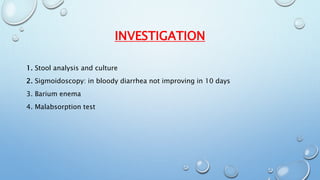
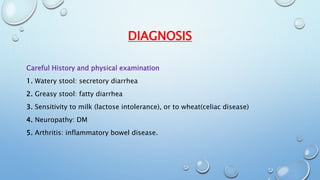
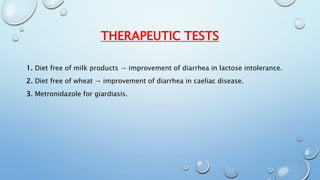
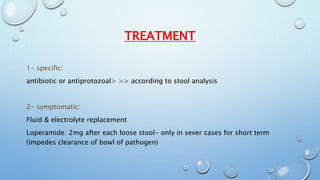
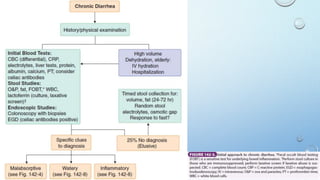
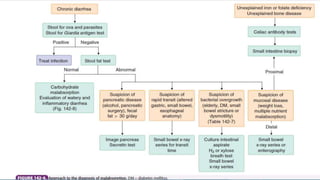
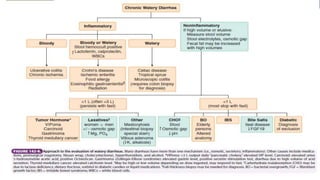
This document discusses the approach to chronic diarrhea. It defines diarrhea and describes the main types: osmotic, secretory, inflammatory, and abnormal motility. Chronic diarrhea is defined as lasting over 4 weeks and can be caused by diseases of the colon or small intestine, endocrinological issues, drugs like antibiotics, or miscellaneous conditions. Diagnosis involves a careful history, physical exam, stool tests, and other imaging exams. Treatment depends on the identified cause, including antibiotics for specific infections or loperamide for symptom relief.