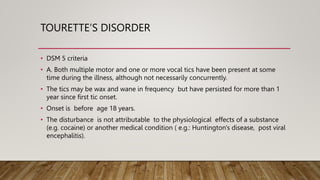
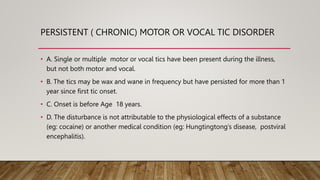
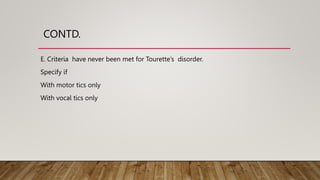
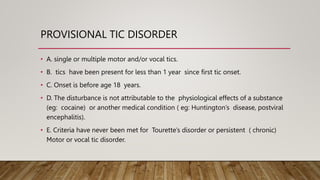
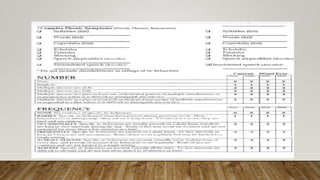
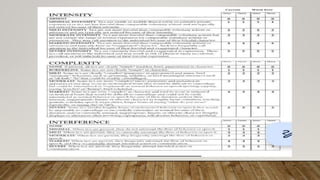
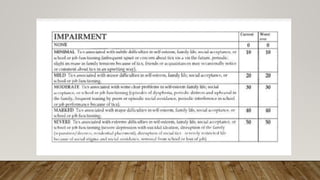
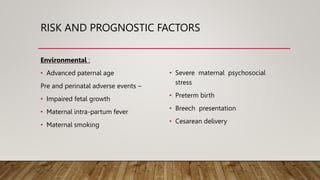
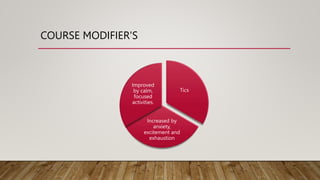
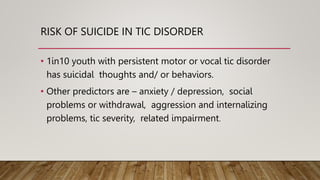
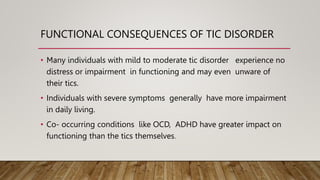
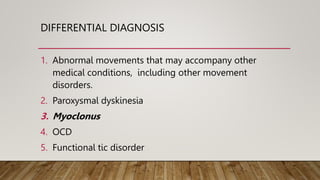
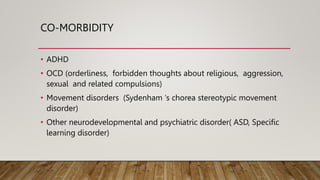
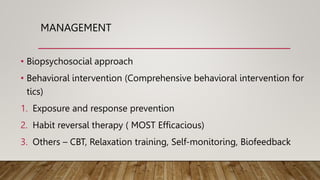
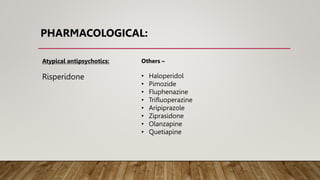
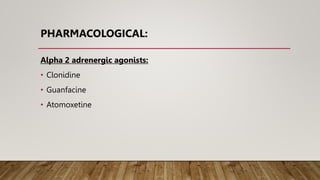
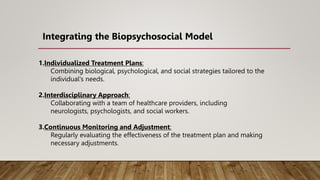
The document provides an overview of tic disorders, including types such as Tourette's disorder and persistent tic disorder, detailing their symptoms, prevalence, biological causes, risk factors, and associated conditions. It highlights the importance of individualized treatment plans combining behavioral and pharmacological interventions, along with an interdisciplinary approach among healthcare providers. The document also addresses the functional consequences of tic disorders, the risk of co-morbid conditions, and strategies for management and monitoring.