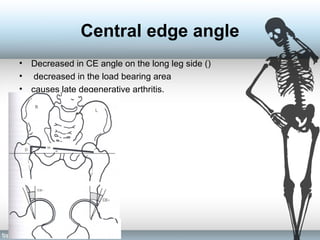
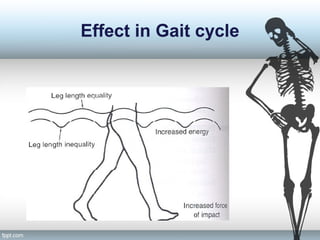
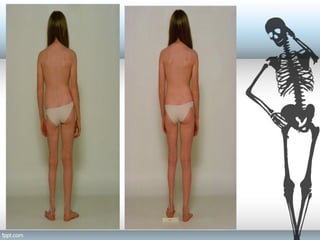
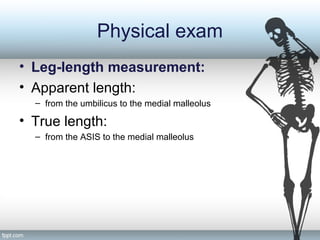
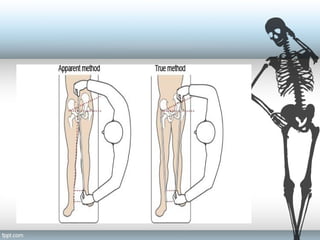
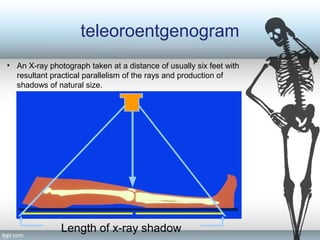
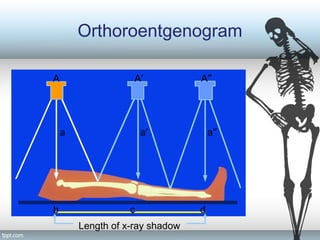
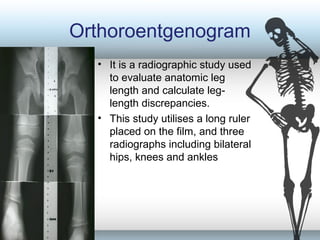
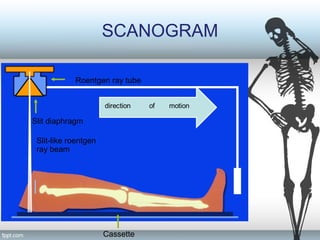
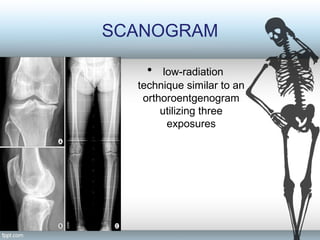
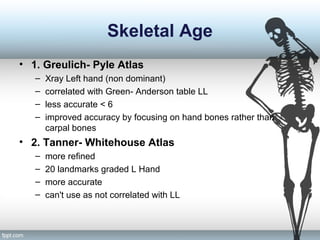
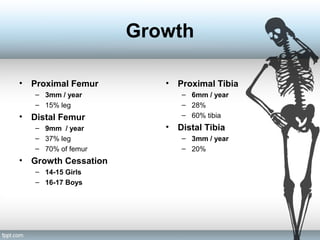
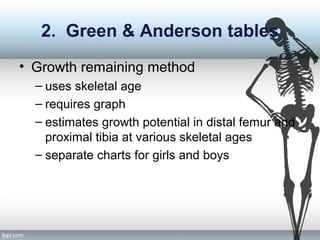
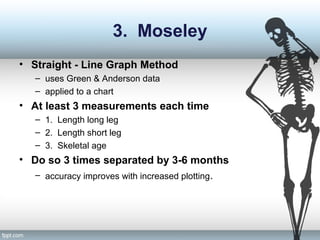
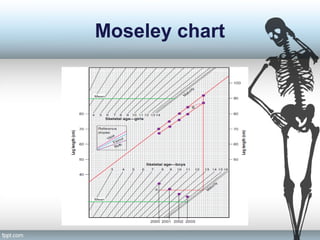
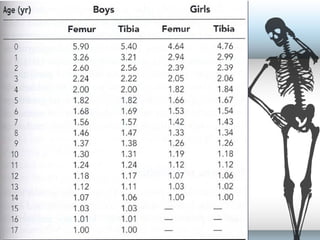
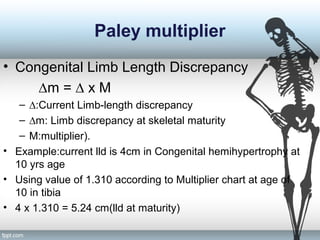
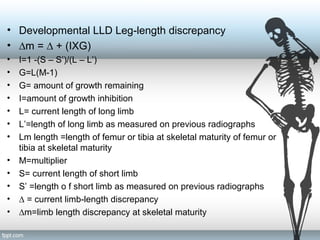
