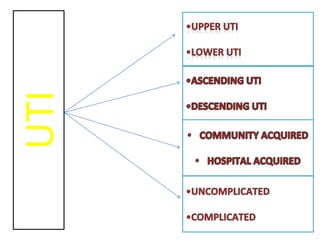
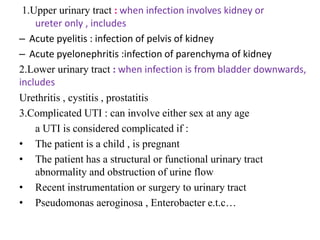
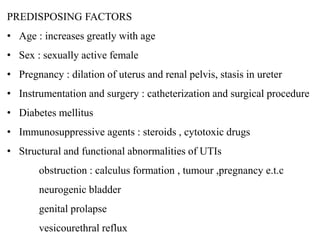
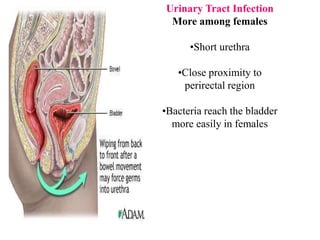
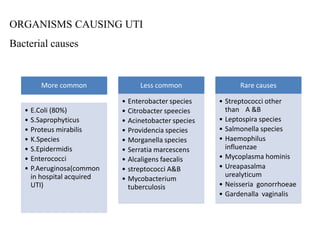
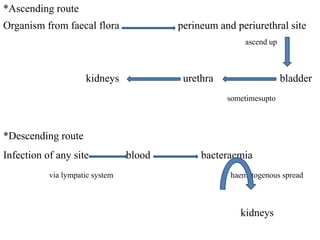
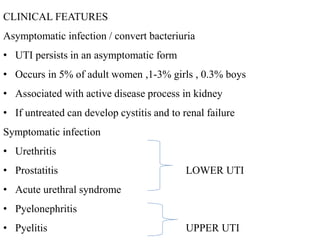
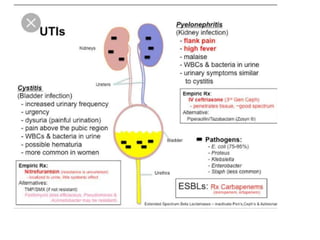
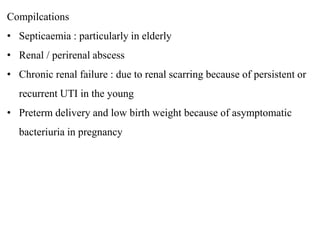
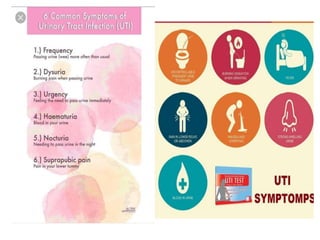
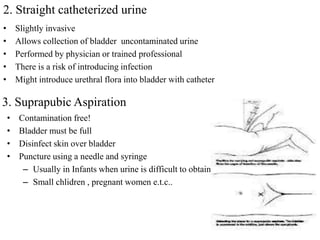
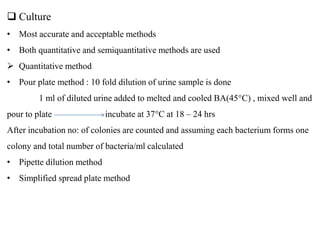
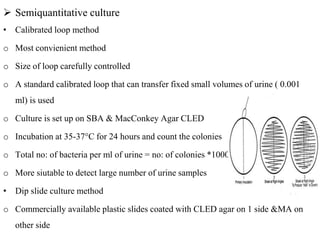
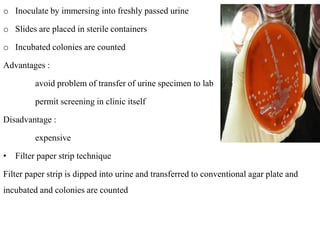
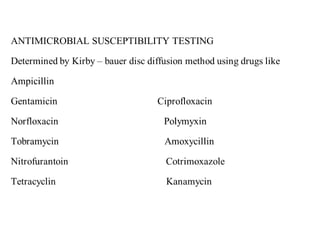
This document defines and describes urinary tract infections (UTIs). It discusses the types of UTIs including upper and lower tract infections. It outlines predisposing factors like age, sex, pregnancy, and structural abnormalities. It describes the typical organisms that cause UTIs like E. coli. The document discusses pathogenesis, clinical features, complications, and laboratory diagnosis of UTIs including specimen collection and screening tests. Culture remains the most accurate diagnostic method.