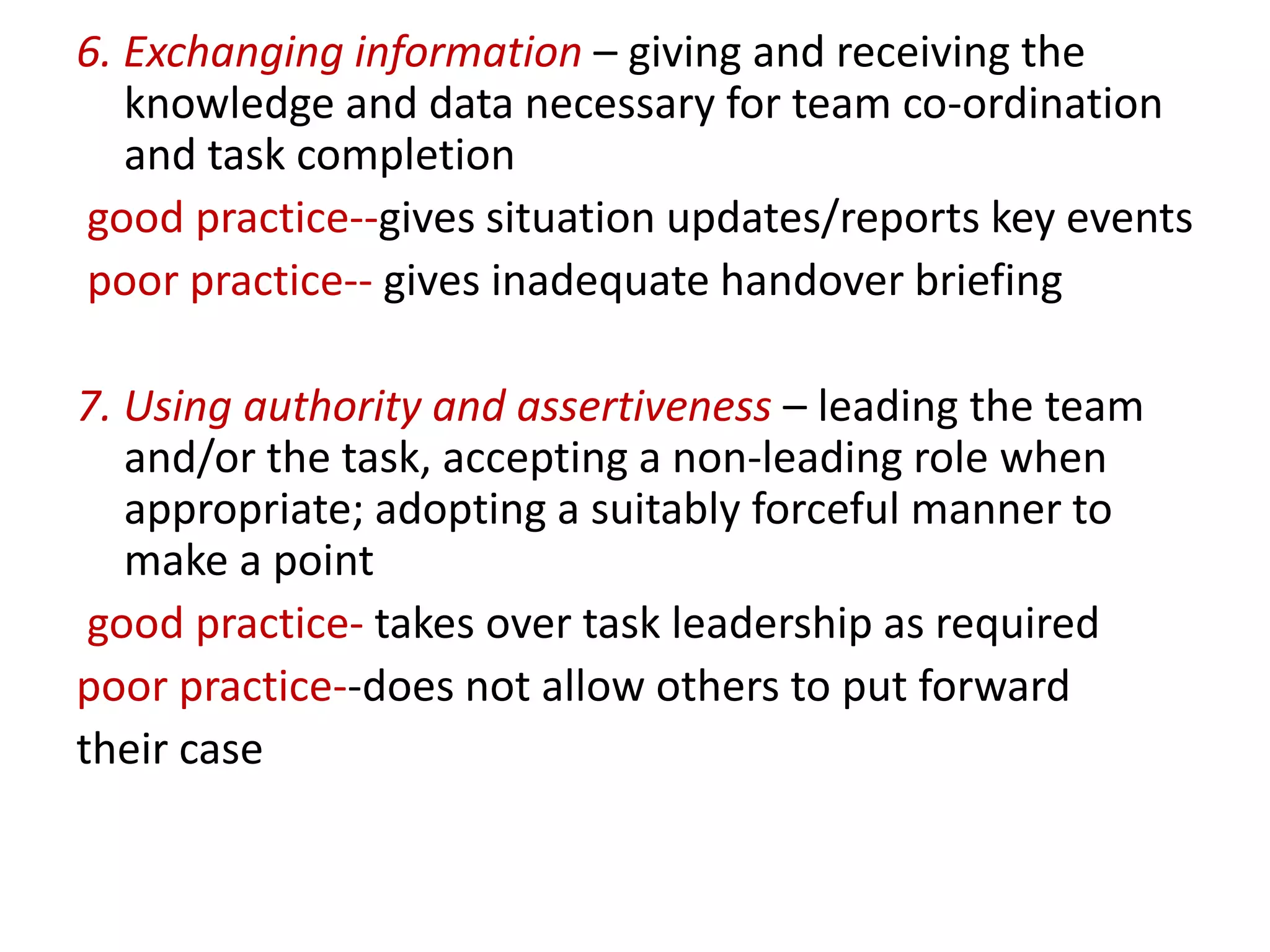
The document discusses non-technical skills that are important for anesthesiologists, including situation awareness, decision making, teamwork, and stress management. It describes how the Anesthetists' Non-Technical Skills (ANTS) system was developed to identify and rate non-technical skills in four categories (task management, team working, situation awareness, and decision making) based on observational studies. The ANTS system provides a standardized way to assess and provide feedback on anesthesiologists' non-technical performance.