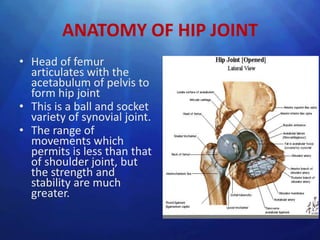
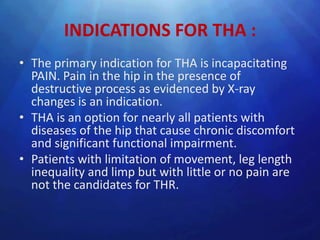
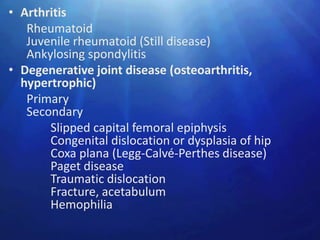
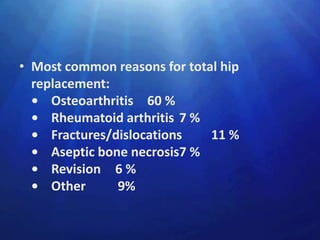
- Total hip arthroplasty involves replacing the hip joint with prosthetic components. It is commonly performed for arthritis and other hip diseases.
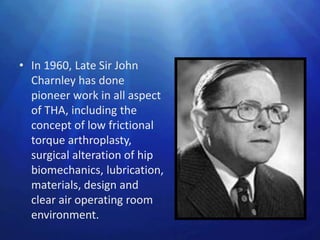
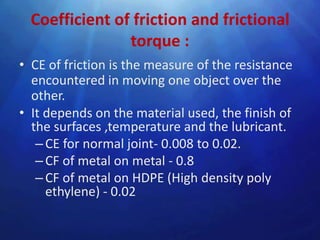
- The procedure has evolved significantly since the early attempts in the 1900s using materials like gold foil and glass. Modern THA designs aim to reduce friction and stress on the implants.
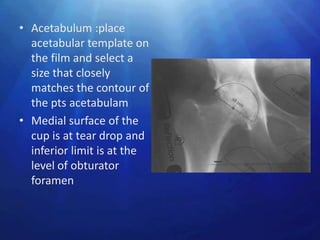
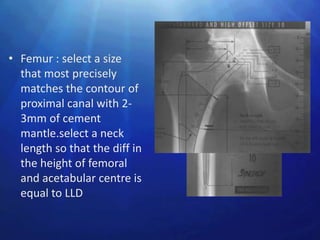
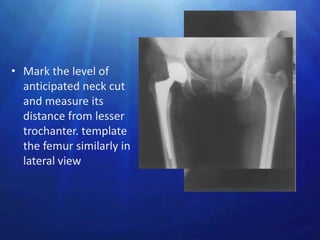
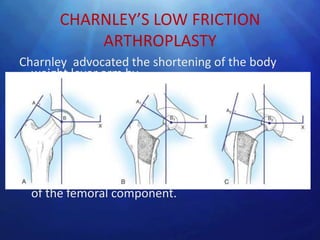
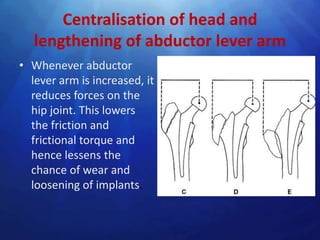
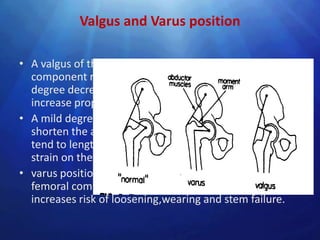
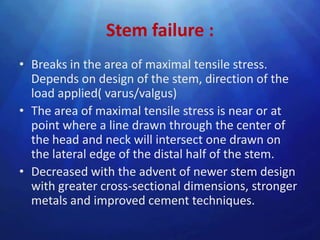
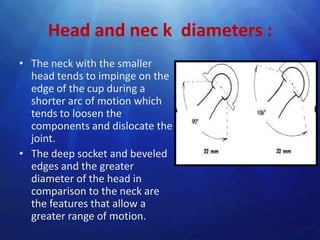
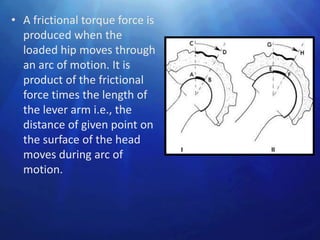
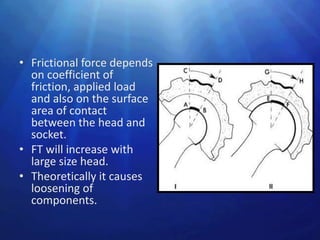
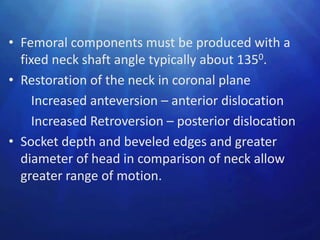
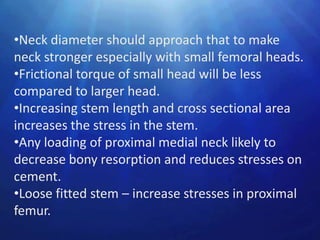
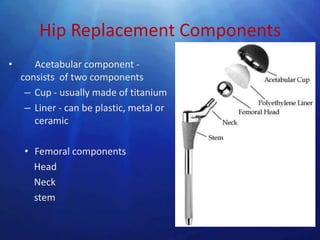
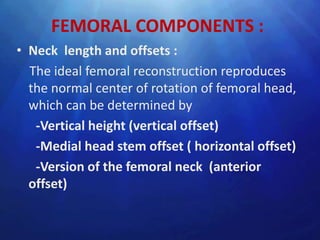
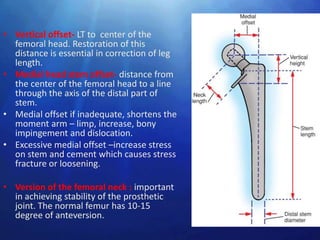
- Key considerations in THA include restoring normal hip biomechanics, maximizing stability while allowing a full range of motion, and minimizing wear on the prosthetic components over many years. Proper positioning and design of the femoral stem and acetabular cup are important.






