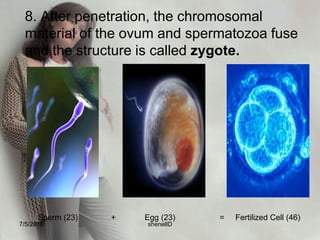
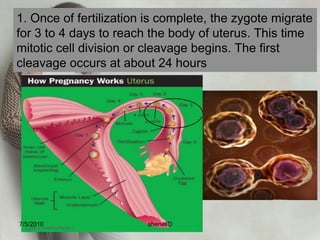
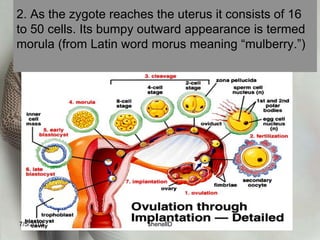
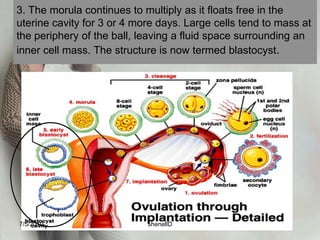
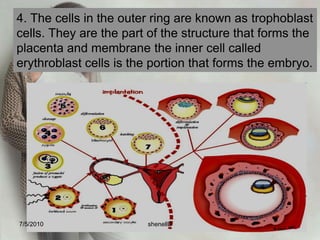
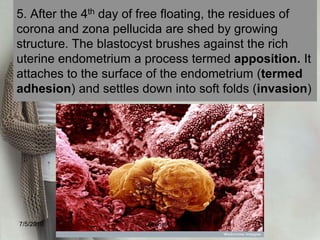
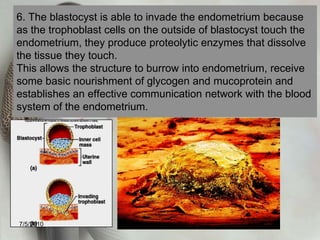
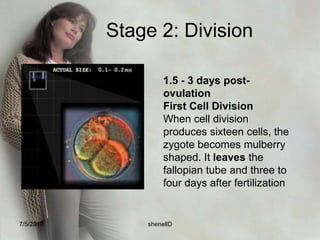
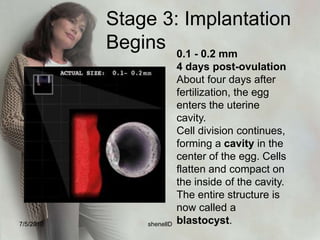
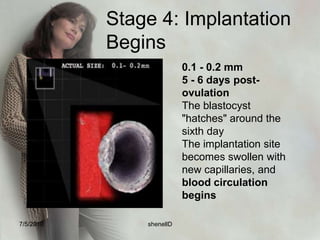
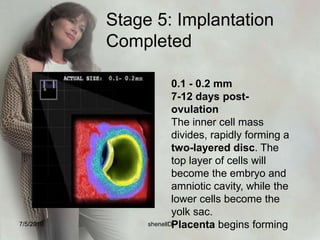
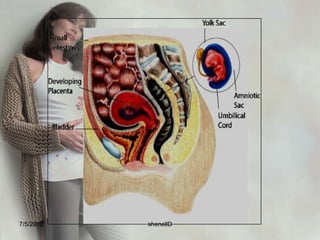
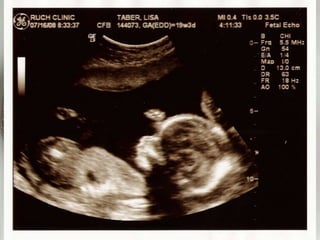
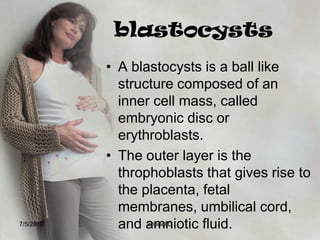
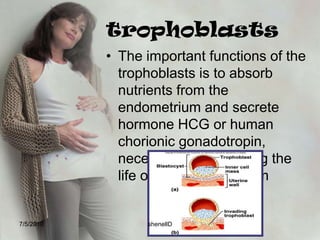
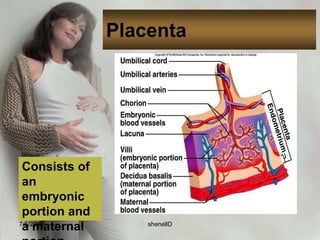
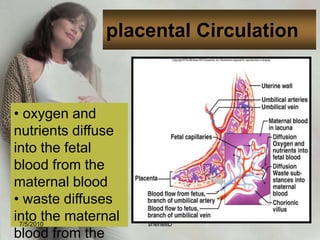
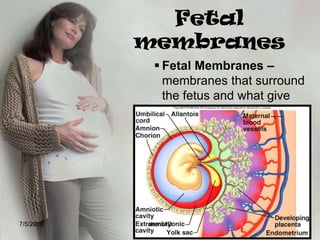
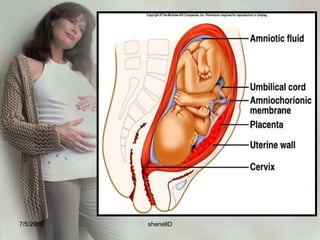
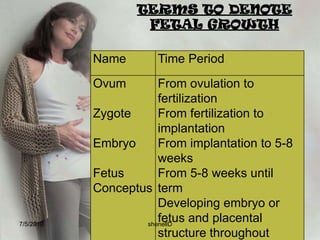
Fertilization occurs when an egg and sperm fuse, forming a zygote. The zygote undergoes cell division and develops into a blastocyst, which implants in the uterine lining. The blastocyst develops an inner cell mass that forms the embryo and outer trophoblast cells that form the placenta. The placenta functions to exchange gases, nutrients, and waste between the mother and developing fetus.