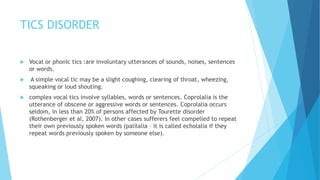
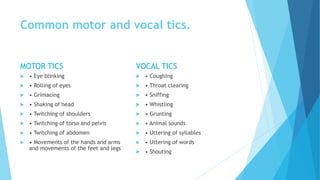
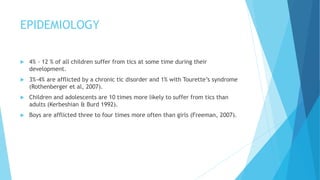
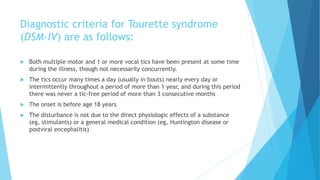
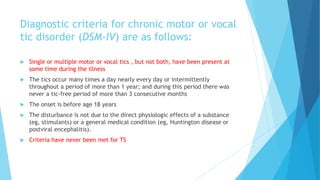
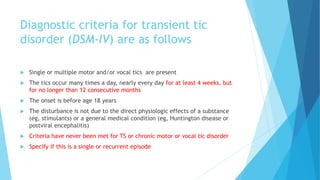
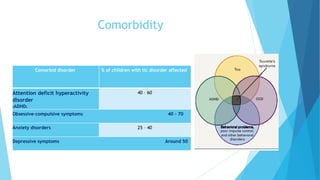
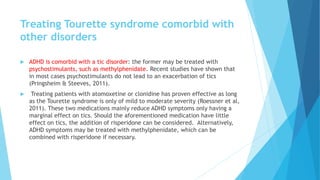
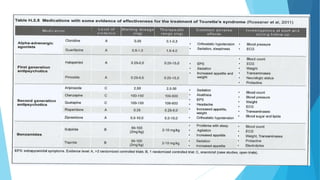
This document provides an overview of tic disorders, including epidemiology, etiology, diagnosis, classification, comorbidity, and treatment. It notes that tic disorders are characterized by sudden, rapid motor or vocal tics and affect 4-12% of children at some point in development. The causes are thought to involve genetic and neurobiological factors interacting with psychological influences. Diagnosis involves medical history and examination to rule out other conditions. Treatment includes psychoeducation, medication management, and addressing any comorbid disorders like ADHD or OCD.