![Metal-on-Metal Bearings
• Metal-on-metal implants seem to be tolerant of
high impact loading, and mechanical failure has
not been reported.
• wear rates less than 10 mm/y for modern metal-
on-metal articulations
• But there remains major concern regarding the
production of cobalt and chromium metallic
debris, and its elimination from the body.
• metal-on-metal (MOM) bearings have a ‘suction-
fit’ less chance of dislocation
(J Bone Joint Surg [Br] 2003;85-B:650-4)](https://image.slidesharecdn.com/thr-ashok-130219100027-phpapp02/85/Total-hip-arthroplasty-63-320.jpg)
![Ceramic-on-Ceramic Bearings
• Alumina ceramic has many properties that make it
desirable as a bearing surface in hip arthroplasty
• high density- surface finish smoother than metal
implants
• The hydrophilic nature- ceramic promotes lubrication
• Ceramic is harder than metal and more resistant to
scratching from third-body wear particles.
• The linear wear rate of alumina-on-alumina has been
shown to be 4000 times less than cobalt-chrome alloy–
on–polyethylene.
• Ceramic-on-ceramic arthroplasties may be more
sensitive to implant malposition than other bearings. (J
Bone Joint Surg [Br] 2003;85-B:650-4](https://image.slidesharecdn.com/thr-ashok-130219100027-phpapp02/85/Total-hip-arthroplasty-64-320.jpg)