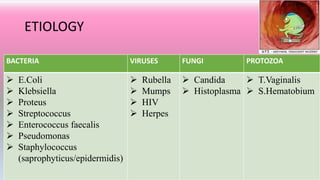
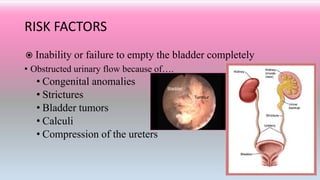
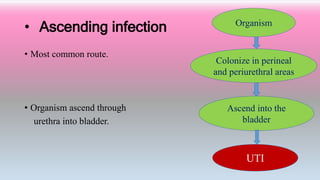
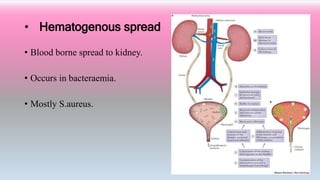
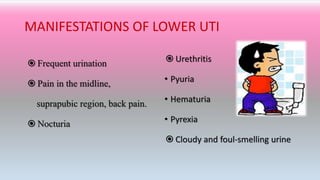
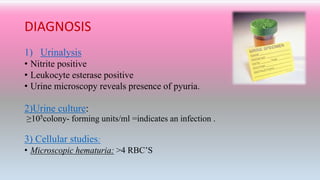
An 40 year old woman presented with complaints of painful urination, urgency, lower back pain and burning urination. Urine culture showed 105 colony-forming units/ml of bacteria. She was treated with an antibiotic (Trimethoprim–sulfamethoxazole) twice daily for 3 days and pain medication, which reduced her symptoms. Urinary tract infections are common and occur when bacteria or other microbes infect the urethra, bladder, ureters, or kidneys. Symptoms include painful urination and back pain. Diagnosis involves a urine test and culture. Treatment is usually a short course of antibiotics along with pain medication and hydration.