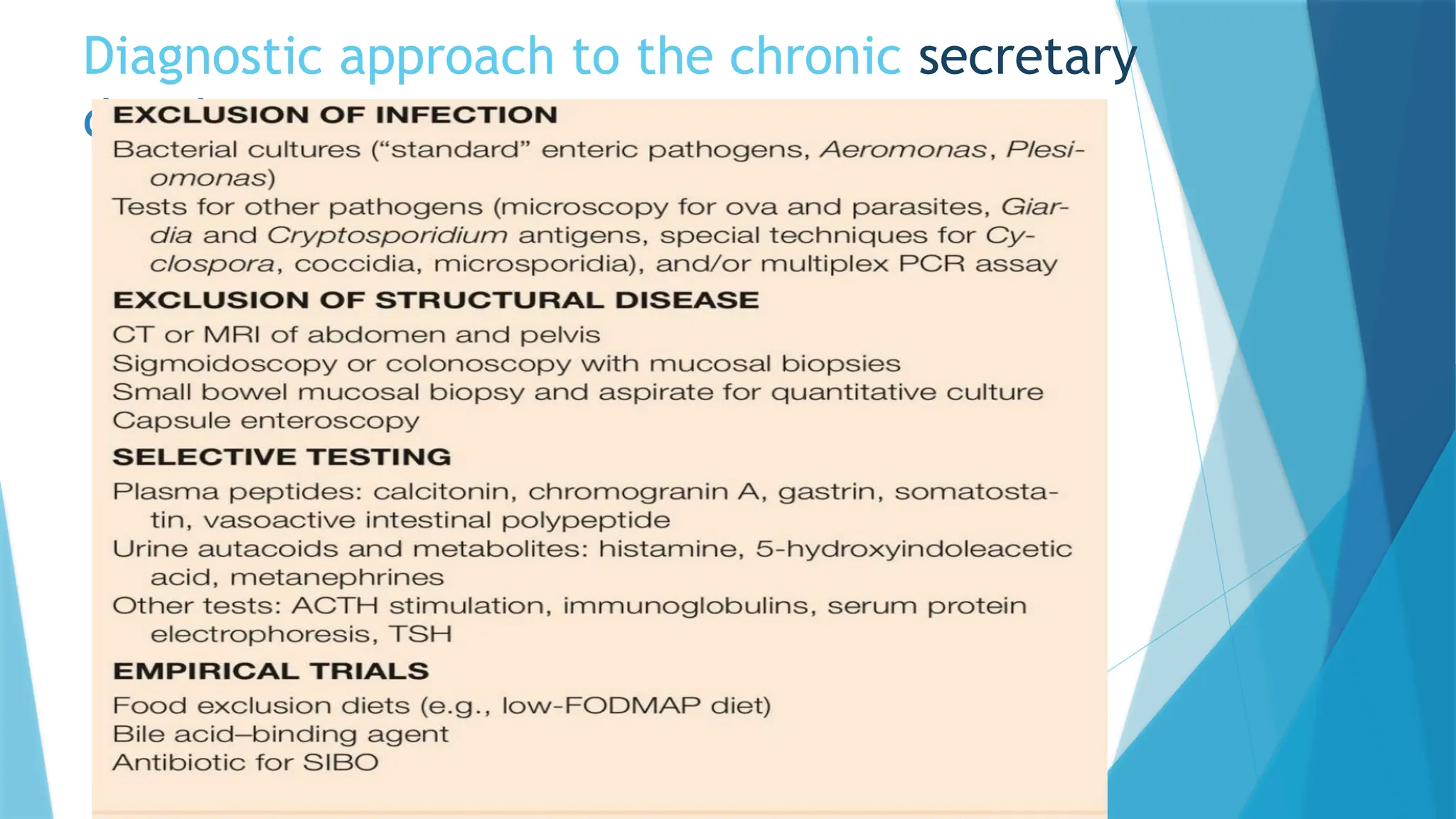
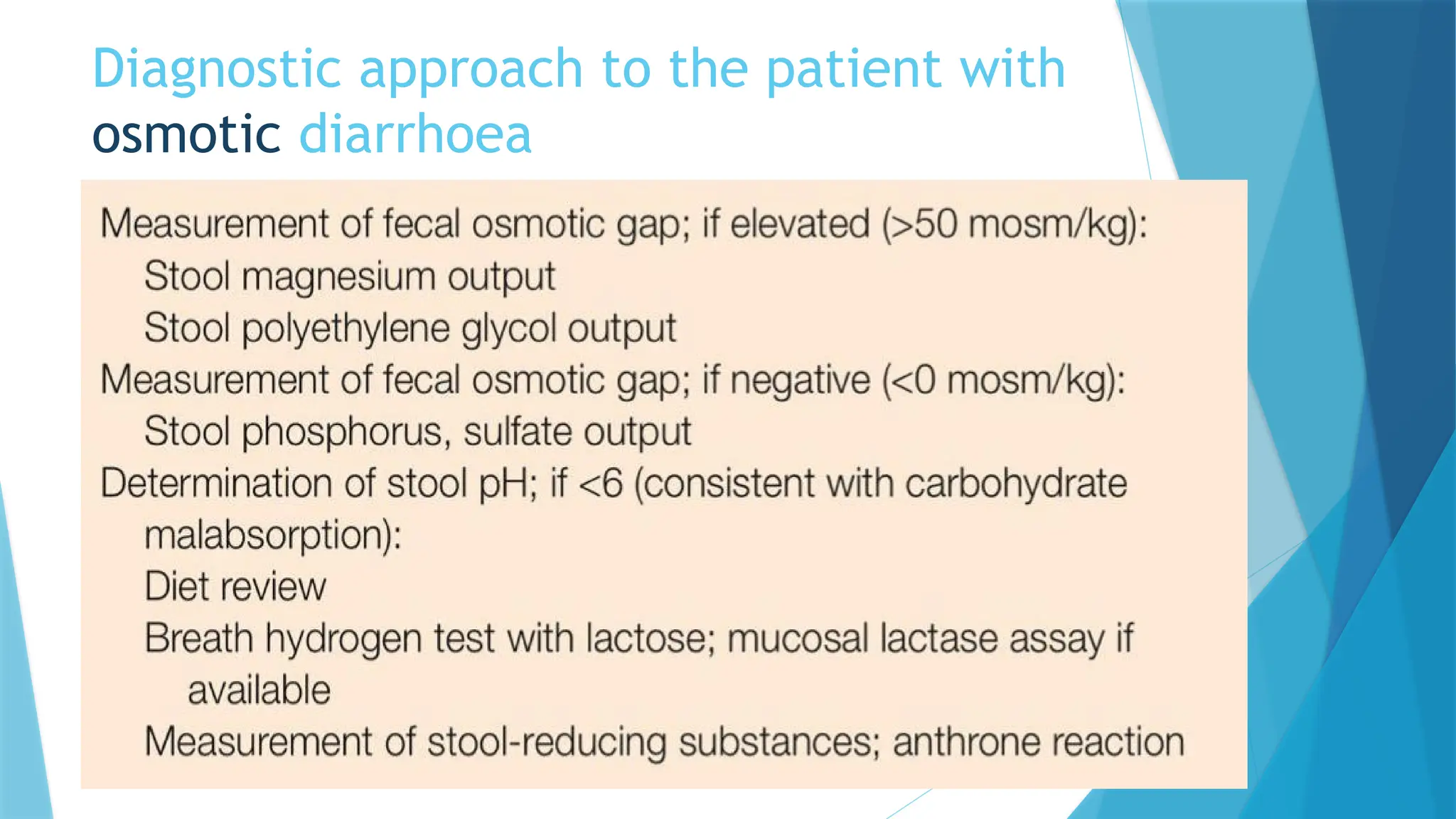
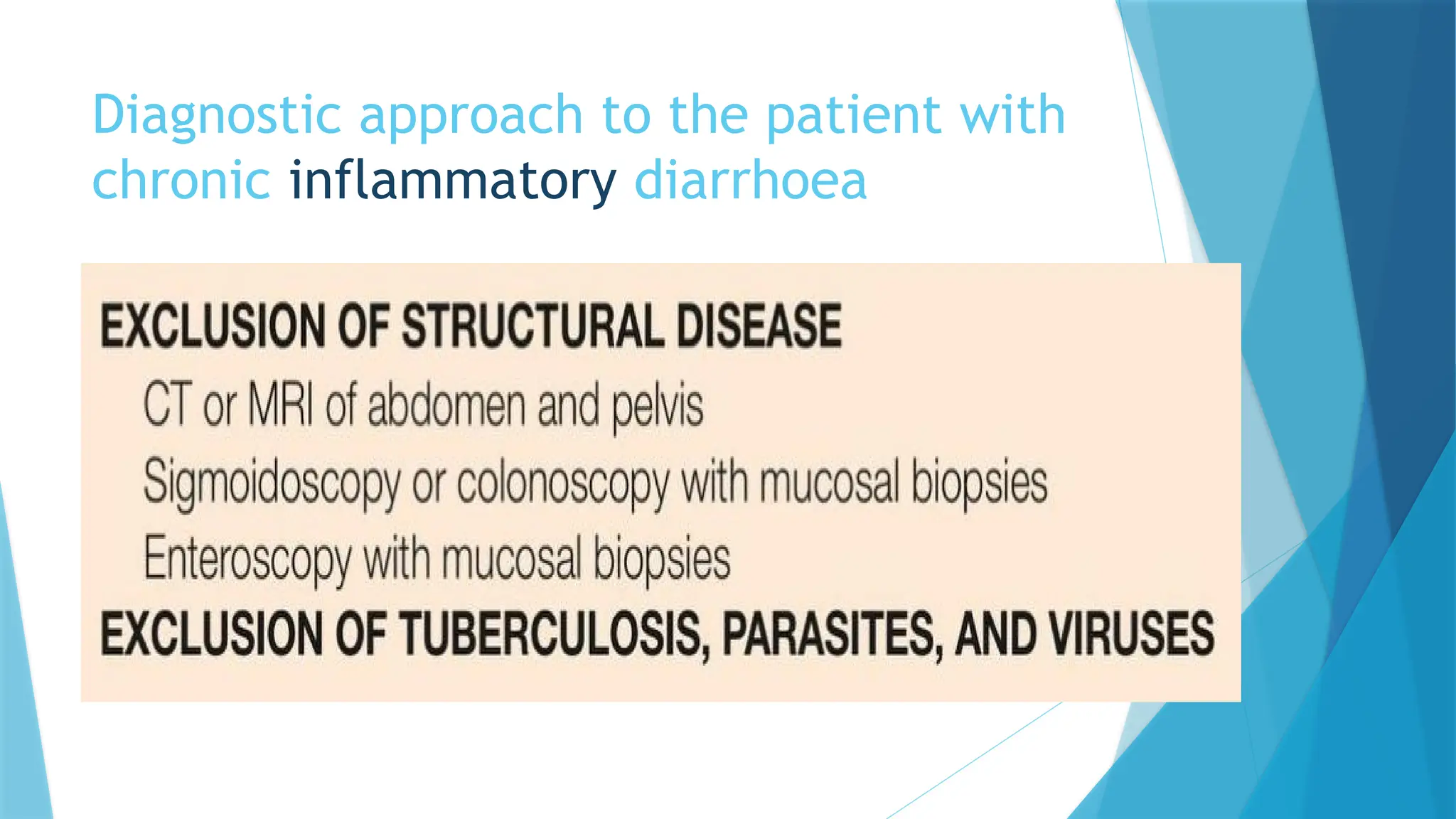
Chronic diarrhea, defined as the passage of three or more loose or liquid stools per day for over four weeks, can have multiple non-infectious causes, classified into secretory, osmotic, steatorrheal, inflammatory, dysmotility, factitial, and iatrogenic. Diagnosis involves assessing stool characteristics, patterns, and a range of diagnostic tests including blood tests and stool analysis to identify specific underlying conditions. Treatment primarily focuses on fluid and electrolyte replenishment, with additional options depending on the underlying cause, such as enzyme replacements and probiotics.




![SECRETORY DIARRHEA
Due to derangements in fluid and electrolyte transport across
the entero-colonic mucosa.
The mechanism is net secretion of anions ( chloride or
bicarbonate ),potassium or net inhibition of sodium
absorption.
Lack of sufficient absorptive surface area limits electrolyte
absorption (sodium ).
Characterized by -watery ,large volume fecal output,painless
and persist with fasting.
No or <50mosm/kg fecal osmotic gap
[Fecal osmotic gap=serum osmolarity-{2*(fecal Na+K conc.)}]](https://image.slidesharecdn.com/chronicdiarrhea-7-241124174433-48630580/75/CHRONIC-DIARRHEA-an-symptomatic-approach-pptx-5-2048.jpg)