The document provides an overview of acute viral hepatitis, including:
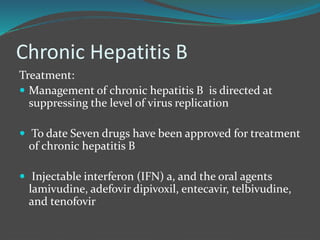
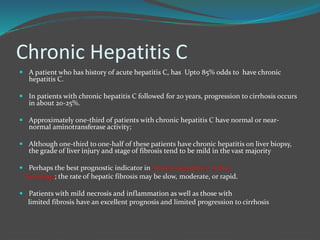
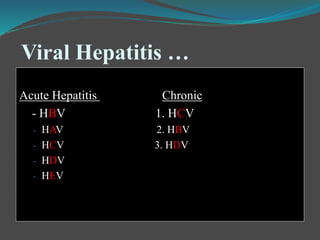
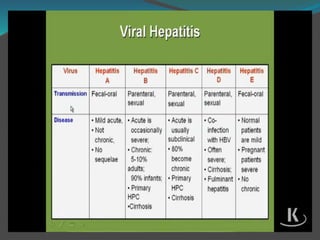
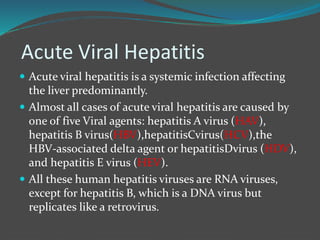
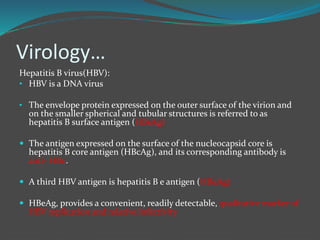
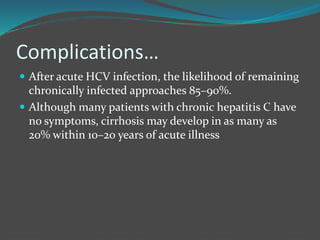
1) It is caused by five main viruses - HAV, HBV, HCV, HDV, HEV. HBV and HCV often cause chronic infections leading to cirrhosis and liver cancer, which contributed to over 1 million deaths in 2015.
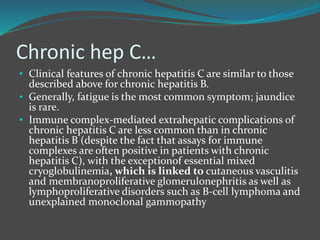
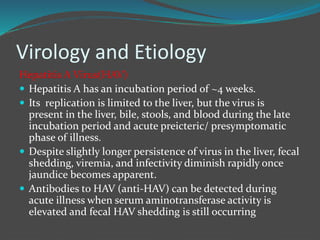
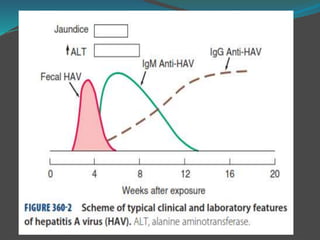
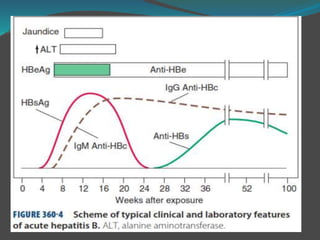
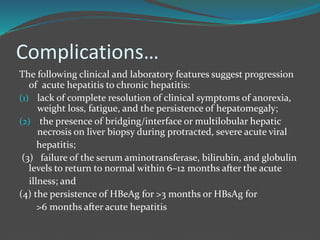
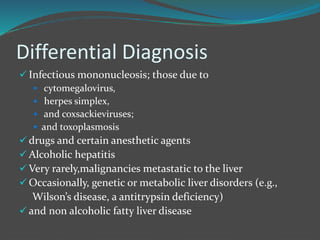
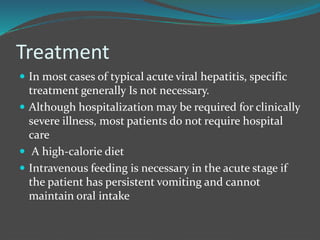
2) The viruses have varying incubation periods and methods of transmission. Clinical features include nausea, vomiting and jaundice. Laboratory tests show elevated liver enzymes and bilirubin. Fulminant hepatitis is a rare but serious complication.
3) Prognosis is generally good for HAV and HEV, but chronic infections can develop for HBV, HCV and HDV,
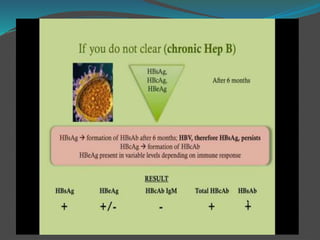
![Chronic…
Lab…
In severe cases, moderate elevations in serum bilirubin
[3-10 mg/dL]) occur.
Hypoalbuminemia and prolongation of the
prothrombin time occur in severe or end-stage cases.
Hyperglobulinemia and detectable circulating
autoantibodies are distinctly absent in chronic
hepatitisB (in contrast to autoimmune hepatitis)](https://image.slidesharecdn.com/viralhepatitismele-190531011937/85/Viral-hepatitis-55-320.jpg)