This document provides information about pyelonephritis (kidney infection) including:
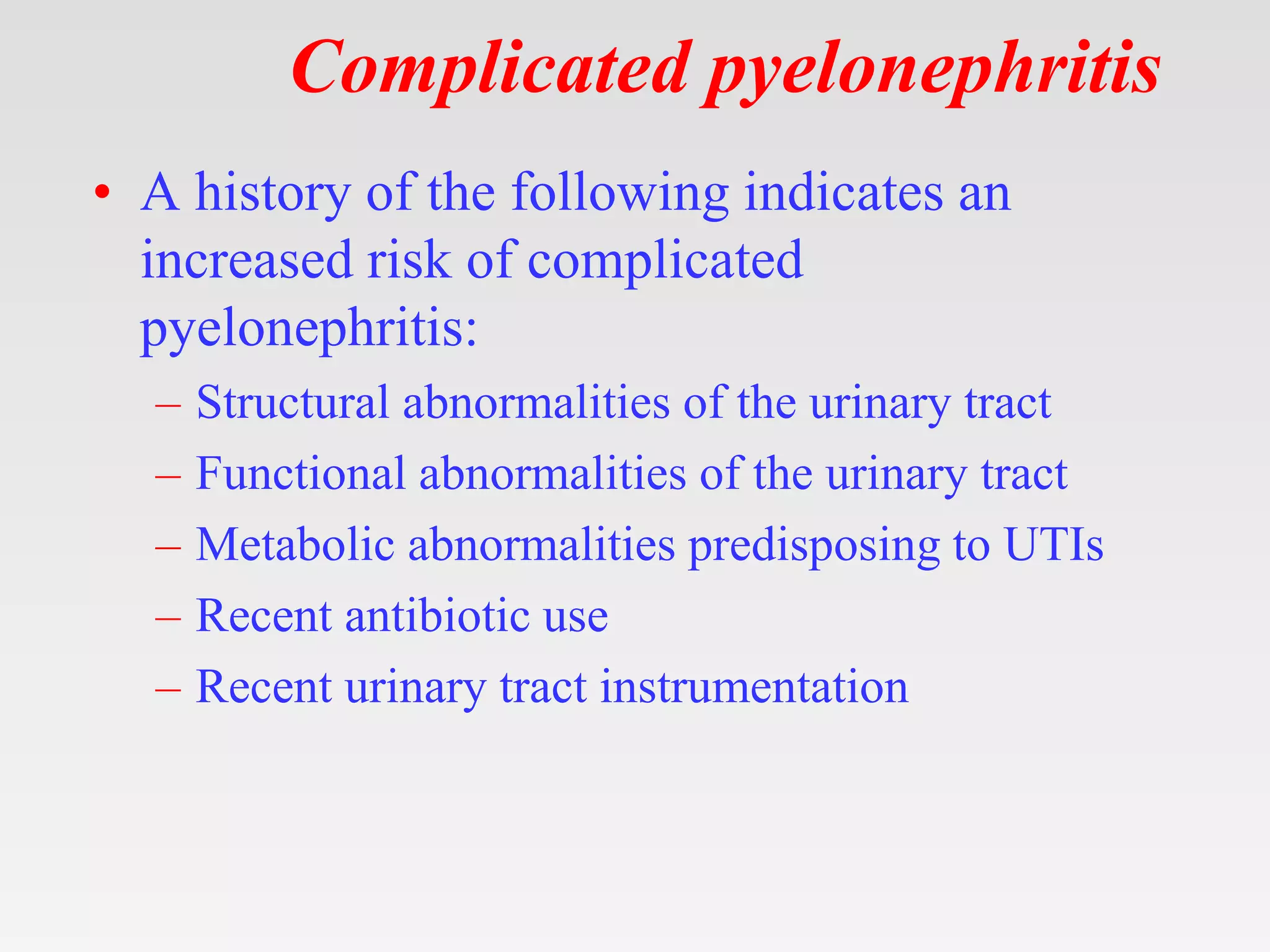
1. It defines pyelonephritis as an infection of the