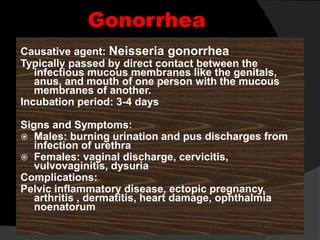
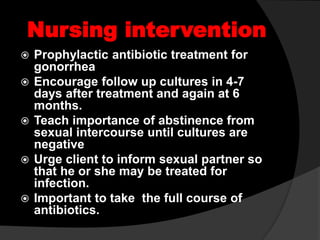
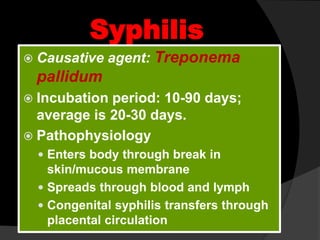
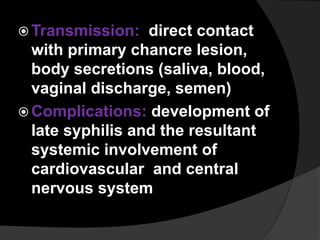
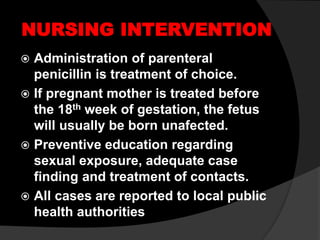
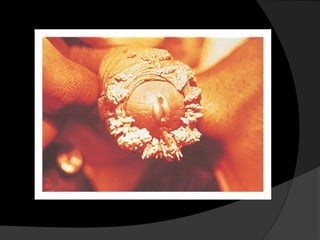
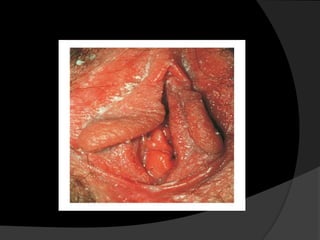
This document discusses sexually transmitted infections (STIs), including their causes, symptoms, transmission, treatment and prevention. It covers common STIs like chlamydia, gonorrhea, herpes, HPV, syphilis and trichomoniasis. It also addresses vaginal inflammatory conditions like bacterial vaginosis and candidiasis. The key points are that STIs are often passed through unprotected sex; have a variety of symptoms; and can be treated with antibiotics or other medications, with prevention through education and barrier methods.