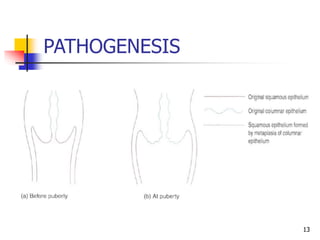
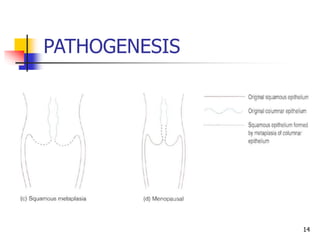
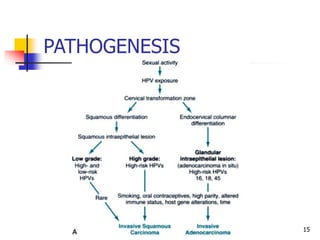
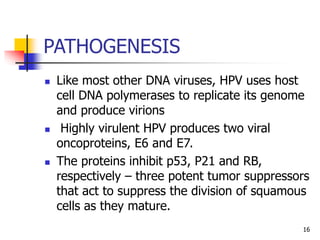
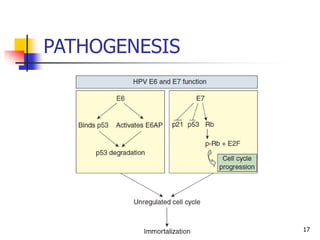
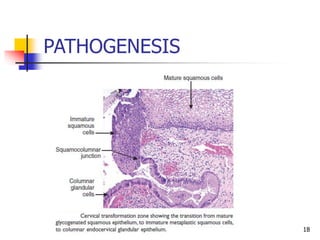
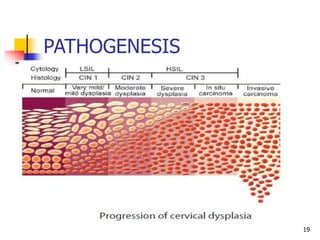
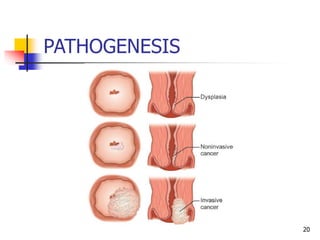
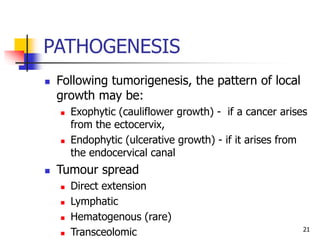
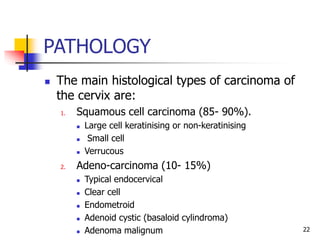
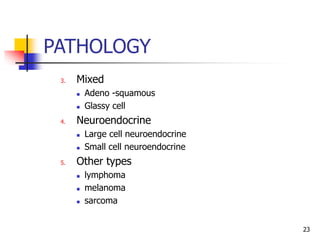
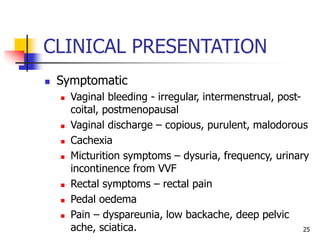
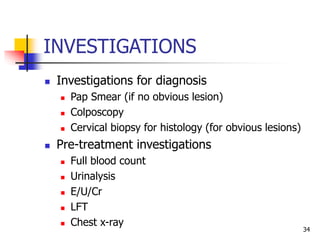
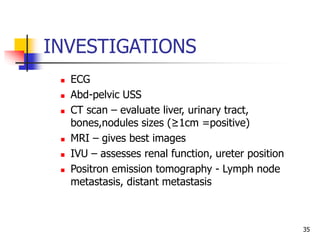
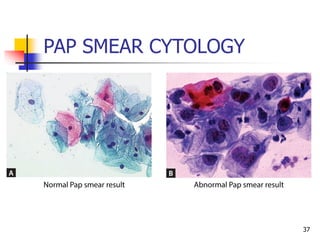
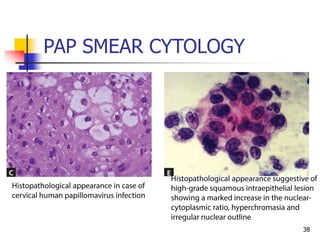
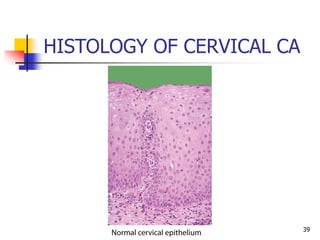
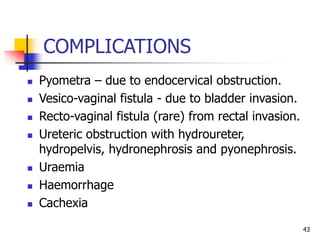
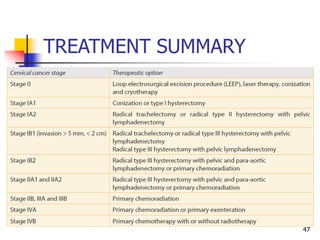
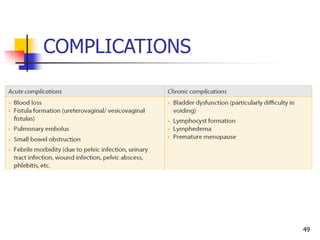
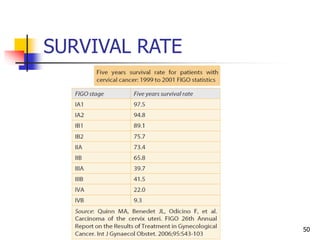
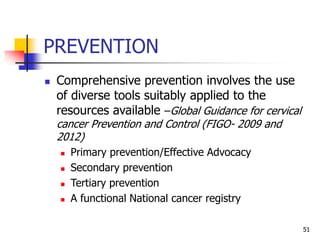
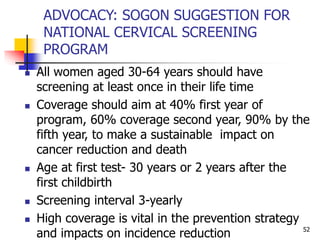
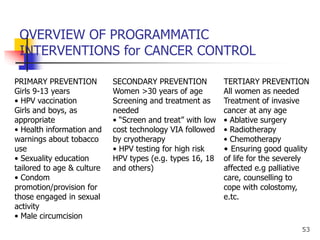
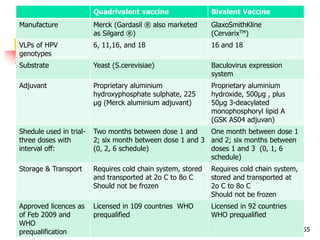
