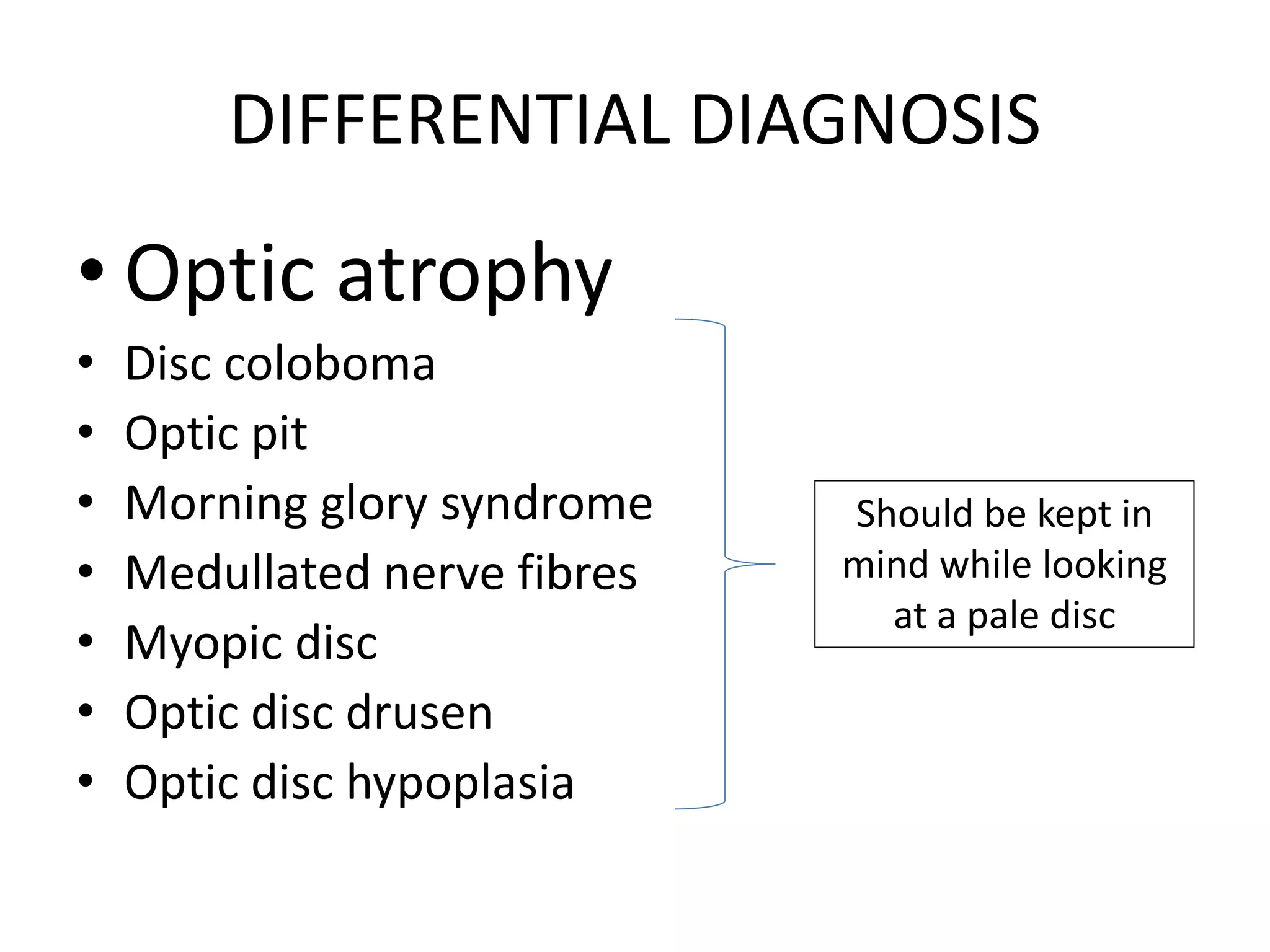
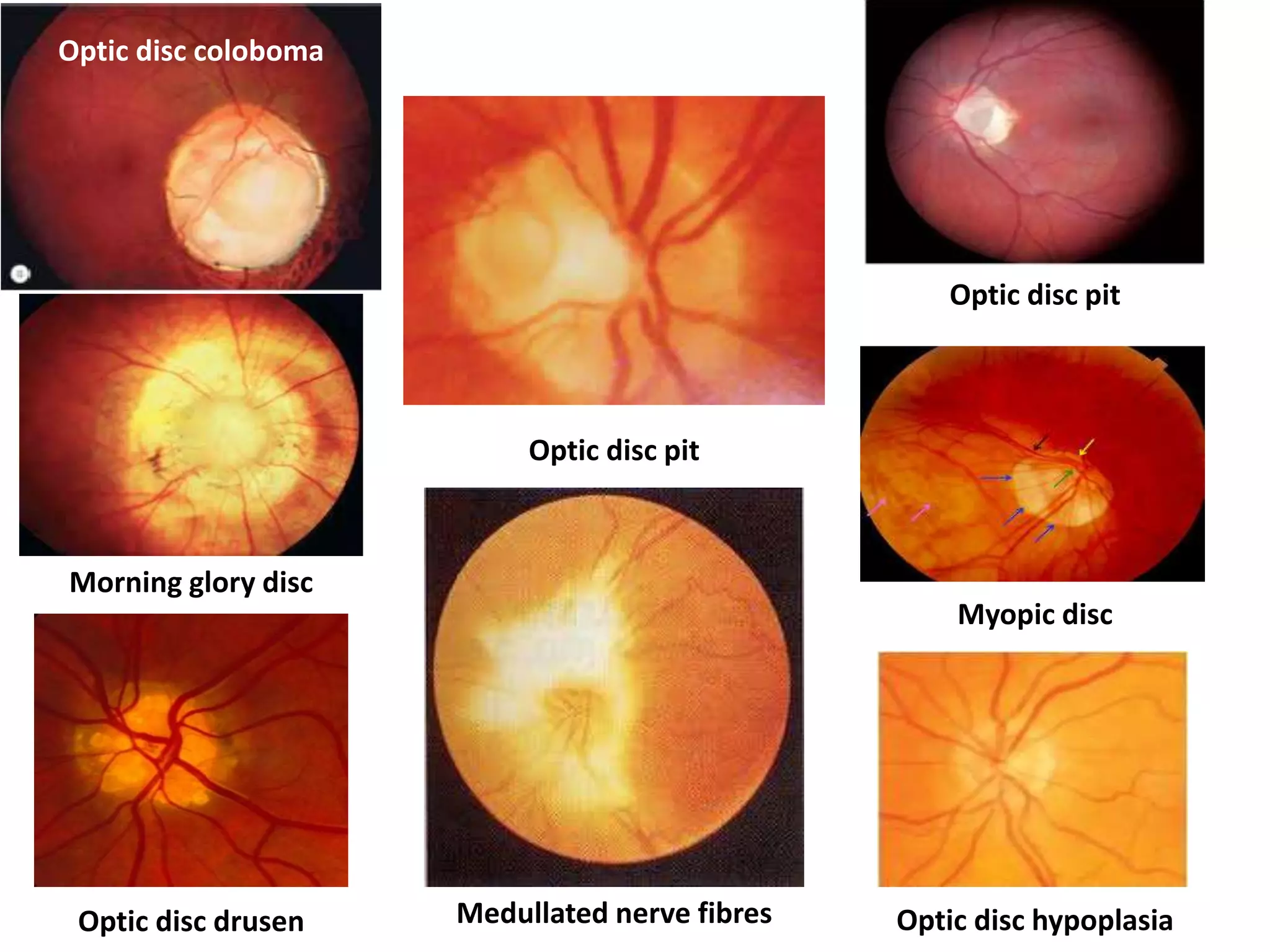
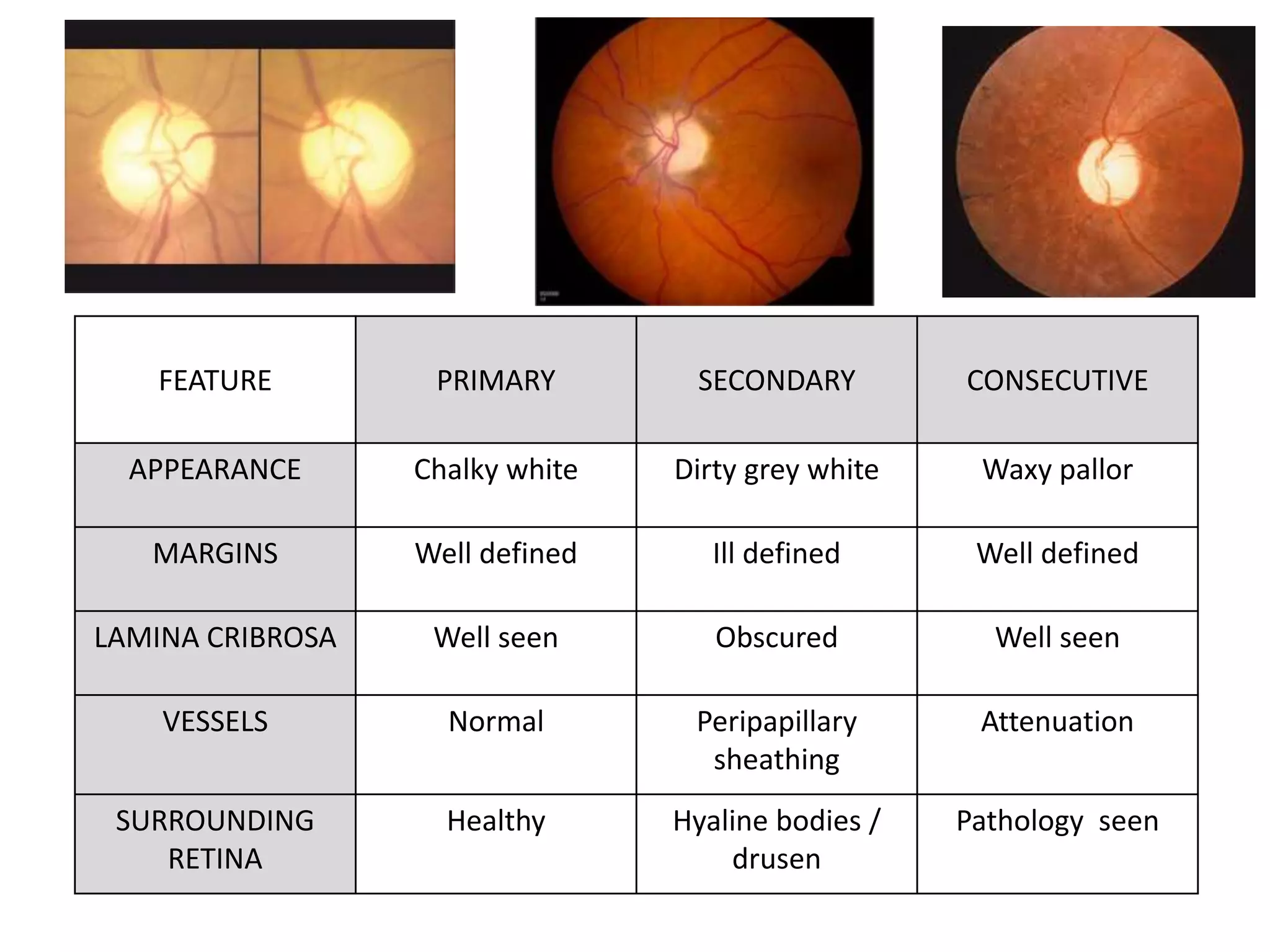
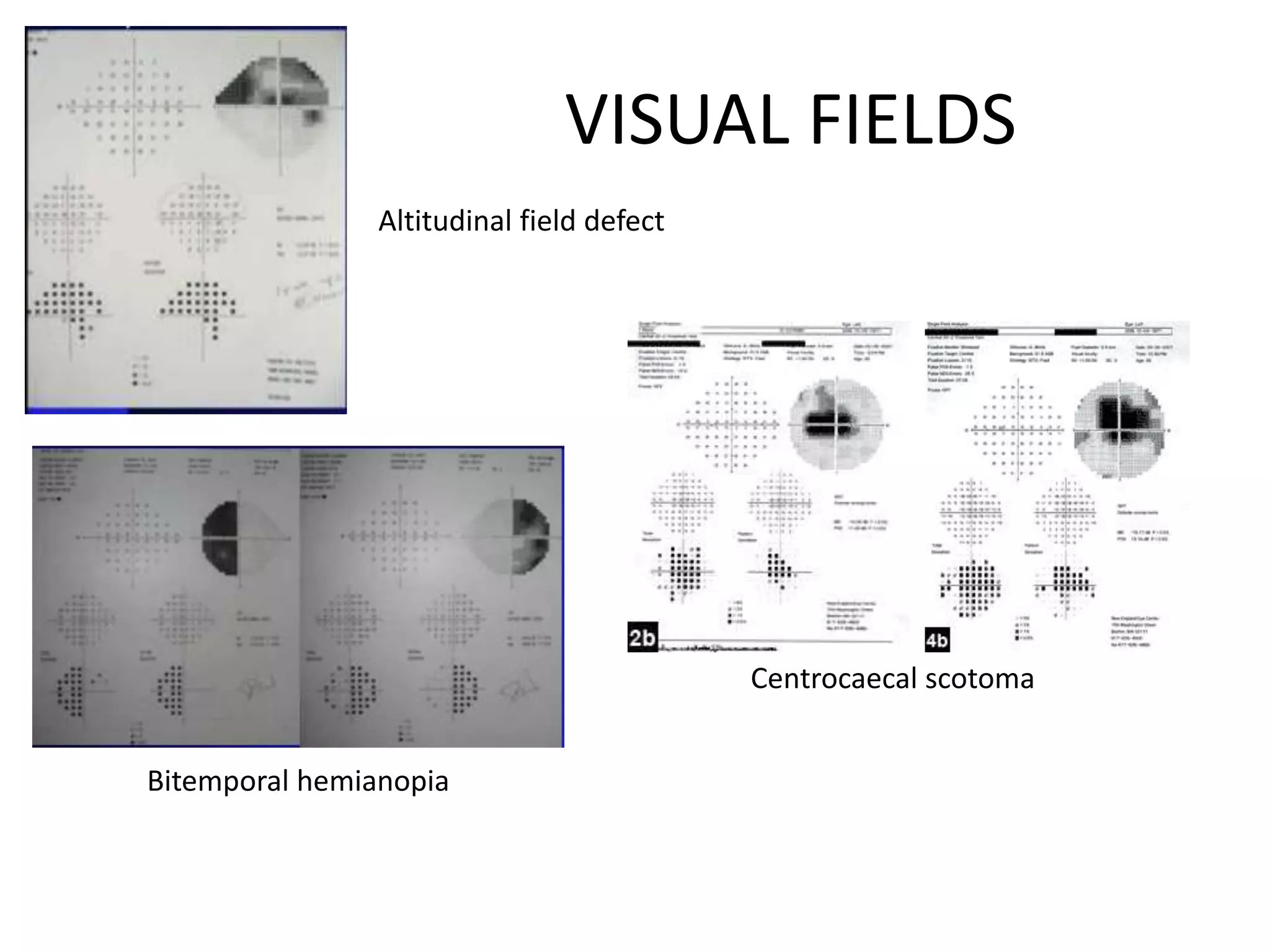
The document provides a comprehensive overview of pale optic disc assessment, covering its etiology, differential diagnosis, and management strategies. It emphasizes the importance of clinical evaluation to determine the underlying cause of disc pallor and assess visual prognosis. Example cases and specific examination details highlight various pathologies associated with optic disc appearance and recommendations for investigations and interventions.