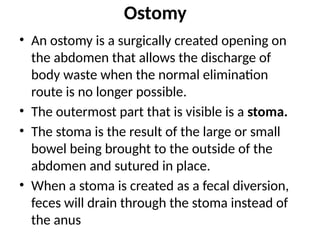
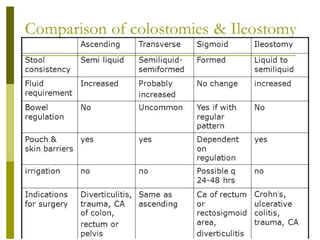
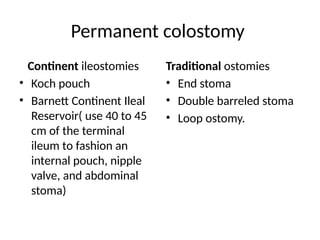
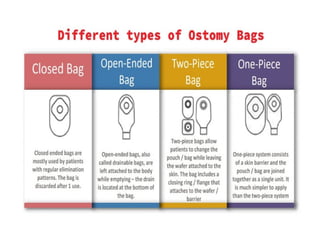
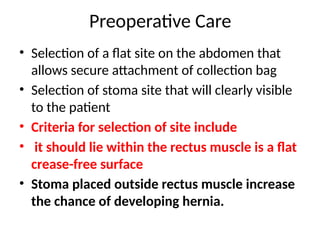
The document provides comprehensive information on colostomy and ileostomy care, explaining the surgical creation of a stoma for waste discharge when normal routes are unavailable. It details the types of ostomies, indications for their creation, preoperative and postoperative care, and guidelines for managing nutrition and wound care. The document emphasizes the importance of supporting patients' emotional well-being and body image adjustments following surgery.