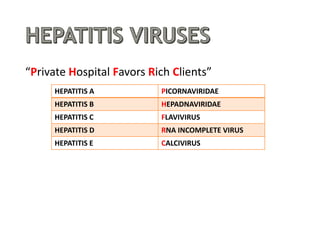
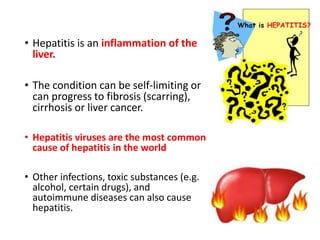
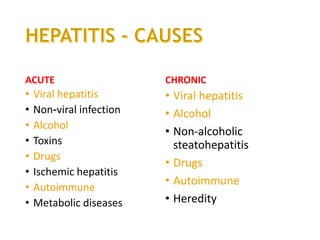
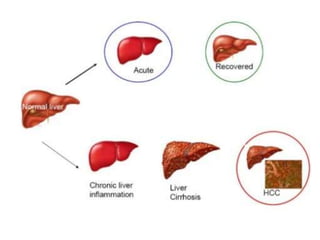
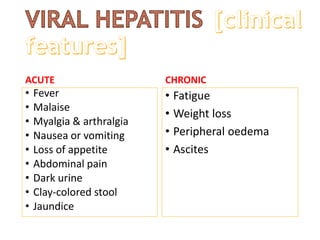
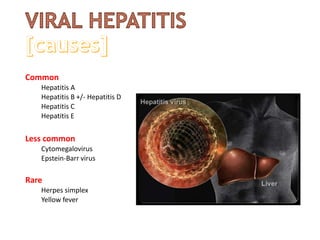
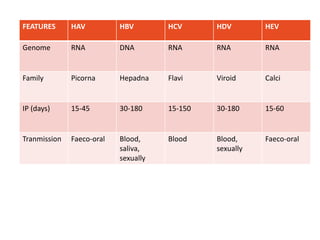
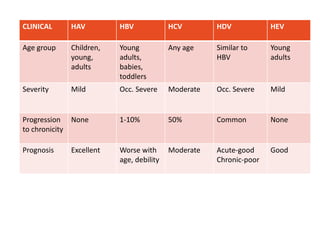
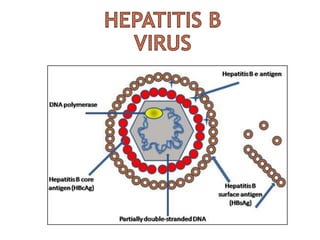
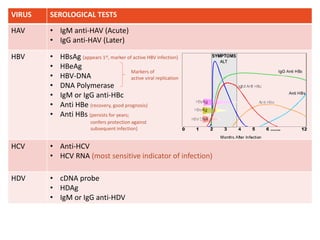
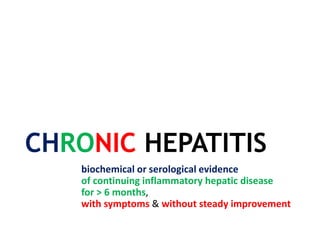
Hepatitis is an inflammation of the liver that can be caused by viruses, toxic substances like alcohol, or autoimmune diseases. The document discusses the different types of hepatitis, including acute and chronic forms. It provides details on hepatitis viruses A through E, describing their genomes, incubation periods, modes of transmission, clinical features, and recommended treatments. Chronic hepatitis B and C are managed primarily through antiviral drug therapy and occasionally liver transplantation.

![• ALT, AST
[N: <40 units]
• ALP
[N: 30-120 IU/L]
• Plasma bilirubin
>2.5 mg/dL up to 20 mg/dL
• Prolong PT
[N: 11.5-12.5 seconds]
• Hypoglycemia
• Serological tests](https://image.slidesharecdn.com/viralhep-150507132644-lva1-app6892/85/VIRAL-HEPATITIS-10-320.jpg)
![CHRONIC HEPATITIS B
[management]
2 drugs are used
• Direct acting nucleoside/nucleotide analogues
• Lamivudine 100mg daily orally
• Adefovir 10mg daily orally
• Entecavir 0.5mg orally
• Pegylated interferon-α
• IFN- α 2a&2b: SC 10 million units thrice weekly
or 5 million units daily
• IFN- α 2a: 180 mcg weekly
• IFN- α 2b: 100 mcg weekly
Liver transplantation
• Indicated FHF and ESLD
• Combined nucleoside analogue + hep B Ig therapy
For 48 weeks
For 6 months
For 48 weeks](https://image.slidesharecdn.com/viralhep-150507132644-lva1-app6892/85/VIRAL-HEPATITIS-19-320.jpg)
![CHRONIC HEPATITIS C
[management]
GROUP I GROUP II GROUP III GROUP IV
Anti-HCV + + + -
HCV RNA - + + +
ALT NI NI Raised NI
Management No treatment Under follow-
up
IFN + Ribavirin Liver biopsy](https://image.slidesharecdn.com/viralhep-150507132644-lva1-app6892/85/VIRAL-HEPATITIS-20-320.jpg)
![CHRONIC HEPATITIS C
[management]
GROUP I GROUP II GROUP III GROUP IV
Anti-HCV + + + -
HCV RNA - + + +
ALT NI NI Raised NI
Management No treatment Under follow-
up
IFN + Ribavirin Liver biopsy
Peg IFN-α 2a 180mcg SC weekly
or Peg IFN-α 2b 1.5mcg/kg SC
weekly
+
Ribavirin 1000-1200 mg/day
orally for 48 weeks](https://image.slidesharecdn.com/viralhep-150507132644-lva1-app6892/85/VIRAL-HEPATITIS-21-320.jpg)
![CHRONIC HEPATITIS C
[management]
GROUP I GROUP II GROUP III GROUP IV
Anti-HCV + + + -
HCV RNA - + + +
ALT NI NI Raised NI
Management No treatment Under follow-
up
IFN + Ribavirin Liver biopsy
Peg IFN-α 2a 180mcg SC weekly
or Peg IFN-α 2b 1.5mcg/kg SC
weekly
+
Ribavirin 1000-1200 mg/day
orally for 48 weeks
Peg IFN-α 2a 180mcg SC weekly
or Peg IFN-α 2b 1.5mcg/kg SC
weekly
+
Ribavirin 800 mg/day orally for
24 weeks](https://image.slidesharecdn.com/viralhep-150507132644-lva1-app6892/85/VIRAL-HEPATITIS-22-320.jpg)