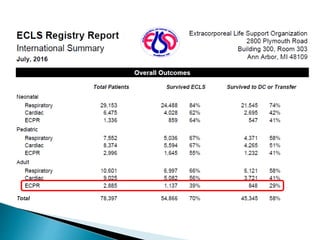
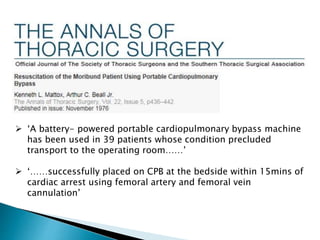
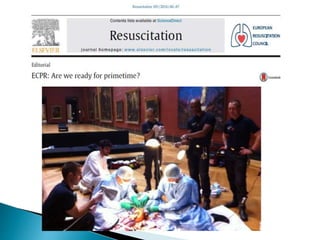
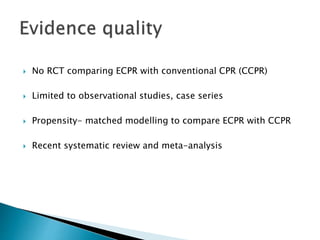
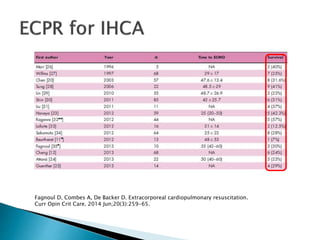
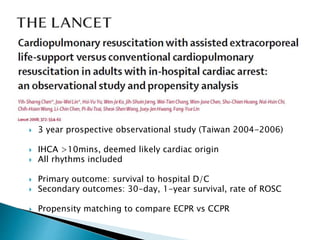
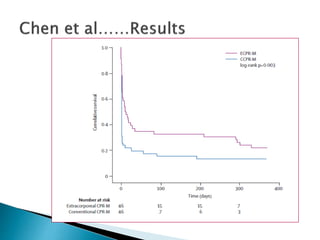
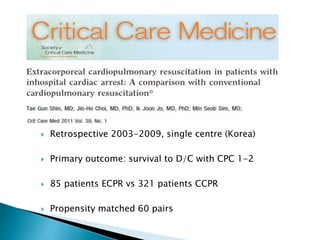
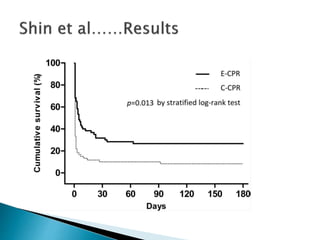
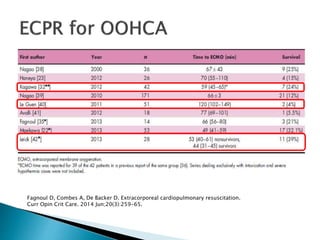
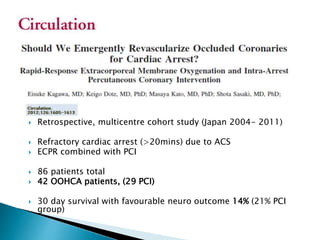
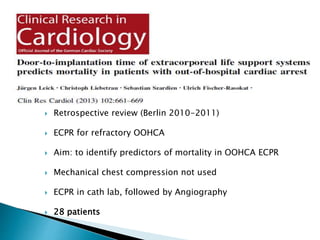
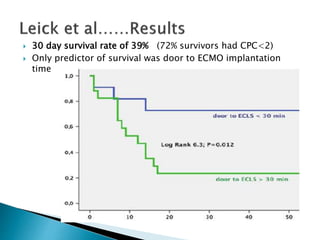
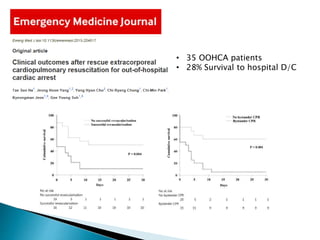
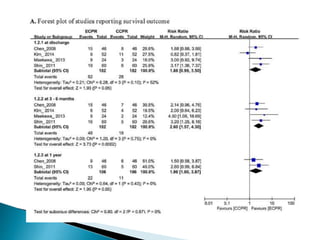
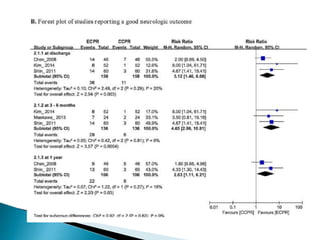
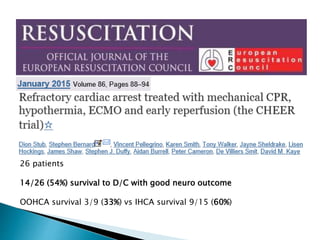
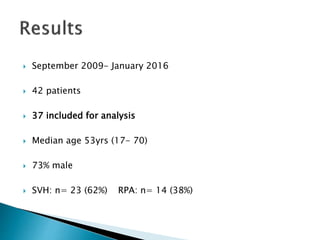
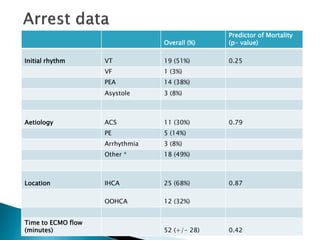
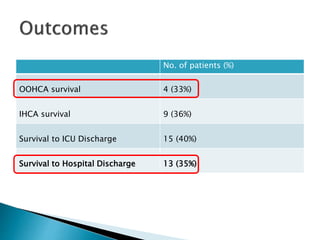
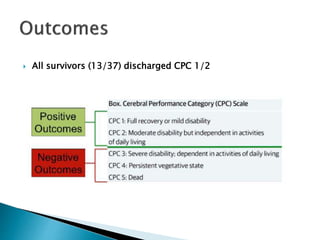
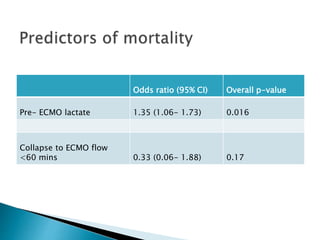
The document discusses the deployment of extracorporeal membrane oxygenation (ECMO) during cardiac arrest, highlighting its potential advantages over conventional CPR, particularly in cases of refractory cardiac arrest. It summarizes findings from various studies, showing survival rates and outcomes associated with ECMO compared to traditional methods, noting the importance of timely intervention and system logistics. Overall, the analysis suggests that ECMO can lead to favorable outcomes in selected patients, although further research is still needed.