kidney and ureters that can be life-threatening.
2. Causes include urinary tract infections ascending from the bladder or entering via the bloodstream.
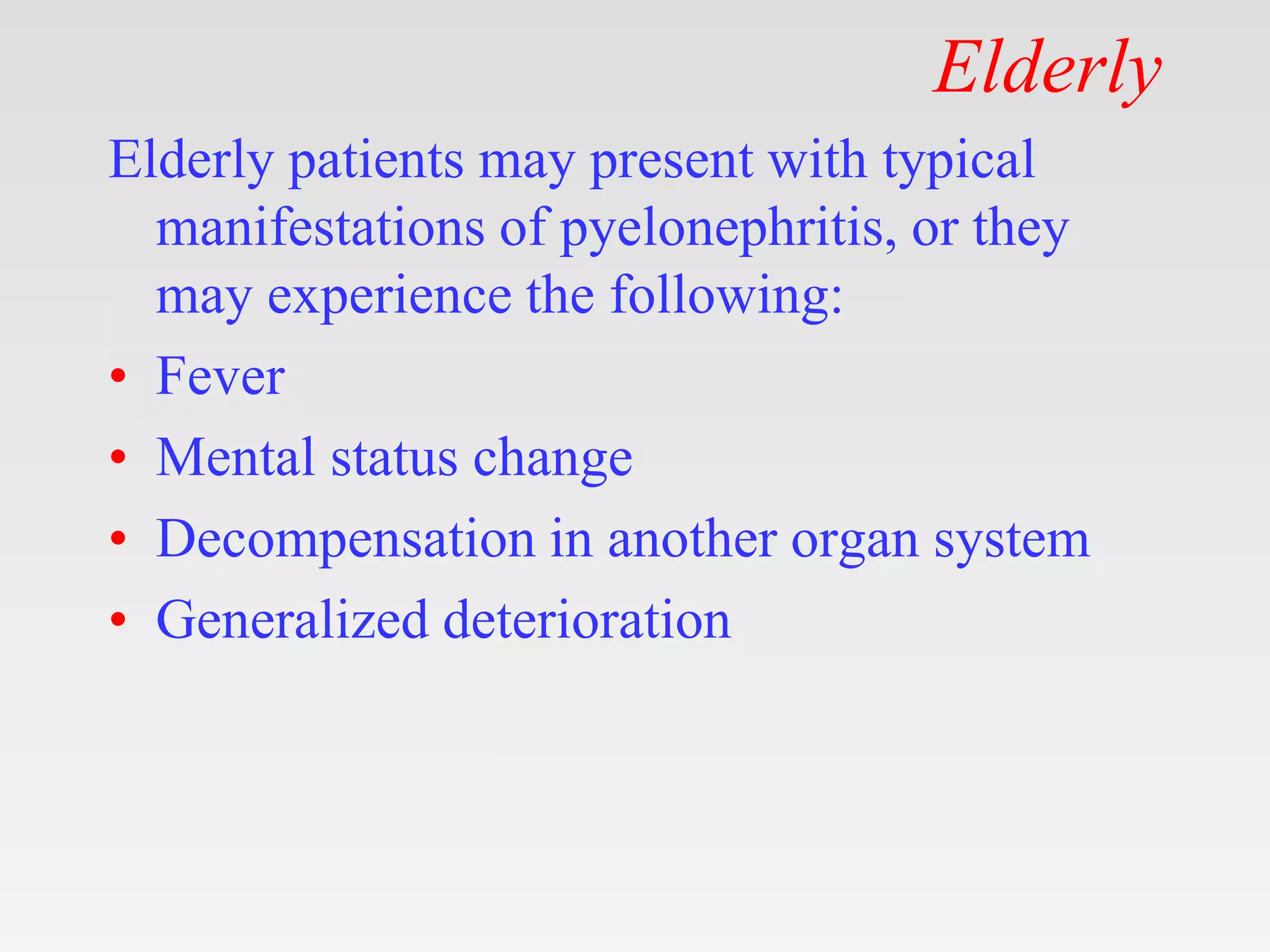
