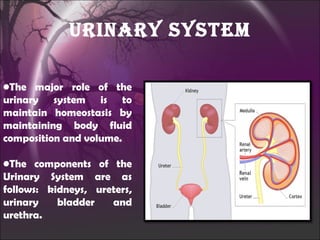
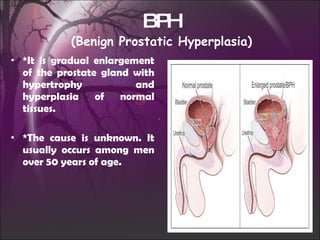
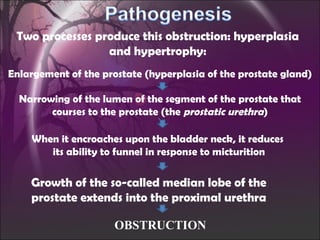
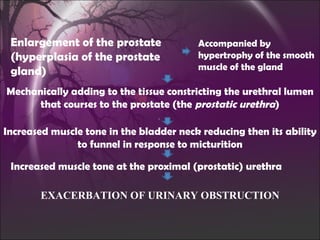
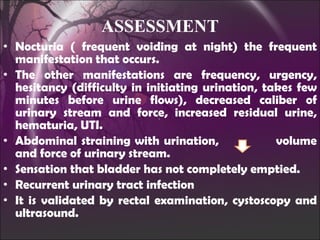
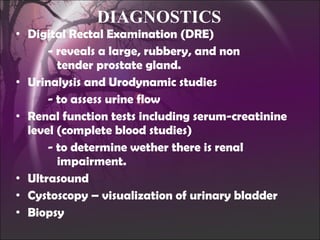
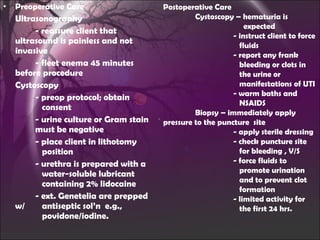
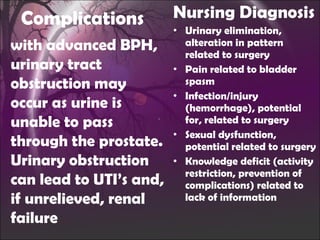
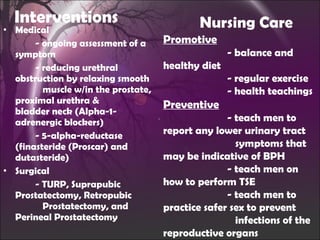
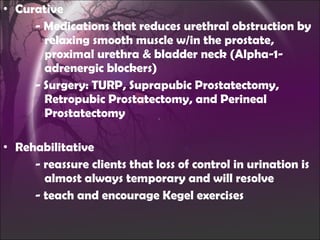
The document discusses benign prostatic hyperplasia (BPH), its causes, symptoms, and treatments. BPH involves the gradual enlargement of the prostate gland due to hormonal imbalances in aging males. This causes compression of the urethra and urinary obstruction, which can lead to complications like urinary tract infections and renal failure if left untreated. Diagnostic tests and treatments include medications to reduce obstruction and surgical procedures like TURP.