The document summarizes anatomy and injuries related to the urinary bladder, urethra, and prostate. It discusses the following:
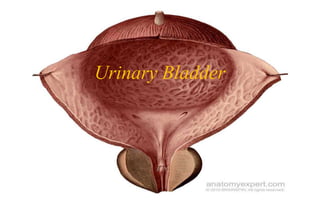
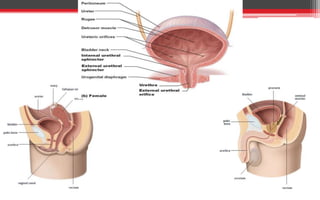
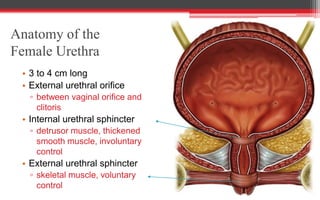
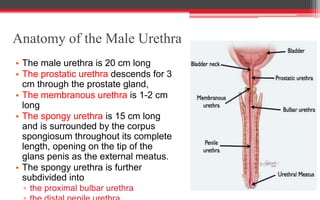
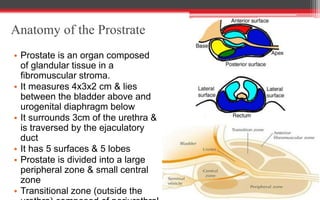
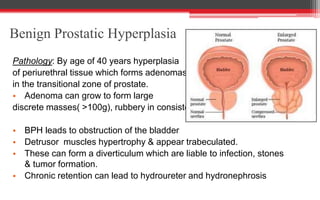
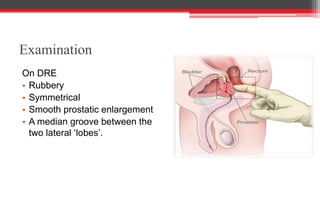
1) The anatomy of the bladder, urethra, and prostate. The bladder stores urine and is lined with transitional epithelium. The urethra carries urine from the bladder. The prostate surrounds the urethra in males.
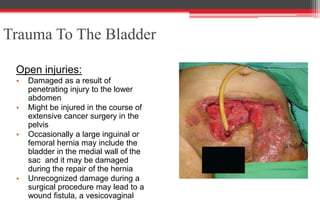
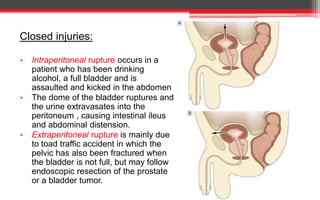
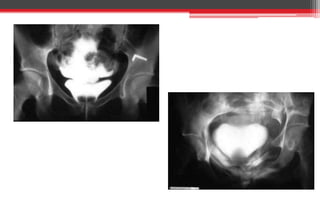
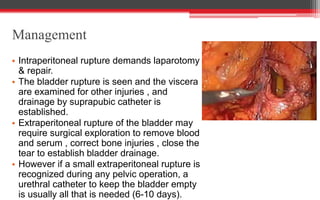
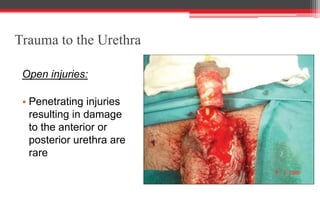
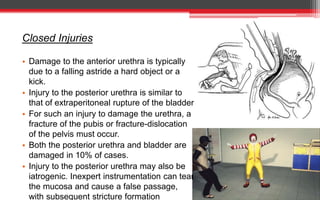
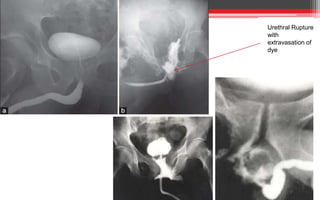
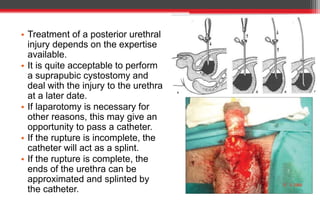
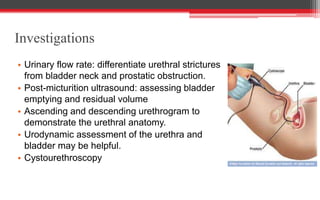
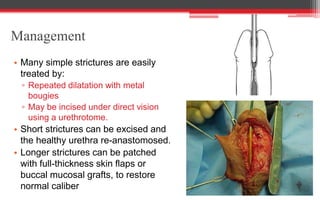
2) Common injuries to these structures including open injuries from trauma and closed injuries from blunt force. Signs, investigations, and management are described for different injuries.
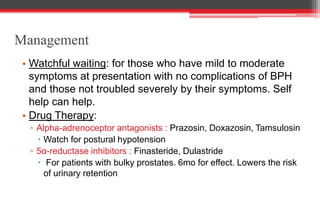
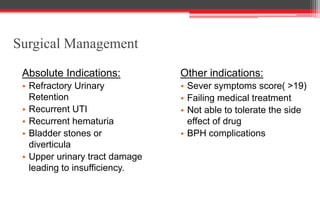
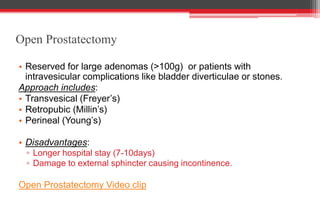
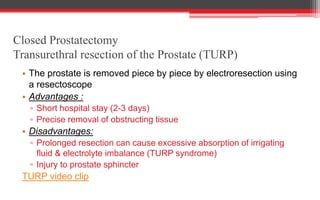
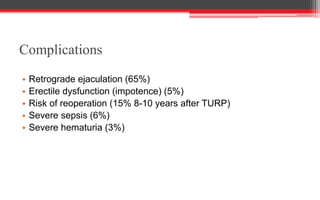
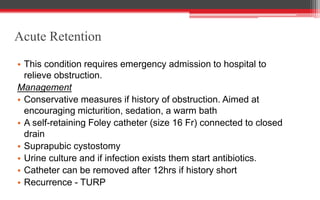
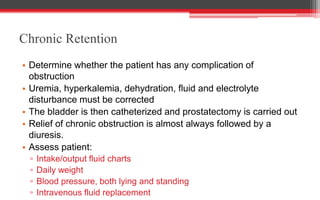
3) Conditions like benign prostatic hyperplasia which can cause obstruction. Medical and surgical treatment options for conditions affecting the bladder, urethra