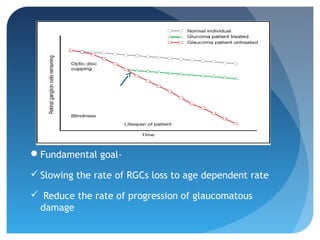
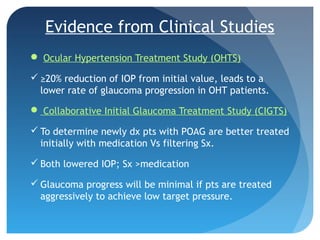
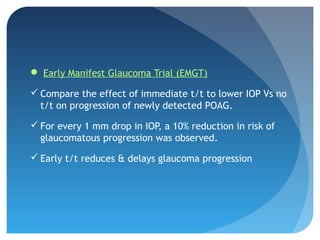
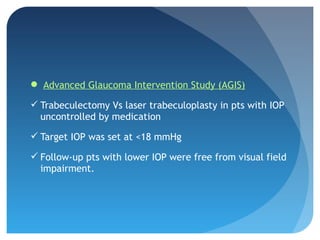
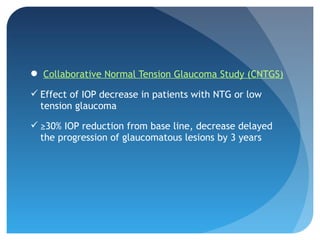
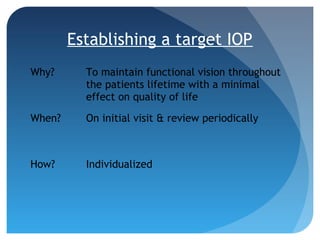
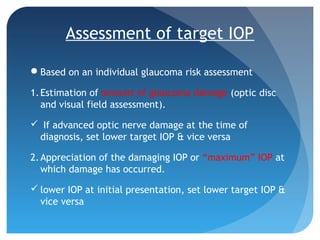
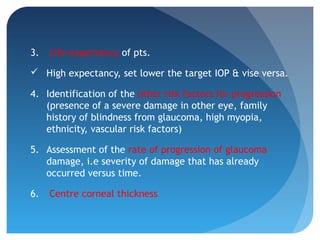
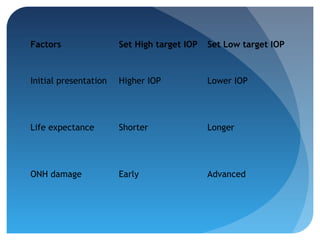
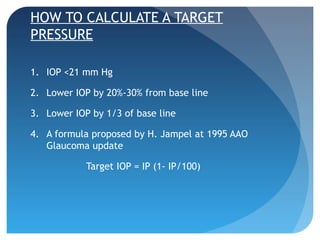
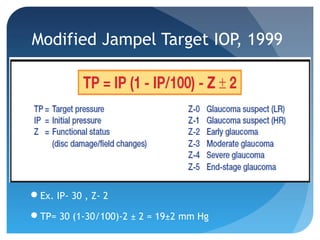
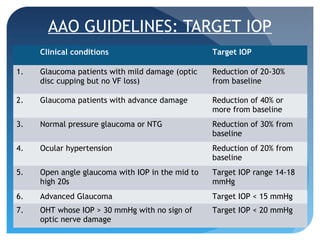
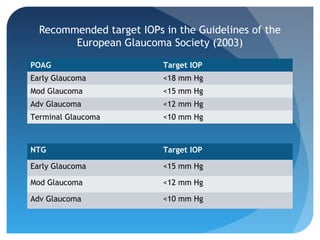
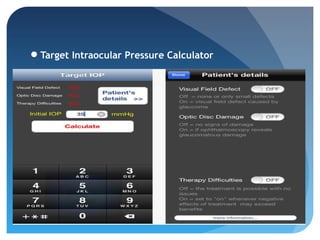
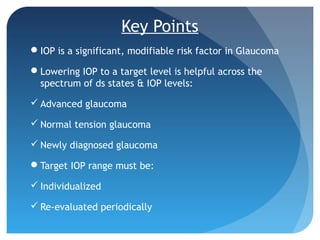
This document discusses target intraocular pressure (IOP) for treating glaucoma. It defines target IOP as the upper limit of IOP that prevents further glaucoma damage. Establishing an individualized target IOP is important to slow retinal ganglion cell loss and glaucoma progression over a patient's lifetime with minimal effects on quality of life. The target IOP should be based on factors like the amount of existing eye damage, maximum past IOP levels, life expectancy, and risk factors. The target is dynamic and must be reevaluated periodically, lowering it if damage progresses or raising it if side effects occur from low IOP. Clinical studies show that greater IOP reductions correlate with less glaucoma progression