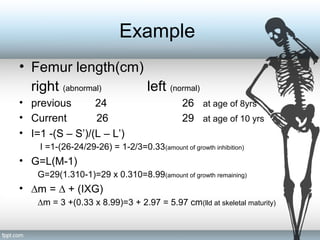
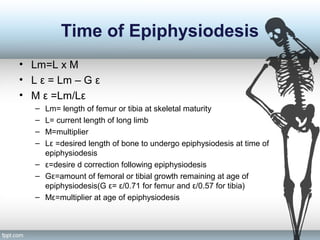
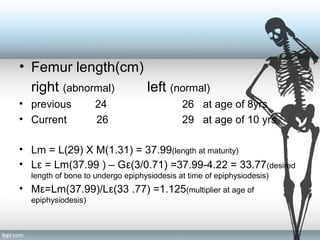
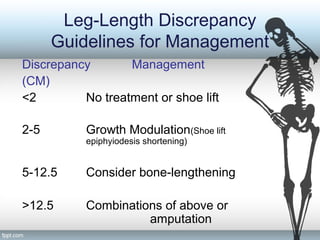
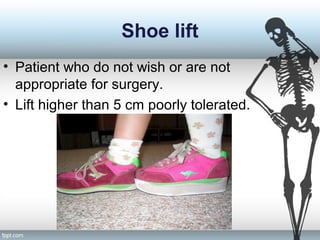
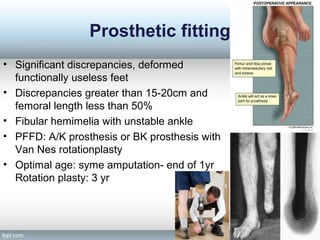
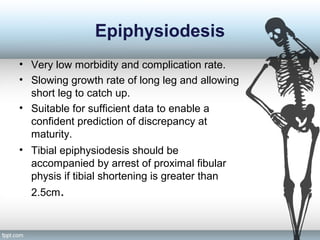
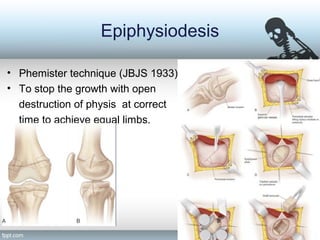
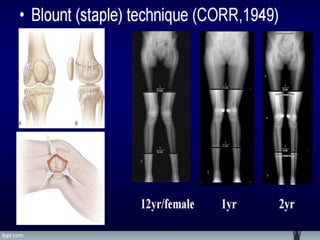
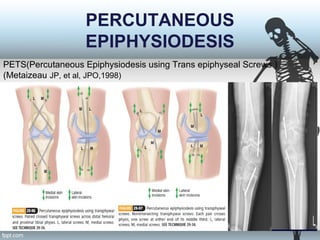
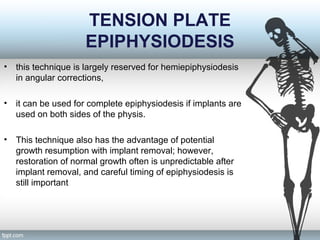
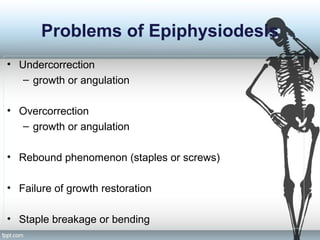
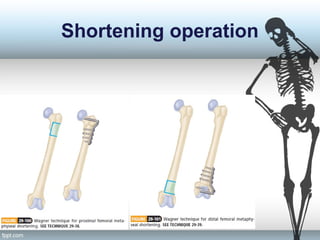
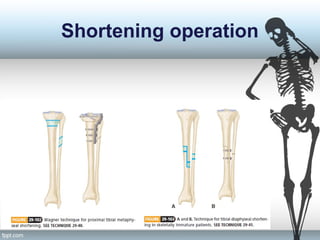
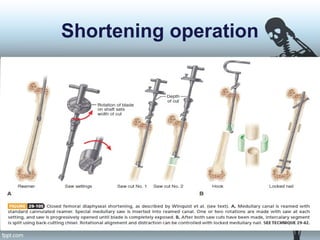
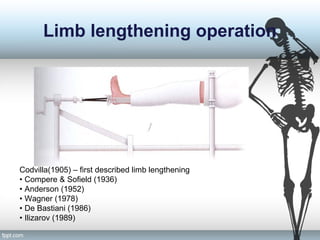
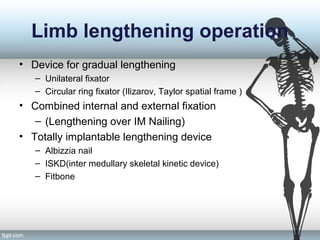
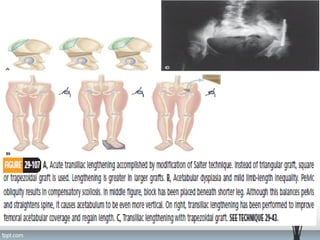
