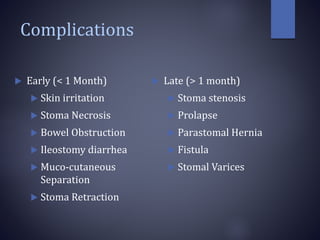
This document discusses complications that can occur with stomas. It defines stomas and provides the incidence of early and late complications. Early complications include skin irritation, stoma necrosis, bowel obstruction, ileostomy diarrhea, and mucocutaneous separation. Late complications include stoma stenosis, prolapse, parastomal hernia, and fistula. For each complication, the document discusses causes, clinical features, and management approaches. It provides details on evaluating and treating various early and late stoma complications.