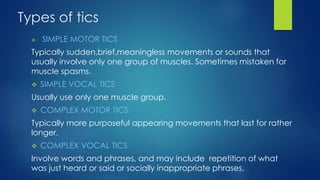
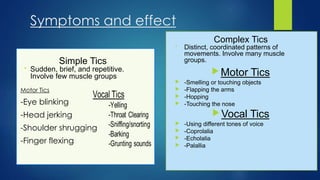
Tics are sudden, repetitive movements or sounds that involve discrete muscle groups. Tourette's syndrome is a neurological disorder characterized by both motor and vocal tics which begin in childhood and are often linked to conditions like ADD and OCD. While there is no cure, tics typically improve after adolescence. Treatment options include medications, behavioral therapies, and supportive counseling to help manage symptoms and their social impact.