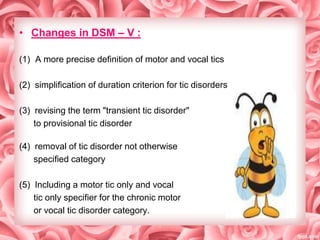
This document provides an overview of tic disorders, including Tourette's syndrome and chronic motor or vocal tic disorder. It defines tics and describes the DSM-IV criteria for different tic disorders. Potential etiologies include genetic and neurochemical factors. Treatment involves pharmacotherapy with antipsychotics or clonidine, as well as behavioral therapy such as habit reversal training. Prognosis is generally good, though comorbid conditions can worsen outcomes. The DSM-V made changes including reclassifying tic disorders as motor disorders and revising diagnostic criteria.
![Motor and vocal tics are divided into:
1]Simple motor tics:
2] Simple vocal tics
3] Complex motor tics
4] Complex vocal tics](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-3-320.jpg)
![DSM-IV-TR TIC DISORDERS:
1] Gilles de la Tourette syndrome
2] chronic motor or vocal tic disorder,
3] transient tic disorder, &
4] tic disorder not otherwise specified](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-4-320.jpg)
![DSM-IV-TR Diagnostic Criteria for
Tourette's Disorder:
1] Multiple motor and one or more vocal tics have been present at
some time during the illness, although not necessarily concurrently.
2] The tics occur many times a day, nearly every day or intermittently
throughout a period of more than 1 year, and during this period there
was never a tic-free period of more than 3 consecutive months
(2 months in ICD-10)
3] The onset is before age 18 years.
4] The disturbance is not due to the direct physiological effects of a
substance (e.g., stimulants) or a general medical condition (e.g.,
Huntington's disease or postviral encephalitis).](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-5-320.jpg)

![ETIOLOGY
1] Genetic Factors
2] Neurochemical and Neuroanatomical Factors
3] Immunological Factors](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-7-320.jpg)
![A] GENETIC FACTORS:
1)Twin studies.
2)Bilinear mode of familial transmission:
3)Rare sequence variant in SLITRK1 on chr.13q31
4)50% tourette’s patients have ADHD
5)40% tourette’s patients have OCD
6)First degree relatives at risk of tics and OCD](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-8-320.jpg)
![B] NEUROCHEMICAL & NEUROANATOMICAL
FACTORS
1] Dopamine system:
--Anti Dopaminergic agents
[Haloperidol, Pimozide, Fluphenazine] -----tic suppressors.
--Central Dopaminergic activators
[methylphenidate, amphetamines, cocaine]--------tic exacerbators.
--However no concrete evidence
2] choline and n-acetylaspartate:
--Reduction of the above in left putamen and
frontal cortex.
--This leads to reduced density of neurons](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-9-320.jpg)
![3] Endogenous opioids:
pharmacological agents that antagonize endogenous opiates for eg
naltrexone reduce tics.
4] Noradrenergic system:
Clonidine decreases NA and causes reduced Dopamineregic
activity & hence reduces tics.
5] Structural abnormalities
Basal Ganglia lesions are known in movement disorders
C] IMMUNOLOGICAL FACTORS
autoimmune process that is secondary to streptococcal infections is
a potential mechanism for Tourette's disorder.](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-10-320.jpg)
![CLINICAL FEATURES:
• Initial tics are in the face and neck and then they progress
downwards
• The most commonly described tics are those affecting the face &
head, arms & hands, lower extremities, RS & GIT.
• The most frequent initial symptom is an eye-blink tic, followed by
a head tic or a facial grimace.
• The complex tics appear many years later[ coprolalia-1/3rd]](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-11-320.jpg)

