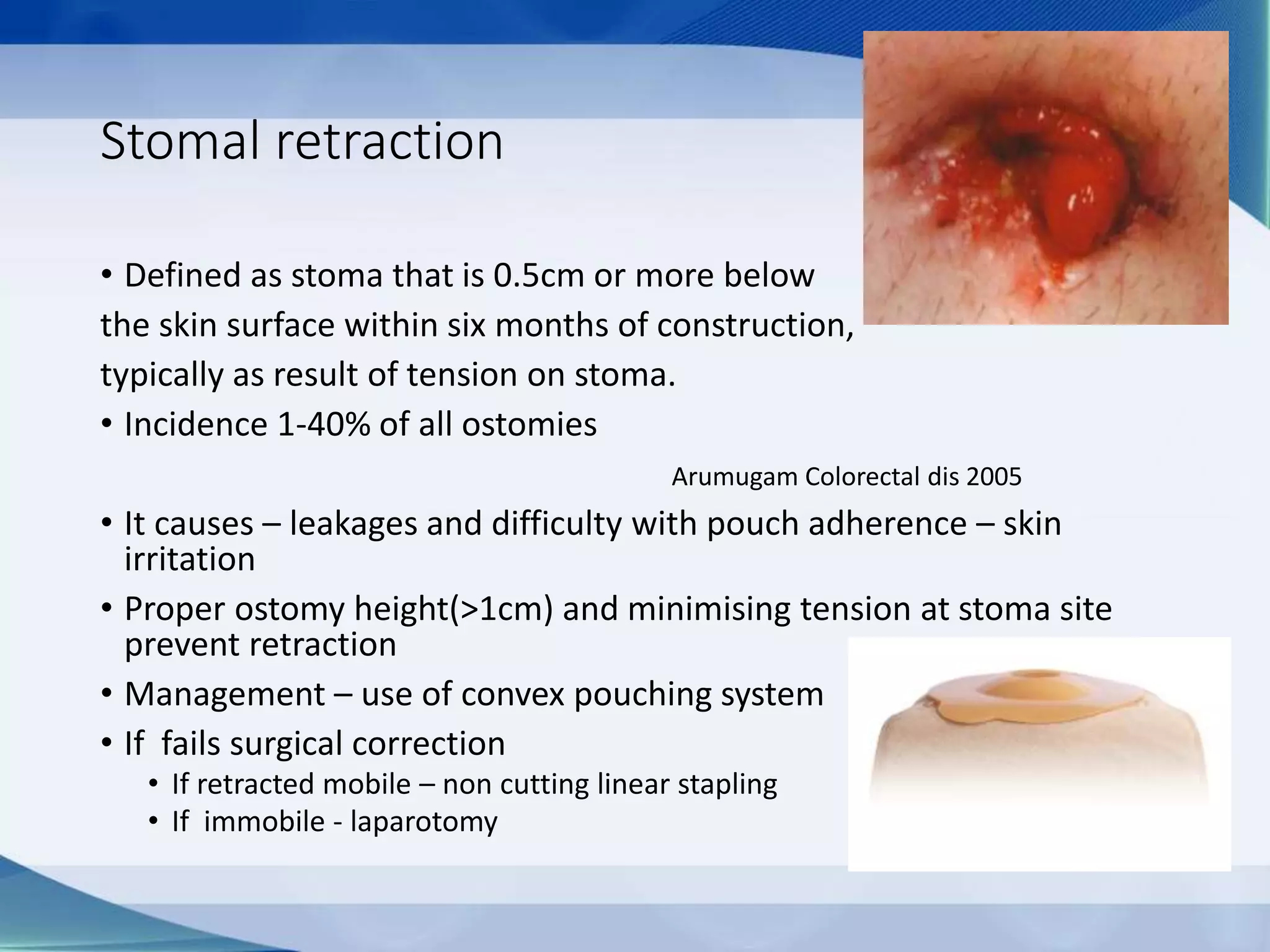
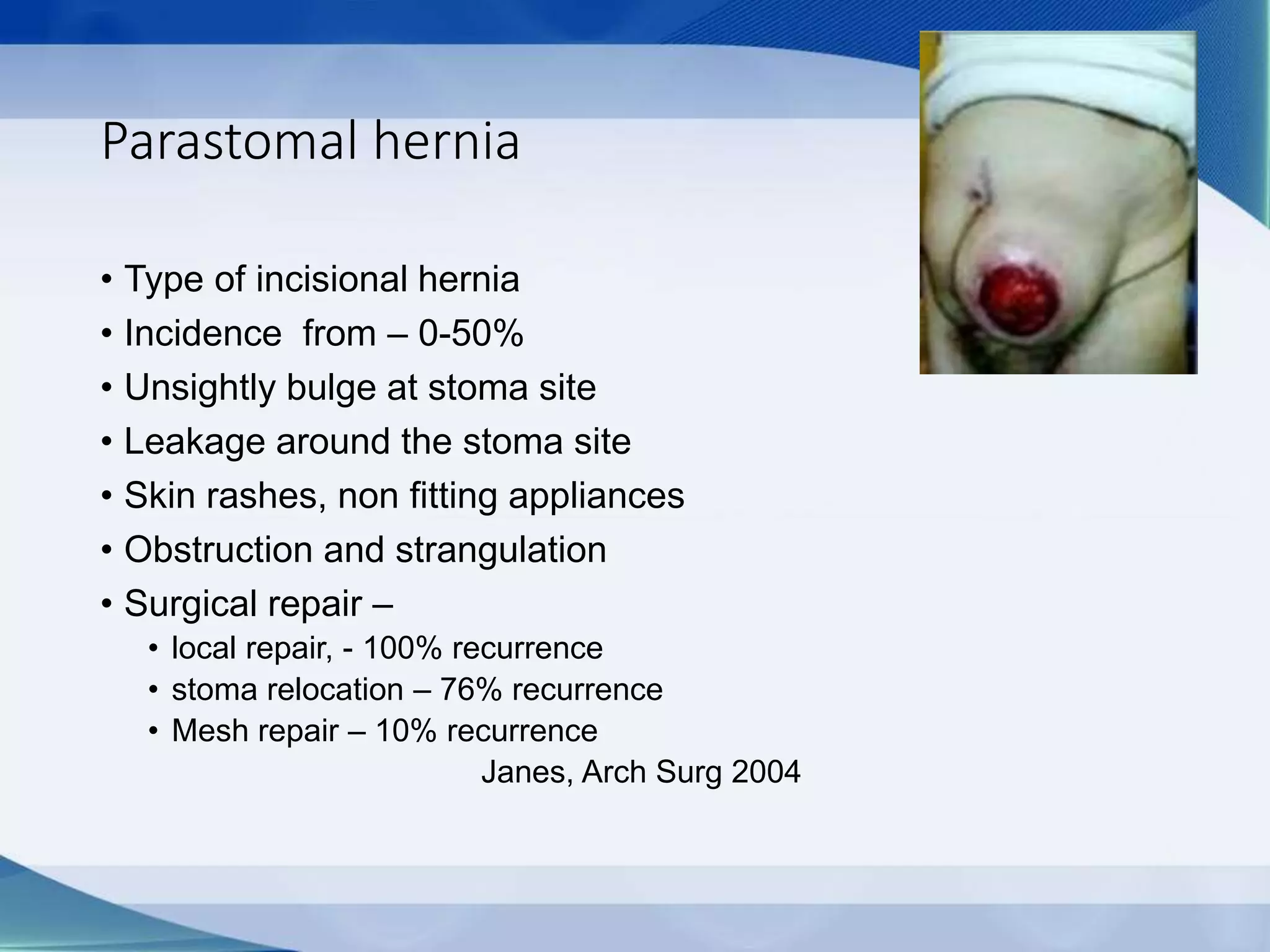
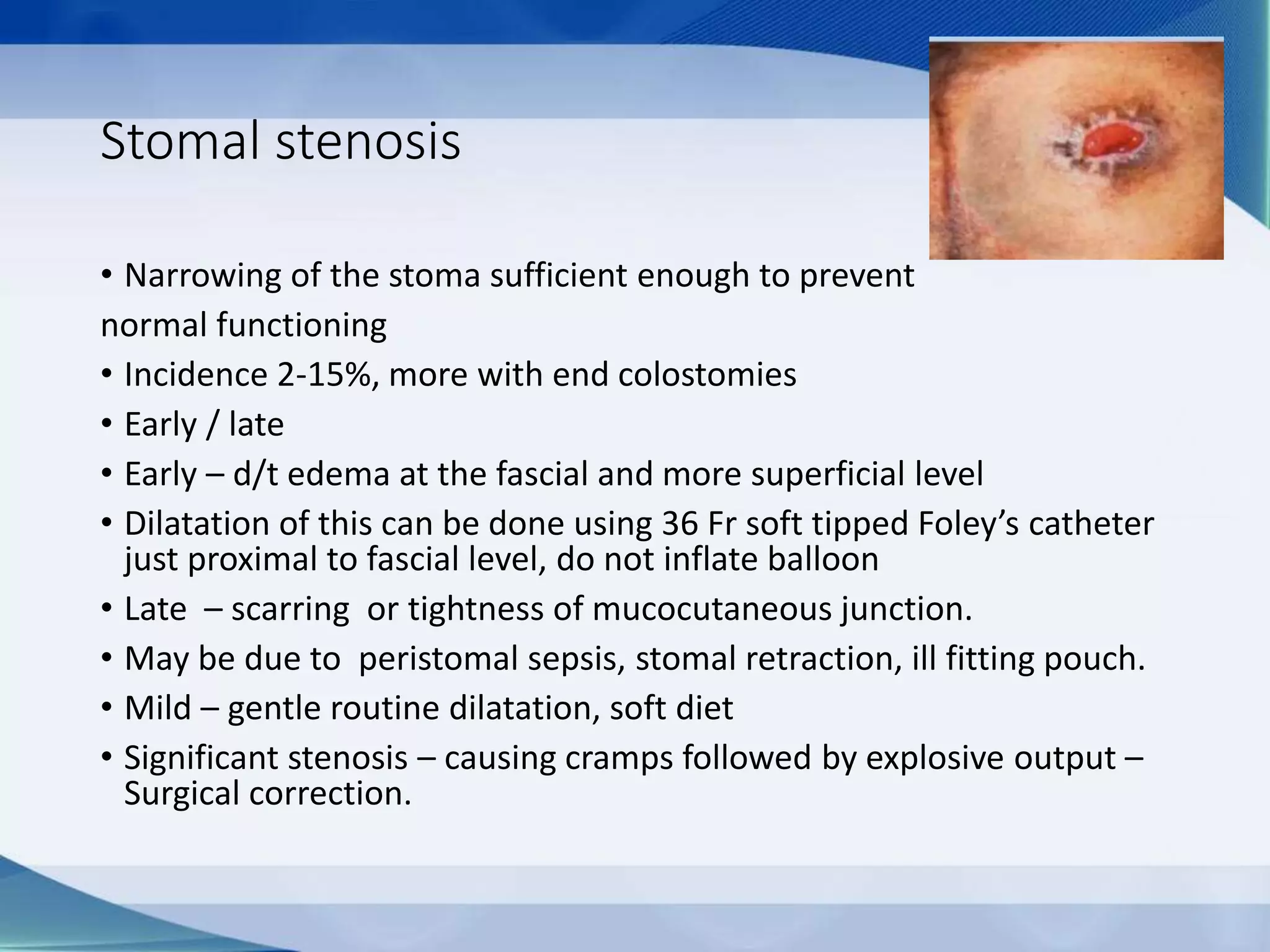
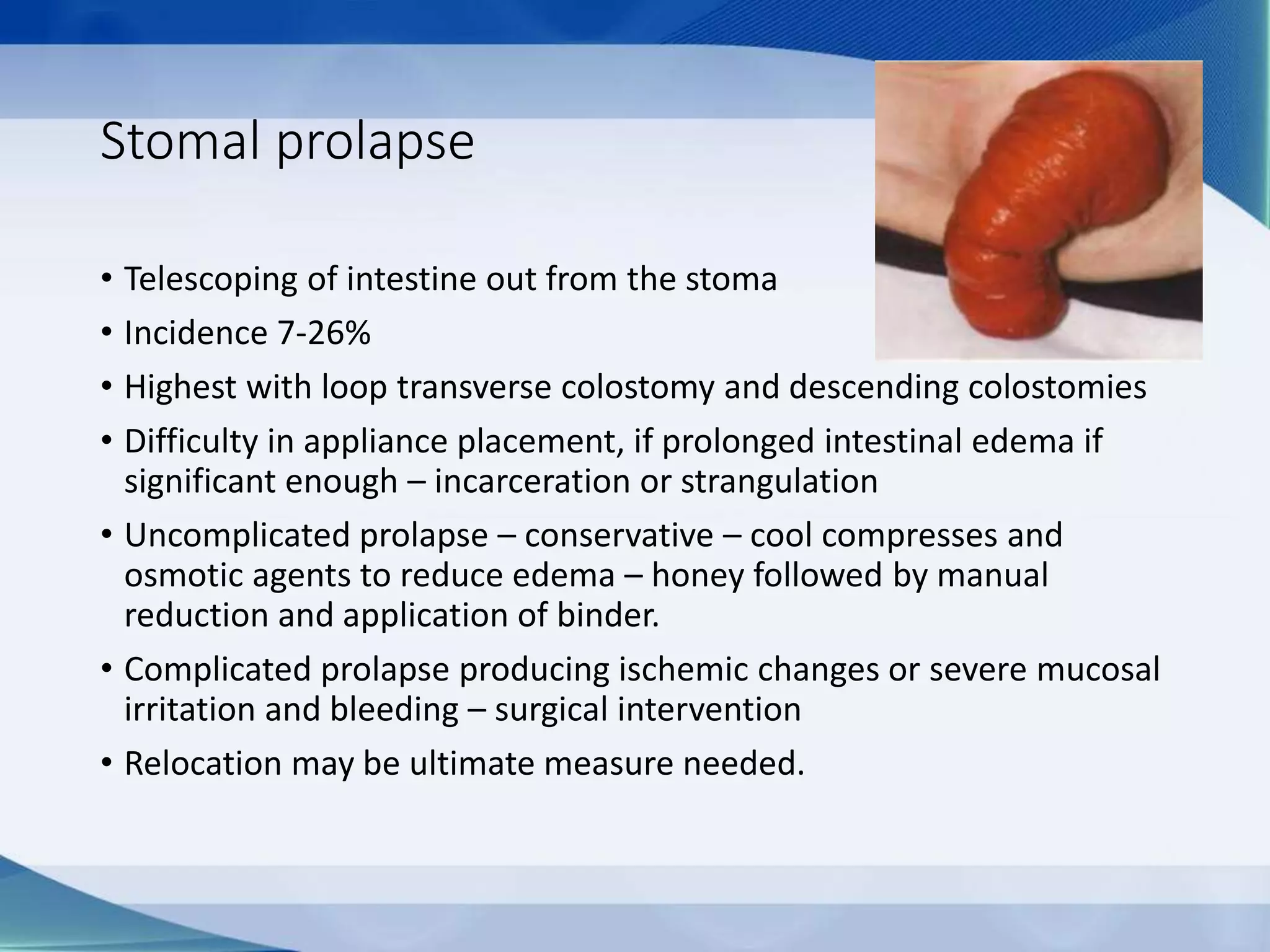
This document discusses intestinal stomas, including definitions, types, indications, and routine care. It covers colostomies and ileostomies, which are surgically created openings of the small or large intestine onto the abdominal wall. Complications are also summarized, such as dermatological issues, bleeding, necrosis, retraction, hernias, and prolapse. The document provides overview on prevention, risk factors, signs, and management of various stoma-related complications.