The document discusses cervical cancer, including its epidemiology, risk factors, pathogenesis, clinical presentation, investigations, complications, treatment, and prevention. Cervical cancer is caused by human papillomavirus (HPV) and is the most common gynecologic cancer in women globally. Screening through Pap smear testing and HPV DNA testing can detect pre-cancerous lesions early and reduce cervical cancer incidence and mortality rates. Prevention involves HPV vaccination, screening programs, and sexual health education and advocacy.




![RESOURCES
6. Kumar V, Abbas AK, Aster JC. Robbins Basic Pathology E-Book.
Elsevier Health Sciences. 2017 Mar 8.
7. Saxena R. Bedside Obstetrics & Gynecology. JP Medical Ltd;
2014 Mar 20.
8. Bruni L, Barrionuevo-Rosas L, Albero G, Serrano B, Mena M,
Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO/IARC
Information Centre on HPV and Cancer (HPV Information
Centre). Human Papillomavirus and Related Diseases in
Nigeria. Summary Report 27 July 2017. [Accessed 20th April,
2018]
9. Etedafe PG. Cervical cancer: Advances in prevention.
Presentation for Part one update course in Obstetrics and
Gynaecology. 2014.
60](https://image.slidesharecdn.com/cervicalcancer-180424165212/85/Cervical-cancer-60-320.jpg)