![ASSESSMENT INSTRUMENTS
•
•
Tic Symptom Self Report
Yale global tic severity scale: [ YGTSS ]
Number
(0-5)
Frequency
(0-5)
Intensity
(0-5)
Complexity
(0-5)
Interference Total
(0-5)
(0-25)
Motor Tic
Severity
Vocal tic
severity
Total Tic Severity Score = Motor Tic Severity + Vocal Tic Severity (0-50)
Impairment:
None : 0
Moderate:30
Minimal : 10
Marked : 40
Total Yale Global Tic Severity Scale Score
( Total Tic Severity Score + Impairment ) ( 0-100 )
Mild: 20
Severe: 50](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-13-320.jpg)
![COURSE AND PROGNOSIS:
1] Most often there is reduction in severity and frequency with age.
2] Co-morbid MDD, OCD and ADHD worsen the prognosis and cause
exacerbation.
3] Imaging has revealed presence of smaller
caudate nucleus in patients and has
predictive value in prognosis.
4] Mild forms need not require treatment
if they are socially functional.](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-14-320.jpg)
![DIFFERENTIAL DIAGNOSIS
SYNDROME
DIFFERENTIATING
FEATURE
COURSE
MOVEMENT
HALLERVORDENSPATZ
A/W optic atrophy
dementia,ataxia,lability,
dysarthria
Progresses to death in
15-20 years
Choreic,athetoid,
myoclonic
SYDENHAM’S
CHOREA
F>M, A/W RF
Self limited
Choreiform
HUNTINGTON’S
DISEASE
Late onset[30-50],
dementia, atrophy
Progressive to death
Choreiform
WILSON’S DISEASE
10-25years,KF rings,
liver fn
Chelating agents
Wing beating tremor,
Dystonia
HYPERREFLEXIA
[LATAH,MYRIACHIT]
CHILDHOOD
Non-progressive
Startle
response,echolalia
MYOCLONUS
Any age, no
vocalisations
Variable
Myoclonus
TARDIVE
TOURETTE’S
DISORDER
SYNDROME
After APD
Variable depending on
dosage
Orofacial dyskinesia,
choreoathetosis,tics,
vocalisations](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-15-320.jpg)
![TREATMENT:
1] Not to misinterprest tic as behavioral problem
2] Family psychoeducation
3] Mild cases : no treatment required
4] Severe cases : pharmacotherapy
& behavioral therapy](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-16-320.jpg)
![PHARMACOTHERAPY
1] Haloperidol and Pimozide most widely researched and used.
Haloperidolinitial daily dose for adolescents is 0.25 and 0.5 mg.
not approved in children < 3 years age.
Pimozide- 1mg-2mg----increase alt. days upto 10-20 mg
2] Risperidone and Olanzapine have
also showed beneficial results.](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-17-320.jpg)
![3]Clonidine and guanfacine :
Although presently not approved by US FDA, several studies
reported that clonidine and guanafacine were efficacious in
reducing tics.
4] For associated OCD, SSRI’s used alone or with APD’s.
5] For co-existing ADHD the decision depends on severity and if
reqired Atomoxetine or methylphenidate might have to be started.](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-18-320.jpg)
![BEHAVIORAL THERAPY:
• Habit reversal technique, stopping premonitory urge, relaxation
therapy ( it may reduce the stress that often exacerbates Tourette's
disorder) [as reviewed by Stanley hobbs]
• Premonitary urge :
Older children, adolescents, and adults often report tics to be
preceded by an unpleasant sensation
denoted as a ―premonitory urge‖.
• Premonitory Urge for Tics Scale (PUTS) :
This is a 10 item scale, & 9 items pertaining
to intensity of premonitory urge is graded
on a scale of 1 to 4. Total maximum score
is 36, while minimum score is 9.](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-19-320.jpg)

![• Prevalence is 100-1000 times more than Tourette’s
• Similar hereditary factors as Tourette’s.
• Motor tics >> vocal tics [not as loud … mainly grunting due to
diaphragm, thoracic or abdominal muscles]
• Prognosis- onset between 6-8years,
facial tics—good prognosis
• Management- psychotherapy &
behavior therapy](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-21-320.jpg)


![REFERENCES
1] Kaplan & Sadock’s Comprehensive
Textbook Of Psychiatry
2] Kaplan & Sadock’s Synopsis Of
Psychiatry
3] Tourette’s disorder and other tic
disorders in DSM-5: a comment
Eur Child Adolesc Psychiatry. 2013
February; 20(2): 71–74](https://image.slidesharecdn.com/18ticdisorderfinal-140113135713-phpapp02/85/tic-disorder-27-320.jpg)
