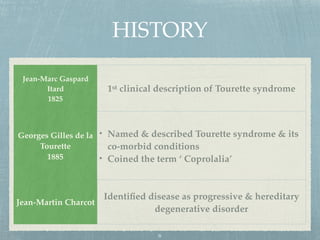
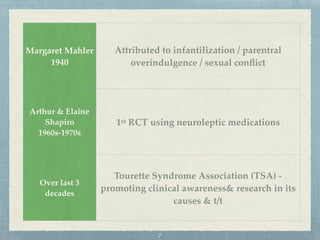
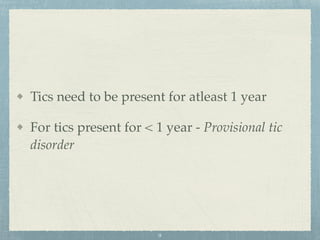
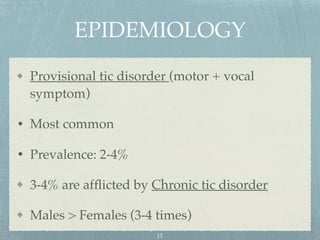
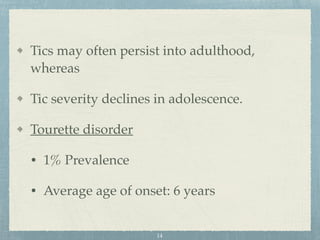
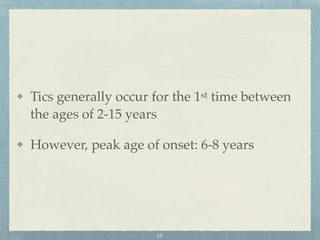
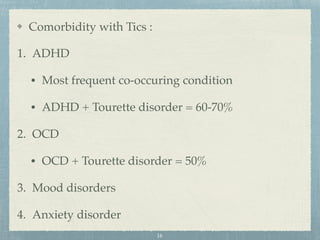
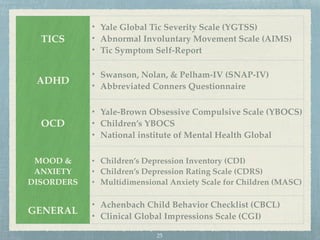
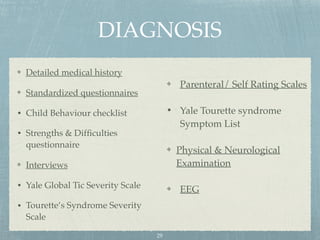
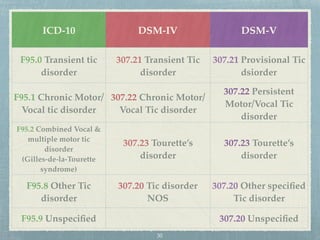
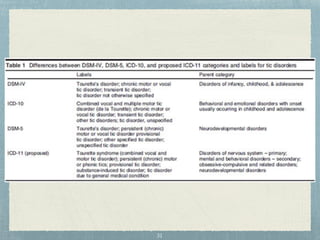
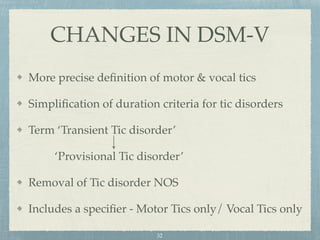
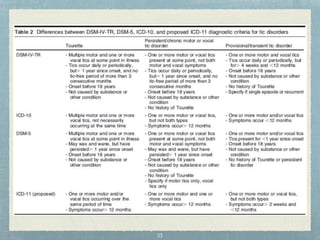
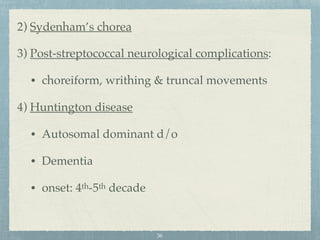
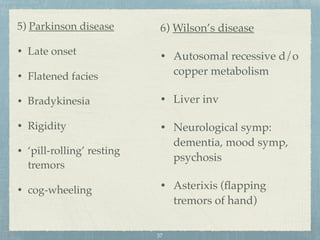
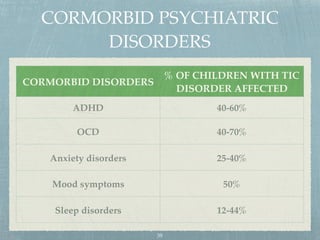
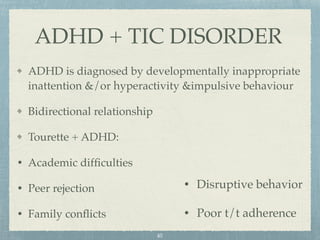
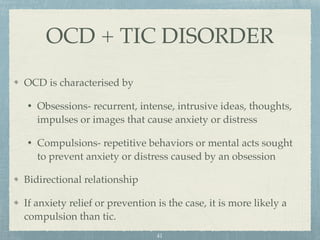
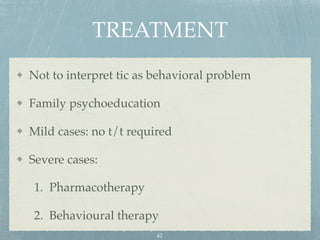
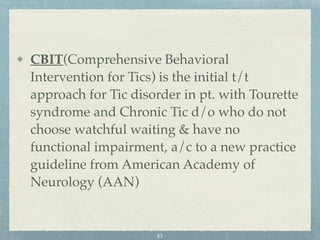
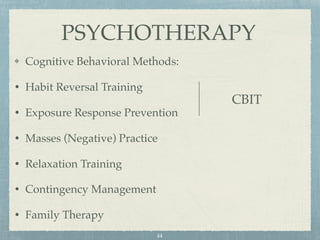
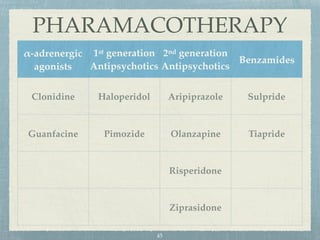
