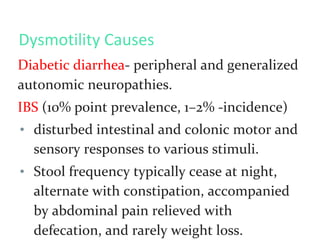
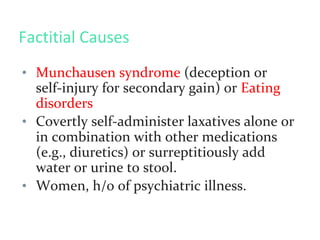
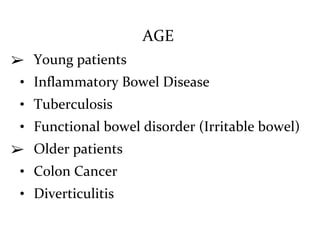
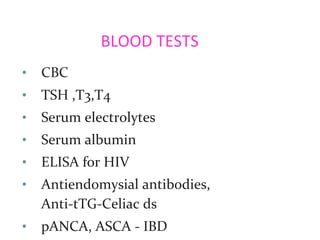
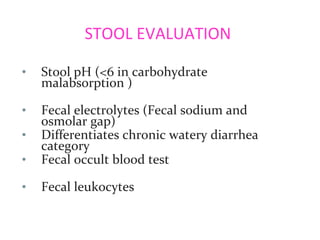
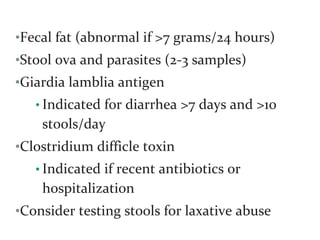
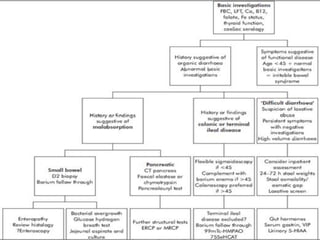
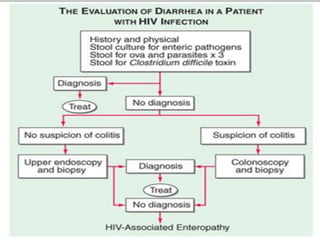
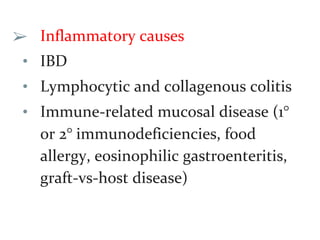
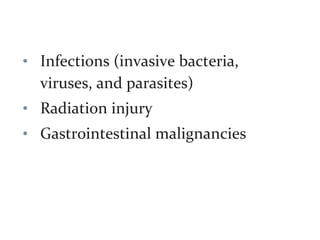
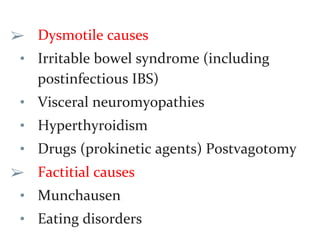
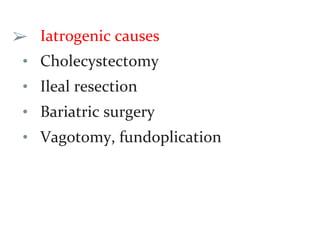
This document defines and classifies chronic diarrhea and outlines its various causes. It discusses secretory, osmotic, steatorrheal, inflammatory, dysmotile, factitial, and iatrogenic causes. A thorough history and physical exam are important to determine the etiology and guide appropriate testing. Common investigations include complete blood count, electrolytes, thyroid function tests, and serologic markers for celiac disease and inflammatory bowel disease. Chronic diarrhea has many potential organic and functional causes and careful evaluation is needed.

![• Medications- most common secretory
causes
• stimulant laxatives [e.g., senna,
cascara, bisacodyl, ricinoleic acid
(castor oil)].
• Chronic ethanol consumption](https://image.slidesharecdn.com/chronicdiarrhoea-190521161818/85/Chronic-diarrhoea-15-320.jpg)
![Congenital Defects in Ion Absorption
• Defective Cl–/HCO3– exchange (congenital
chloridorrhea) with alkalosis (mutated DRA
[down-regulated in adenoma] gene)
• Defective Na+/H+ exchange (congential
sodium diarrhea)with acidosis ( mutation in
the NHE3 [sodium-hydrogen exchanger]
gene)
• Adrenocortical insufficiency-diarrhoea
accompanied by skin hyperpigmentation.](https://image.slidesharecdn.com/chronicdiarrhoea-190521161818/85/Chronic-diarrhoea-22-320.jpg)

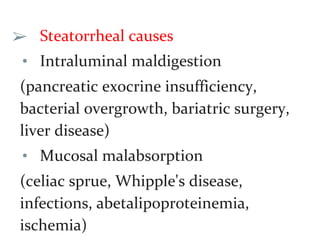
![Osmotic Laxatives
• Mg-containing antacids, health
supplements, or laxatives
• stool osmotic gap (>50 mosmol/L):
serum osmolarity (typically 290
mosmol/kg)-[2 x (fecal sodium +
potassium concentration)].](https://image.slidesharecdn.com/chronicdiarrhoea-190521161818/85/Chronic-diarrhoea-25-320.jpg)