This document provides an overview of the anatomy and clinical assessment of the optic nerve in 3 paragraphs:
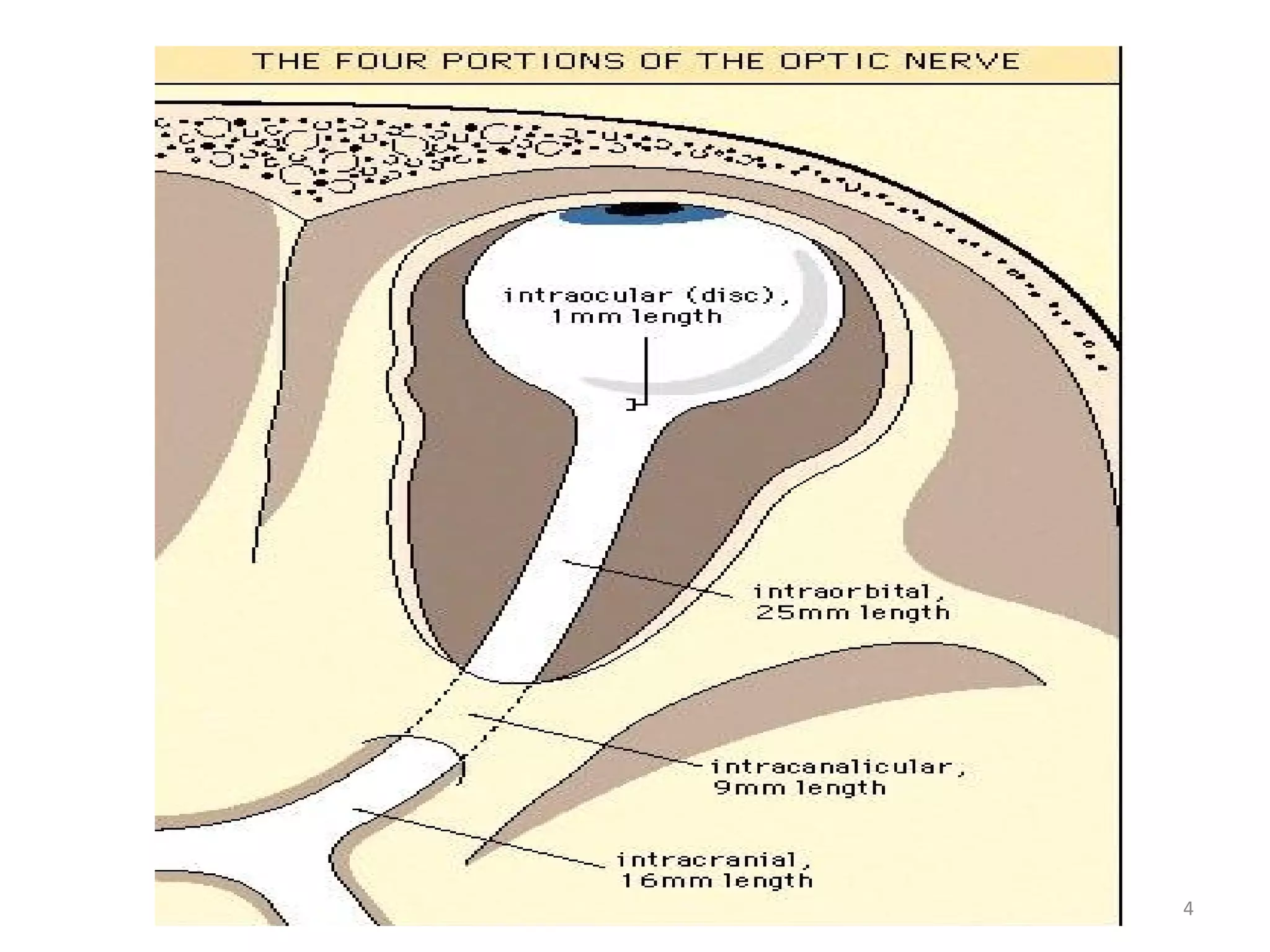
1) It describes the anatomy of the optic nerve, including its origin from the ganglion cells and path from the optic disc to the optic chiasm. It is composed of over 1 million axons and is divided into intraocular, intraorbital, intracanalicular, and intracranial portions.
2) Clinical assessment of the optic nerve involves testing visual acuity, color vision, visual fields, and the pupillary light reflex. Signs of optic nerve pathology include an afferent pupillary defect.
3) Different pathologies like papilledema, optic neuritis, and optic