This document provides an overview of tic disorders, including Tourette syndrome. It discusses the history, classification, epidemiology, etiology, clinical features, diagnosis, differential diagnosis, comorbid psychiatric disorders, and treatment of tic disorders. Some key points include:
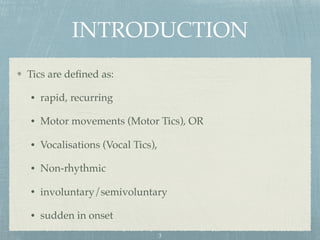
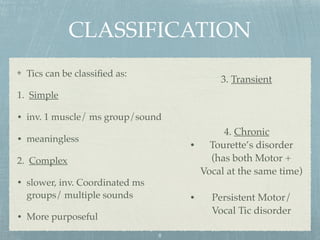
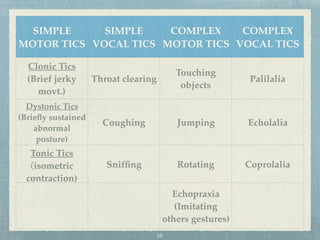
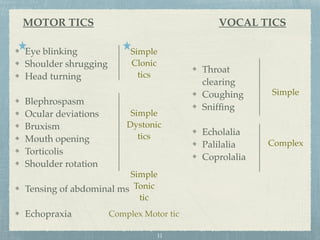
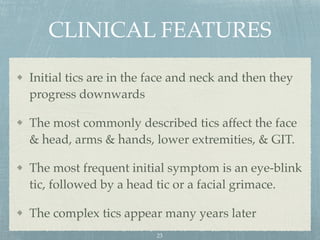
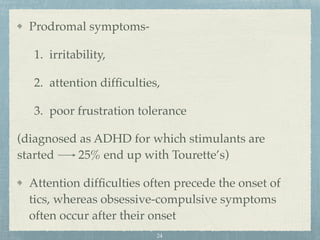
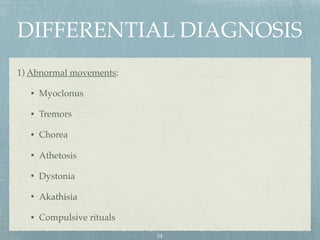
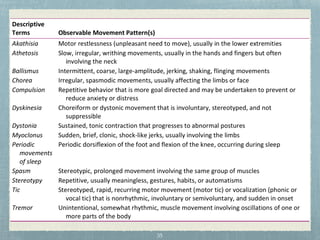
- Tic disorders are involuntary movements or vocalizations that can be either simple or complex. Tourette syndrome involves both motor and vocal tics.
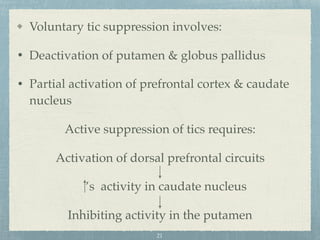
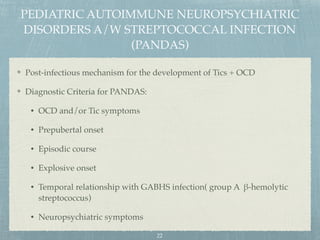
- Risk factors include genetic predisposition and environmental triggers like infections. Involvement of the cortico-striato-thalamic circuits in the brain is also implicated.
- Prevalence of tic disorders ranges from 2-4% for transient tics to 1% for Tourette syndrome. Males are affected more commonly