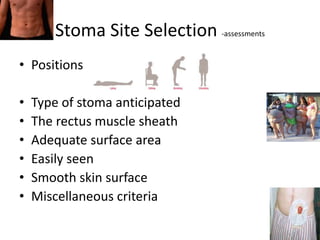
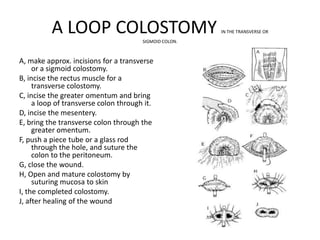
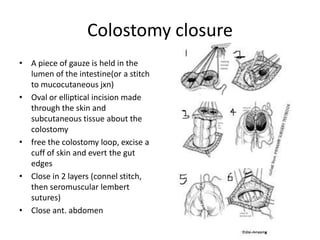
The document discusses colostomies, including their anatomy, indications for use, preoperative preparations, operative techniques, postoperative care, complications, and closure. A colostomy is a surgically created opening of the colon through the abdominal wall to divert fecal matter. It may be temporary or permanent depending on the underlying condition. Proper education and care are important for managing colostomies and improving patients' quality of life. Complications can include bleeding, prolapse, hernias, and skin irritation.