This document discusses ventilators, their types, modes, and use in assisting patients with respiratory failure. It covers:
1) There are two main types of ventilators - invasive, which require an endotracheal or tracheostomy tube, and non-invasive which use face or nasal masks.
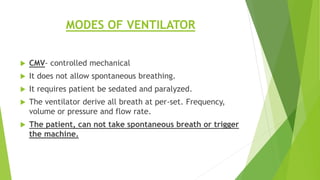
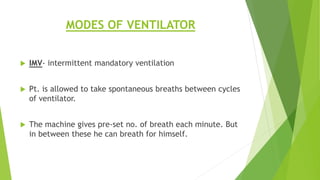
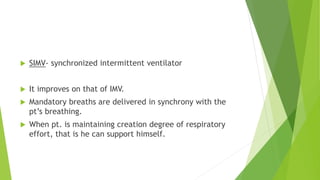
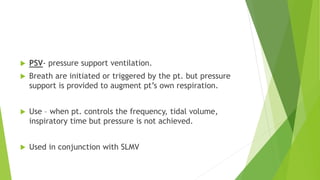
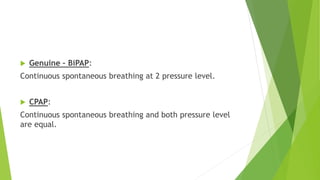
2) Modes include CMV for full support, and modes like SIMV, PSV, and BiPAP that allow some spontaneous breathing.
3) Weaning involves gradually reducing ventilator support using modes that promote patient breathing, like SIMV, PSV, BiPAP, and CPAP. Parameters are monitored to ensure patient readiness before removing all support.