3. Symptoms vary depending on age but usually include fever, flank pain, nausea, and urinary symptoms.
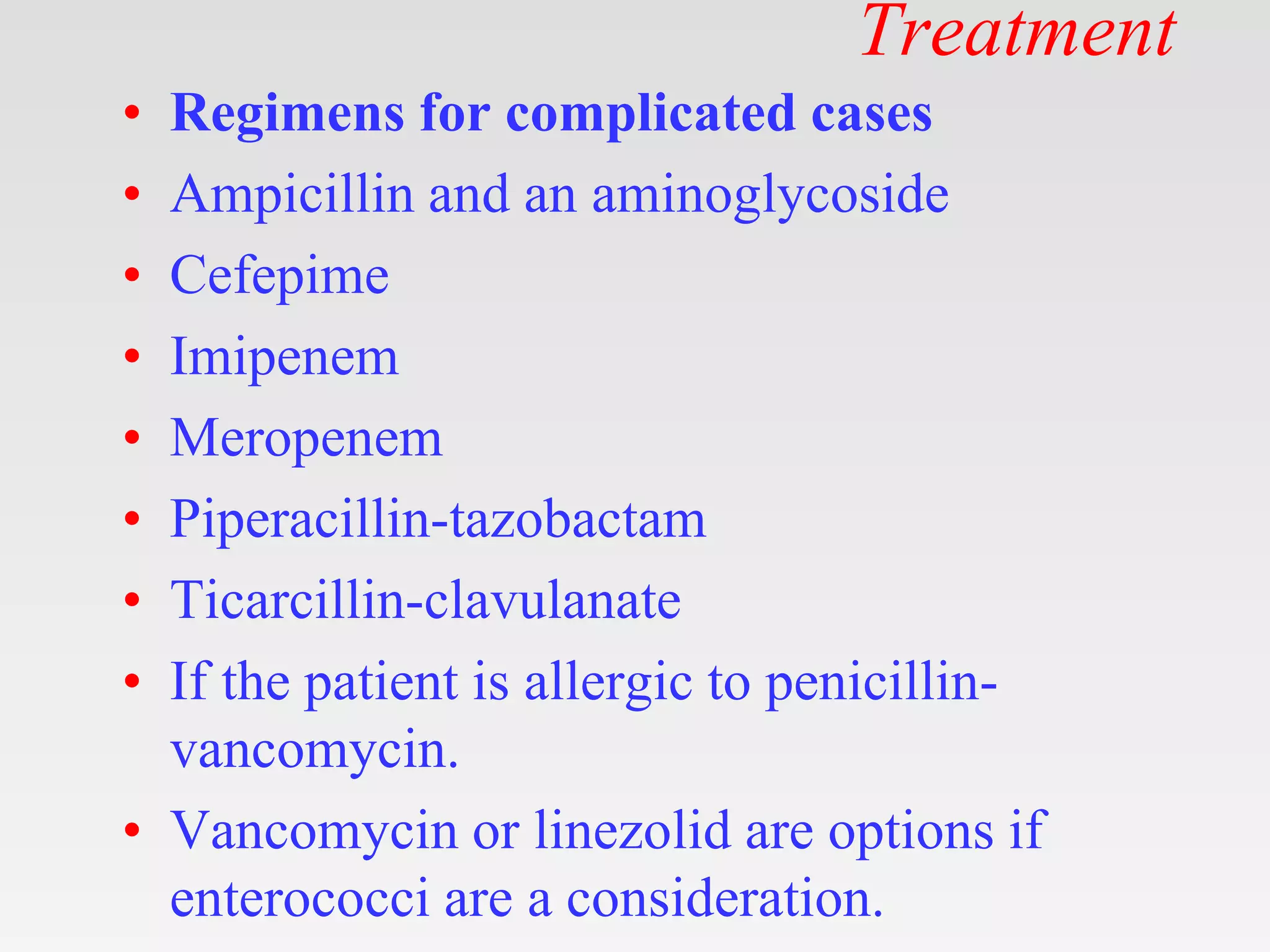
