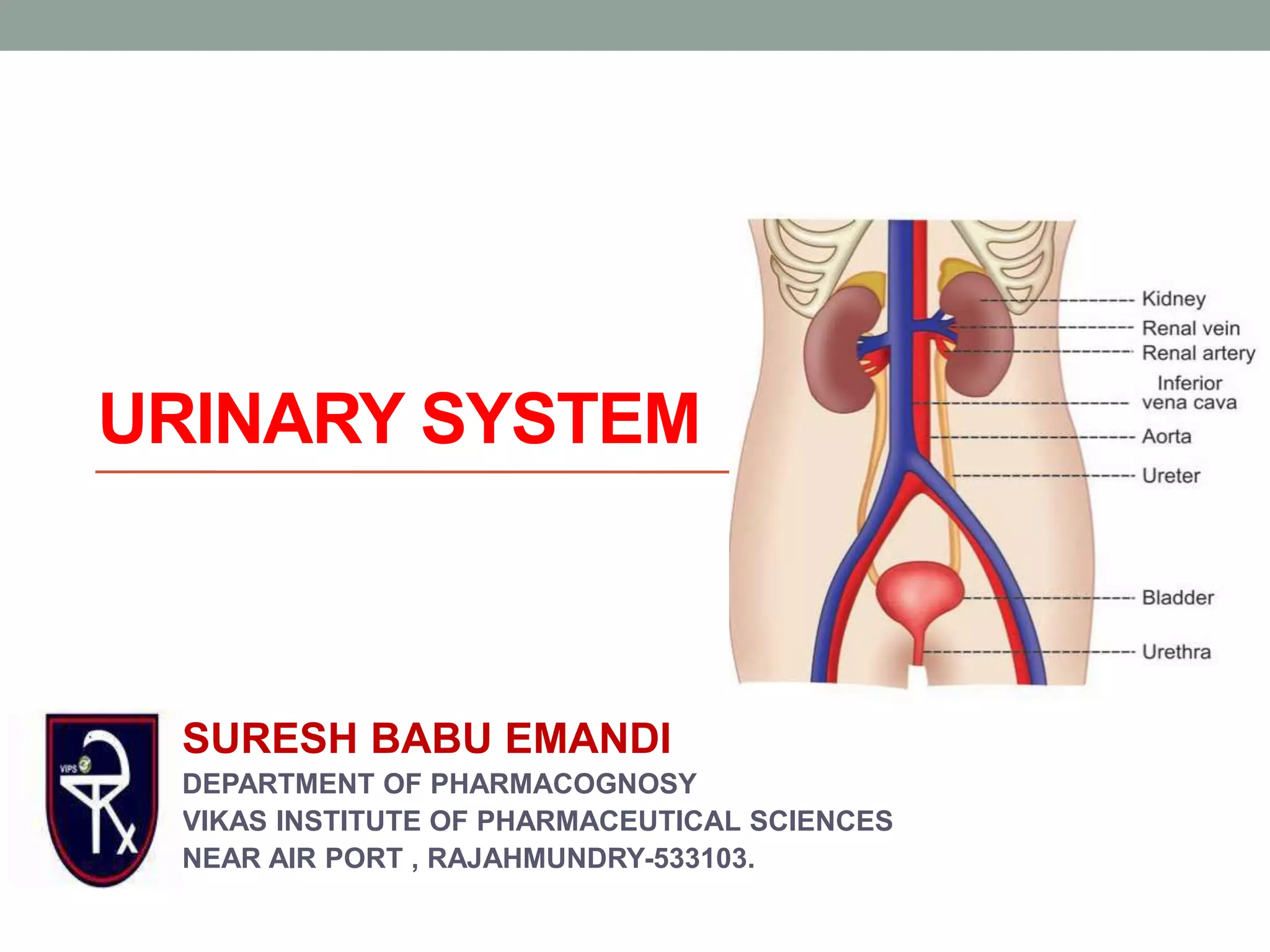
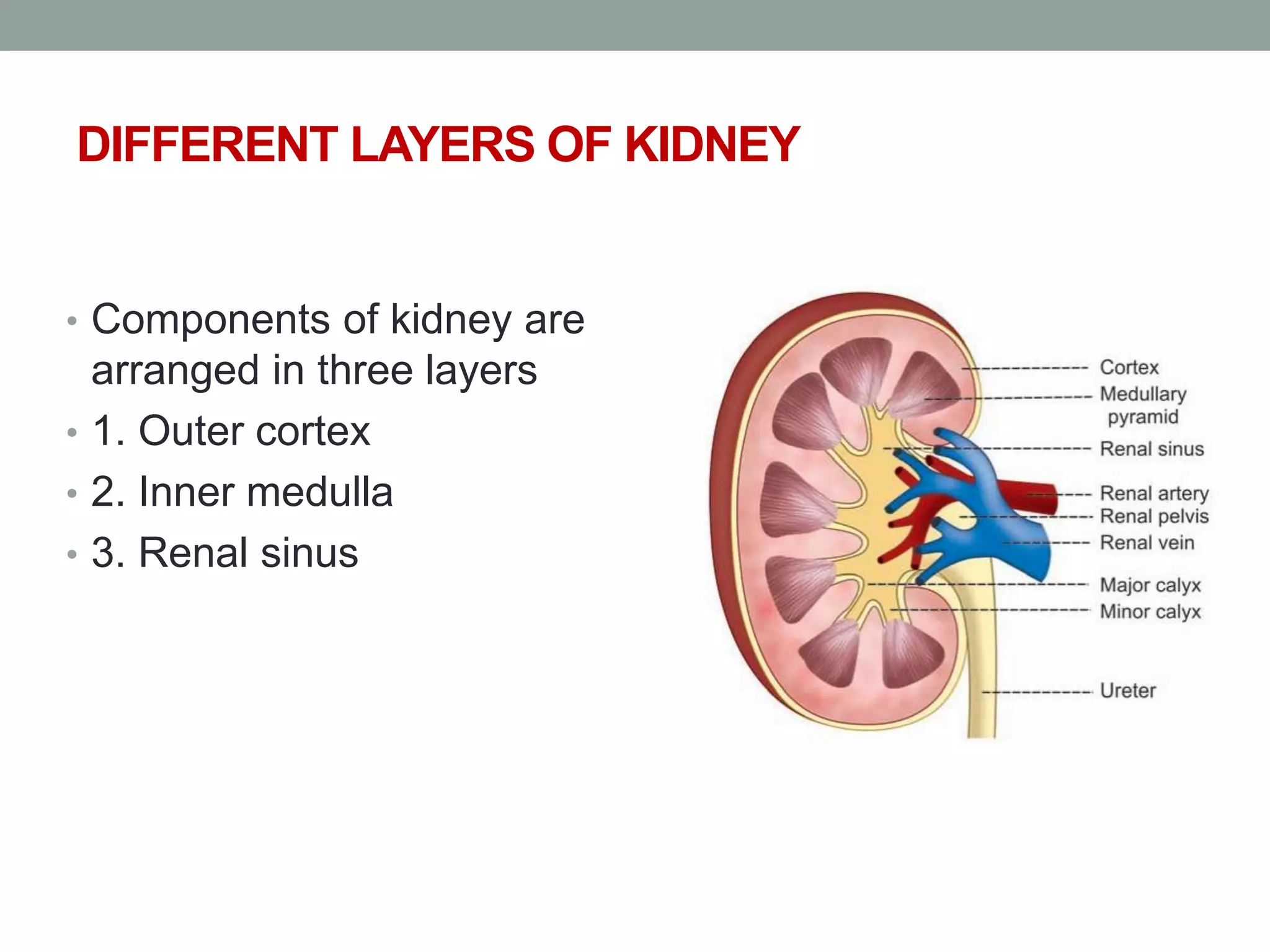
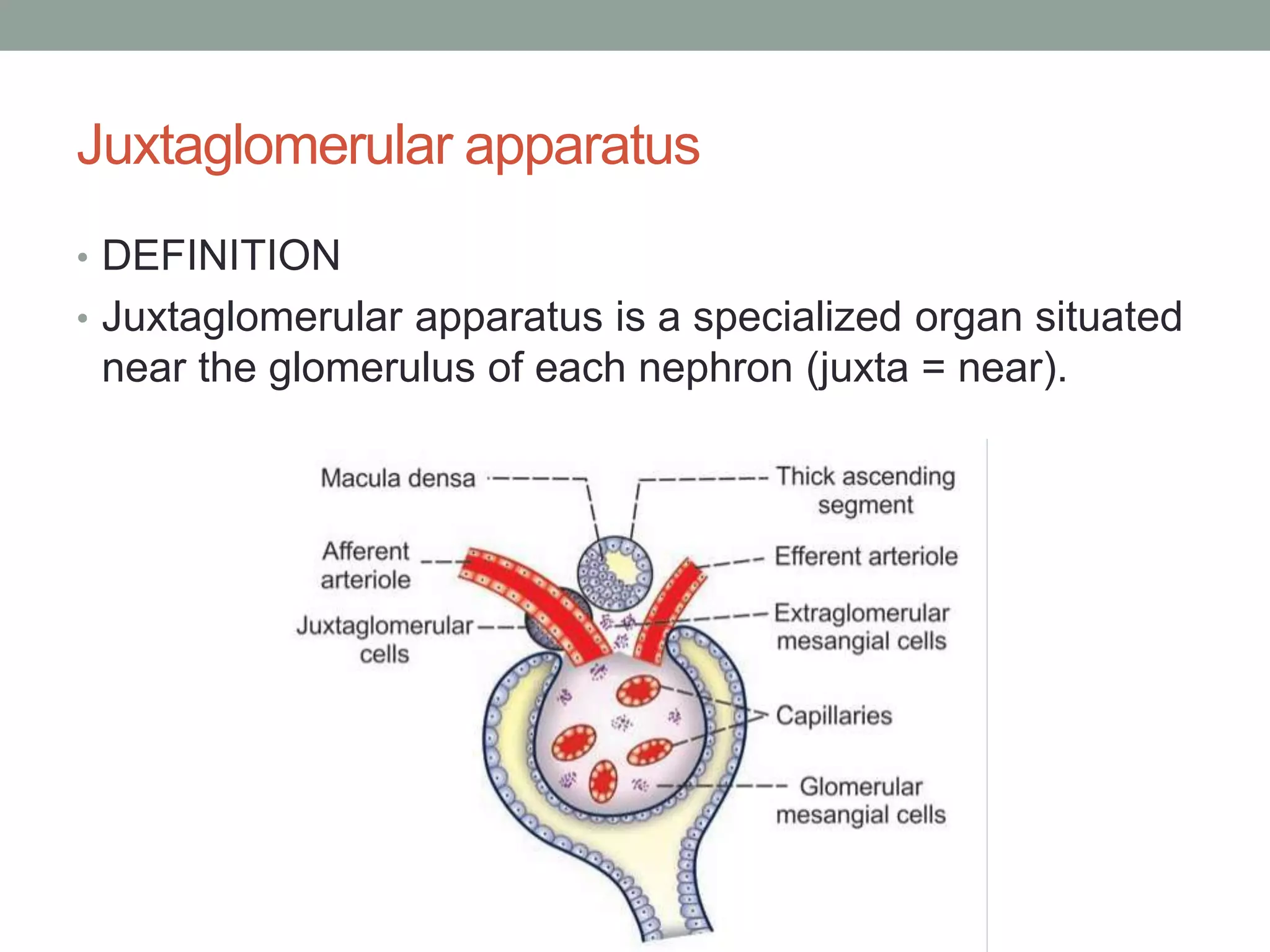
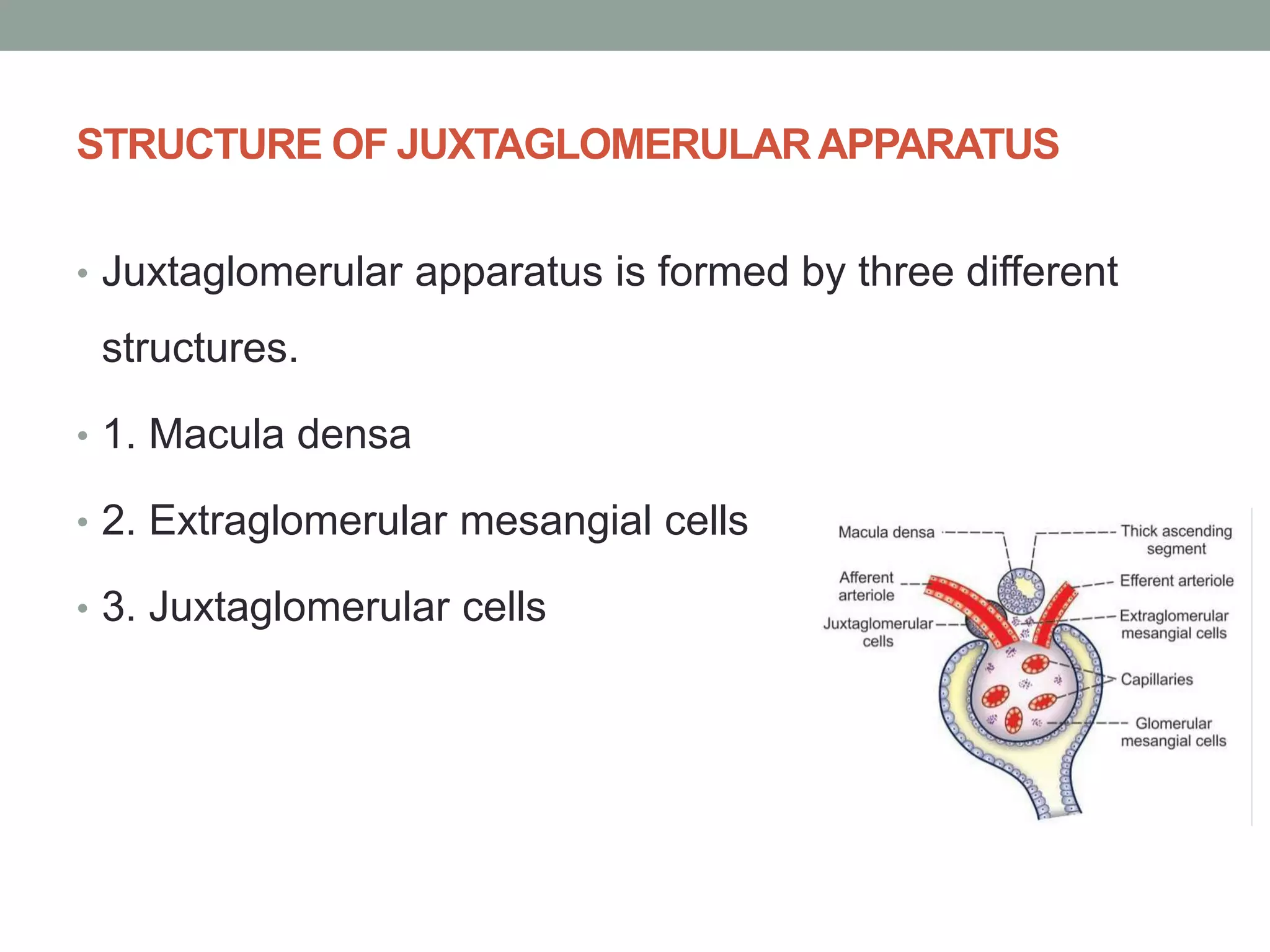
The urinary system, primarily involving the kidneys, plays a crucial role in the excretion of metabolic wastes, maintenance of homeostasis, and regulation of fluid and electrolyte balance. Key components include the filtration process in nephrons, the production of urine, and the secretion of hormones such as erythropoietin and renin. The document details the anatomy and function of various structures within the renal system, emphasizing their importance in maintaining body health.