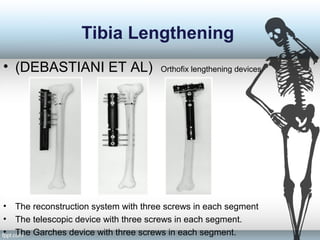
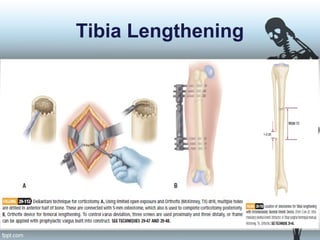
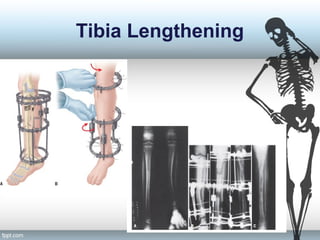
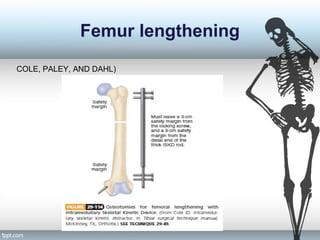
This document discusses limb length discrepancy (LLD), including its definition, causes, effects, evaluation, and management. LLD is when one lower limb is noticeably longer than the other. It is classified as structural or functional. LLD of 2.5 cm or more can cause back/hip/knee pain and gait abnormalities. Evaluation involves history, exam including block testing, and imaging like scansograms. LLD can be managed non-surgically with shoe lifts for small discrepancies or surgically with epiphysiodesis or bone lengthening depending on the severity.