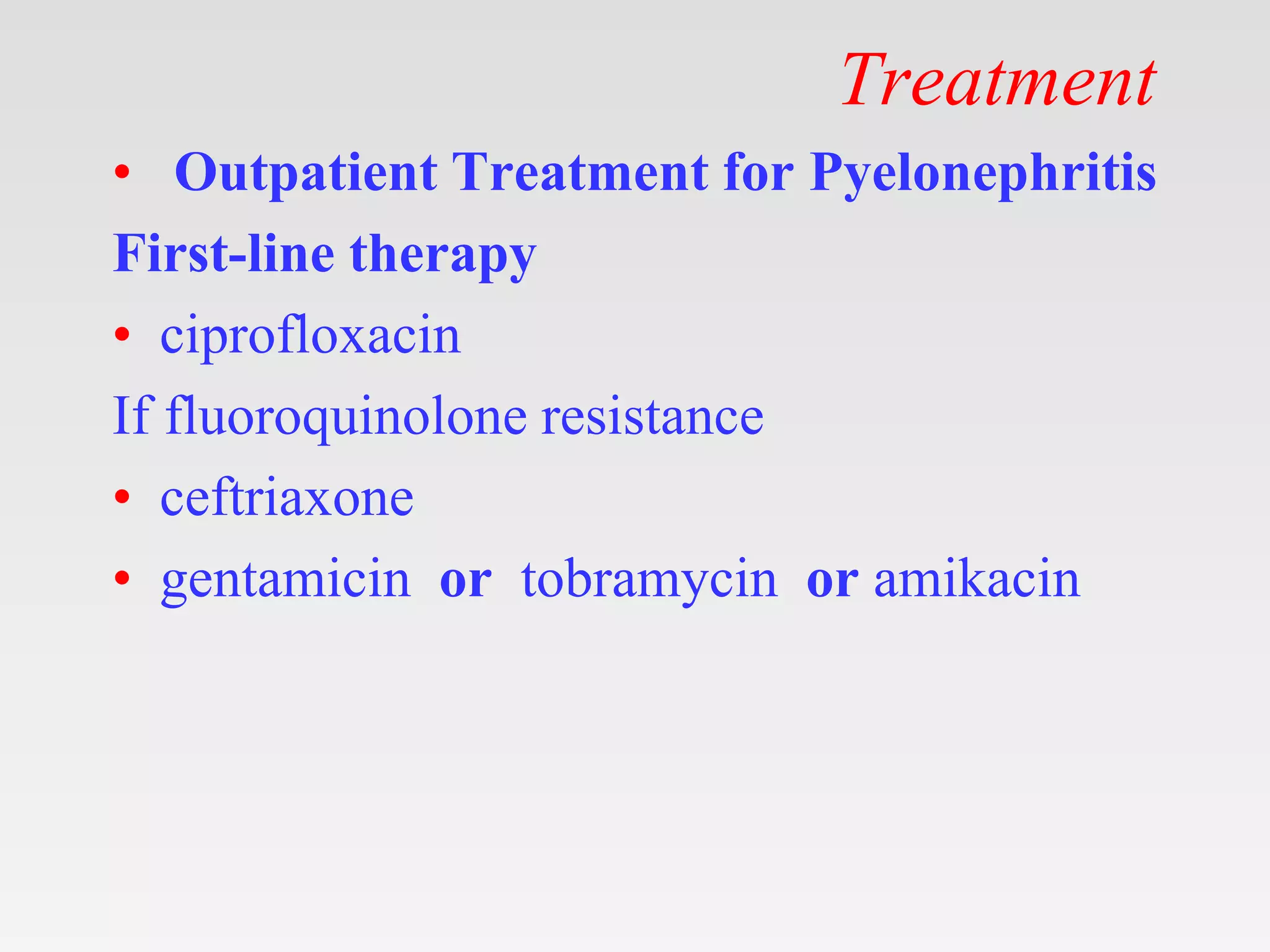
4. Diagnosis involves urinalysis, urine culture, blood tests and imaging. Treatment is usually antibiotics selected based on likely causative organisms.