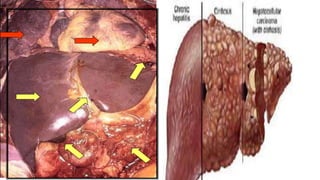
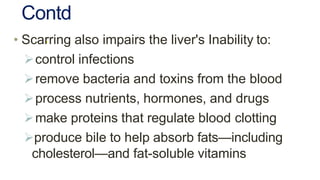
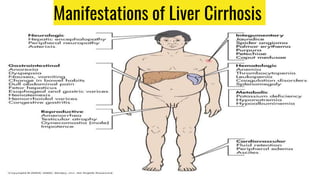
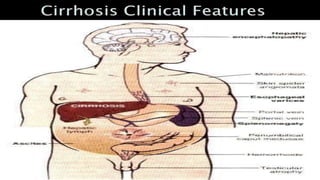
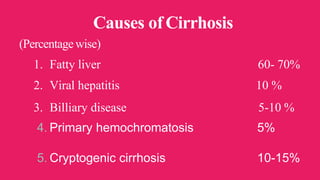
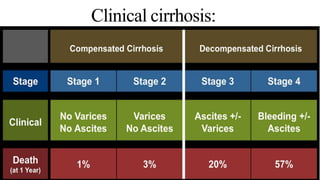
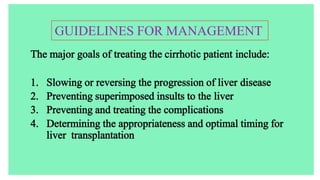
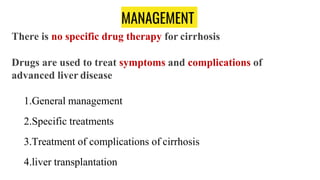
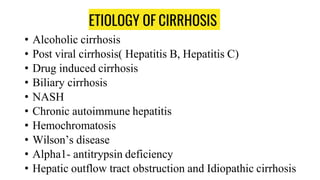
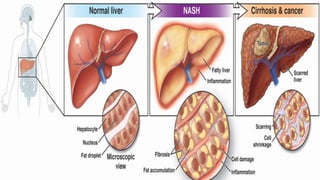
This document discusses liver cirrhosis, including its definition, causes, clinical presentation, management, and treatment of complications. Cirrhosis is characterized by the replacement of liver tissue with scar tissue, leading to loss of liver function. The most common causes are fatty liver disease, viral hepatitis, and alcohol use. Management involves treating the underlying cause, managing complications, and liver transplantation for severe cases. Complications like ascites, bleeding, and encephalopathy are treated through dietary changes, medications, and procedures.


![TREATMENT BASED ON AETIOLOGY
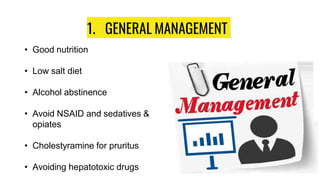
• Alcoholic cirrhosis-
1. Complete abstinence from alcohol
2. Nutritional support(>3000kcal/day) along with multivitamins
3. Prednisolone and Pentoxifylline in severe cases.
4. Pentoxifylline is a hemorrheologic agent, Anti-inflammatory agent.
5. ADR of Pentoxifylline:-
Cyto-toxic effect in Preclinical studies[1].
6. The findings suggest that the administration of 40 mg
of prednisolone daily for 1 month may have a beneficial effect on short-
term mortality but not on the medium-term or long-term outcome
of alcoholic cirrhosis.[2]`](https://image.slidesharecdn.com/livercirrhosis-201218045624/85/Liver-cirrhosis-Management-15-320.jpg)
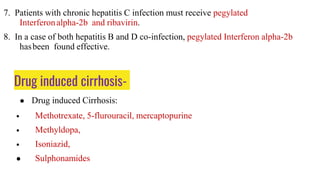
![• Post viral cirrhosis-
1. For chronic hepatitis B infection, Interferon alpha-2b (5 million units daily s.c.
or 10 million units thrice a week for 4-6 months);
2. lamivudine 100mg once daily until HBeAg becomes negative ; entecavir,
tenofovir, adefovir dipivoxil or telbivudine can also be tried.
3. The combination of tenofovir and efavirenz with
either lamivudine or emtricitabine (TELE) has proved to be highly effective
in clinical trials for first-line treatment of HIV-1 infection[3].
4. Lamivudine, entecavir, tenofovir, adefovir dipivoxil or telbivudine comes under
Anti-retroviral nucleoside Reverse Transcriptase Inhibitor
5. Major ADR is NRTI is Thrombocytopenia (decreased level of Platelet)
6. Management of Thrombocytopenia:- Blood transfusion to temporarily increase
platelet levels in your blood. .. And prescribe the steroids[6].](https://image.slidesharecdn.com/livercirrhosis-201218045624/85/Liver-cirrhosis-Management-16-320.jpg)
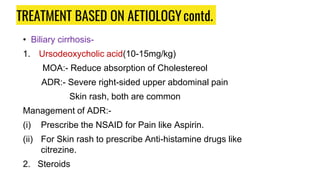
![3. Azathioprine(50mg tab), colchicine (500 microgram tab),
methotrexate 3.3 mg/m2/day orally or cyclosporine 600mg BD are
immunosuppresant.
Among them Immunosuppresent, Azathioprine have more efficacy
compared to other drugs[7].
4. Limit fat intake
5. Monthly injections of vitamin K
6. NASH (Non alcoholic steatohepatitis)
(i) Control of weight, Diabetes and hyperlipidemia
(ii) Metformin 500 mg BD, pioglitazone 15 mg Tab, UDCA,
pentoxyfylline and atorvastatin might be helpful](https://image.slidesharecdn.com/livercirrhosis-201218045624/85/Liver-cirrhosis-Management-19-320.jpg)

![MANAGEMENT OF COMPLICATIONS
Ascites:-
• Bed rest
• Low salt diet (4-6g of salt)
• Avoid NSAIDs
• Fluid restriction to 1-1.5L/24 hr
• Spironolactone 25mg/6 hr orally and increase dose every 48 hr to
400mg/24hr; triamtereneand amiloride can also be tried, but Spironolactone
is more efficacy[4] . Frusemide can be added to the abovetherapy.
• Diuretics should be stopped if there is severe hyponatremia](https://image.slidesharecdn.com/livercirrhosis-201218045624/85/Liver-cirrhosis-Management-26-320.jpg)
![MANAGEMENT OF COMPLICATIONS contd.
Spontaneous bacterial peritonitis
• I.V cefotaxime 2g 8 hourly for 5 days; alternate therapy includes
amoxicillin/clavulanate(1.2g iv 8 hourly followed by 625mg orally) or
ciprofloxacin(200 mg iv 12 hourly followed by 500mg BID) or
ofloxacine(400mg twice daily) in patients with hepatic encephalopathy.
Efficacy - Albumin along with antibiotics reduces risk of hepatic
encephalopathy[5].
• Prophylaxis- ciprofloxacin 750mg or cotrimoxazole 960mg once weekly.](https://image.slidesharecdn.com/livercirrhosis-201218045624/85/Liver-cirrhosis-Management-27-320.jpg)