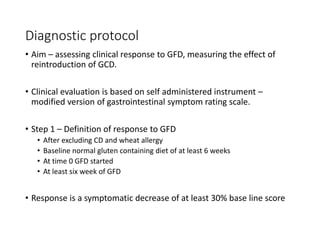
Gluten is a protein composite found in wheat, barley, and rye that gives elasticity to doughs. Non-celiac gluten sensitivity (NCGS) is a condition where symptoms are triggered by gluten ingestion in individuals who do not have celiac disease or wheat allergy. The exact prevalence of NCGS is unknown. Diagnosis involves exclusion of celiac disease and wheat allergy, followed by a gluten-free diet and gluten challenge. While the pathogenesis of NCGS differs from celiac disease, involving innate rather than adaptive immunity, further research is still needed to identify biomarkers and fully understand the condition.