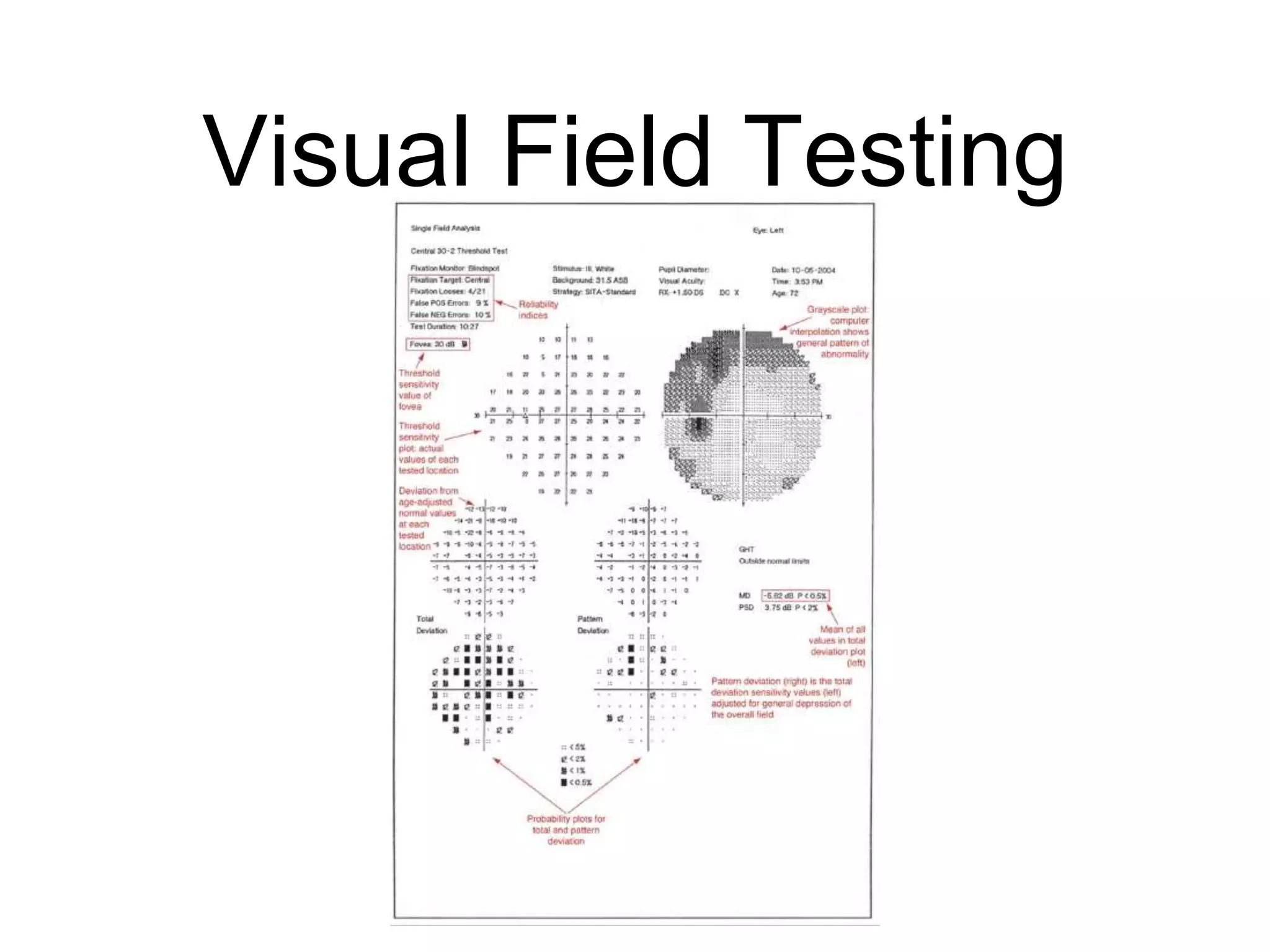
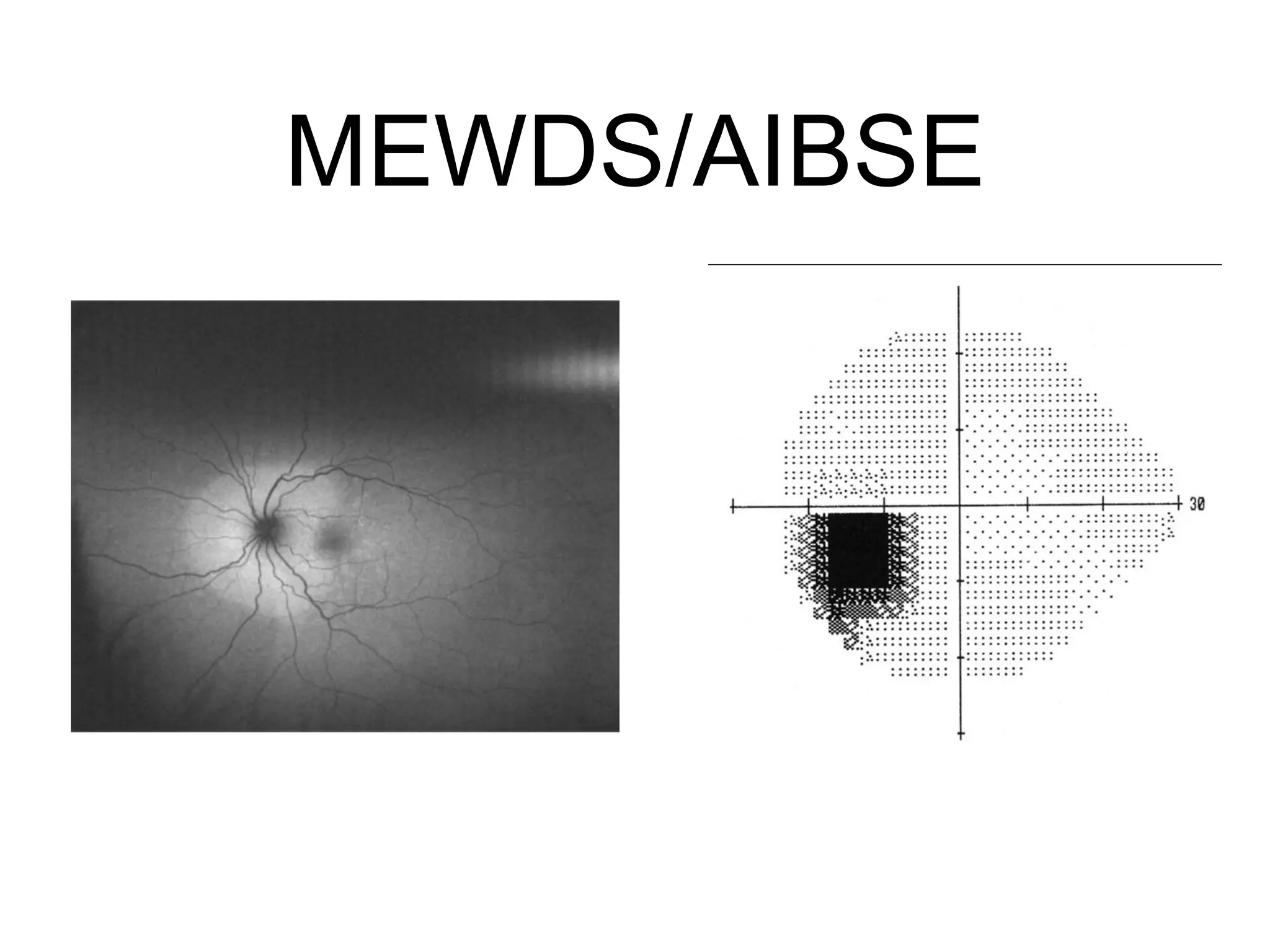
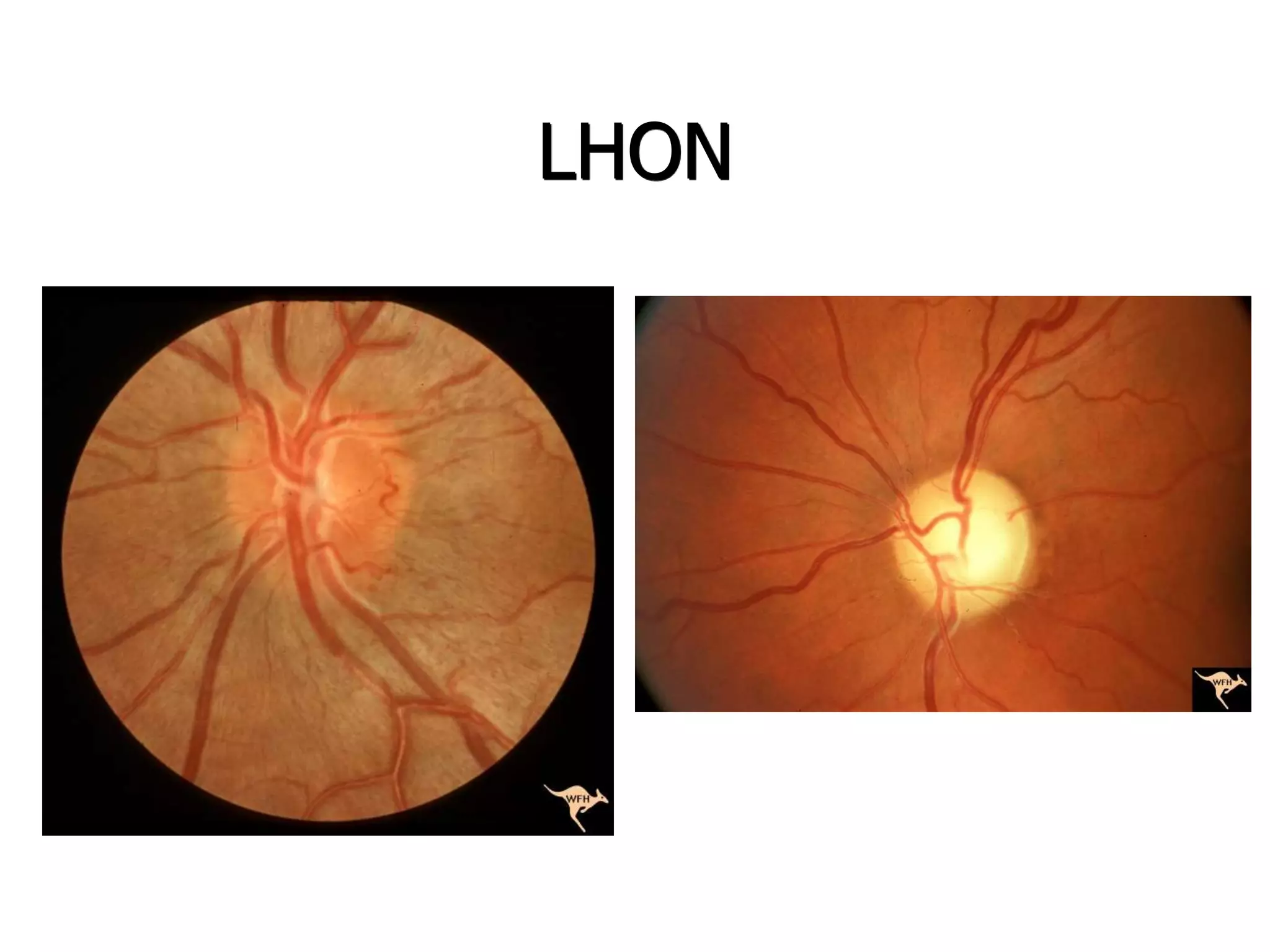
This document provides an overview of evaluating and classifying decreased vision. It discusses evaluating the history, color vision, pupils, fundus, visual fields, and ancillary tests. It then classifies causes as macular, retinal, optic neuropathy, chiasmopathy, visual pathway, or occipital cortex. Specific conditions discussed include NAION, Leber's hereditary optic neuropathy, compressive optic neuropathies, toxic/nutritional neuropathies, and lesions of the chiasm, optic tract, lateral geniculate, and occipital cortex.